Notes »
disease
Acute Lymphoblastic Leukaemia
Overview
Overview Acute Lymphoblastic Leukaemia (ALL) is a malignancy of lymphoid cells. The two main ALL is T-cells ALL and B-cells ALL. In ALL there is uncontrolled proliferation of immature lymphoblasts in the bone marrow leading to overcrowding affecting other cell lineage. It is the commonest cancer in childhood, rare in adults and has a strong associated with Down's Syndrome.
| Definition Leukaemia: Group of malignant disorder, affecting the blood forming tissue of the bone marrow lymph system and spleen Acute lymphoblastic leukaemia: Most common leukaemia affecting children. Characterised by lymphoblasts in peripheral blood smear (lower cytoplasmic-nucleus ratio) Acute Myeloid leukaemia: More common in young adults, adults. Characterised by the development of immature myeloblasts in the bone marrow. Down's Syndrome: Trisomy 21, a genetic disorder. Children with Down syndrome (DS) have an increased risk of B-cell precursor acute lymphoblastic leukemia. |
| SUMMARY OF MAJOR LEUKAEMIA | ||
| Subtype | Description | Typical Group affects |
| Acute lymphoblastic leukaemia | Blast cells on peripheral blood smear or bone marrow aspirate | Children (53% <20yo) |
| Acute Myelogenous leukaemia | Blast cells on peripheral blood smear or bone marrow aspirate; Auer rods on peripheral smear, Myeloperoxidase positive | Adults |
| Chronic lymphoblastic leukaemia | Clonal expansion of at least 5,000 B lymphocytes per μL (5.0 × 109 per L) in the peripheral blood | Older adults (85% >65yo) |
| Chronic Myelogenous leukaemia | Philadelphia chromosome (BCR-ABL1fusion gene) | Adults |
Haematopoesis
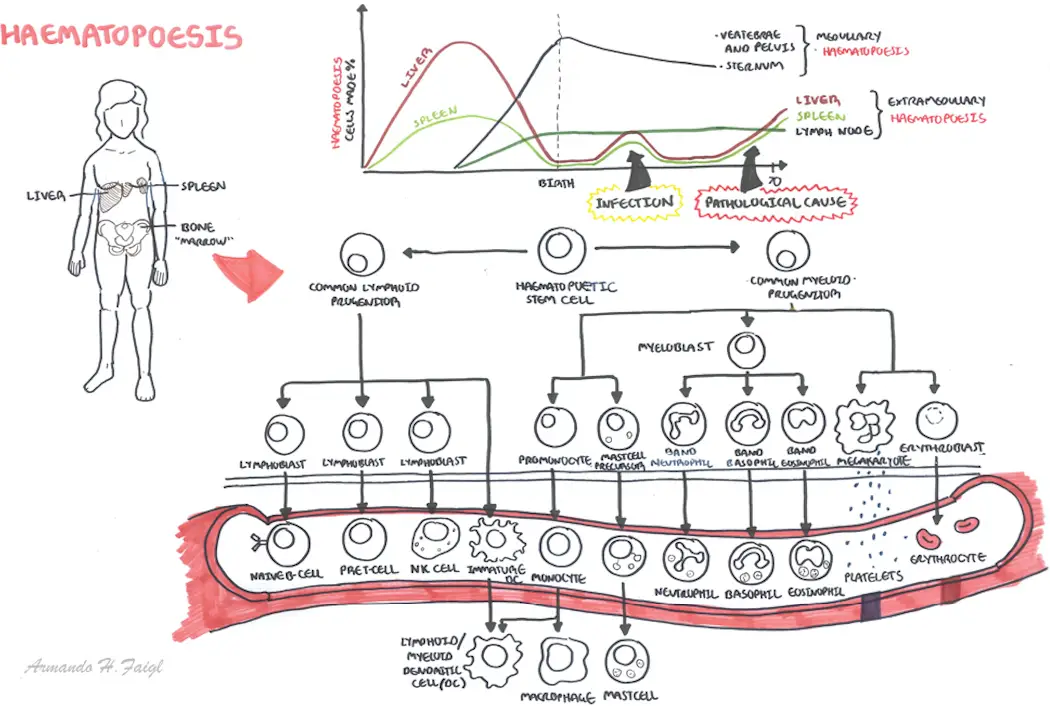
| Watch Video Haemtopoesis |
Classification
ALL is classified based on 3 things:
- Morphology - divided into L1, L2, L3 based on microscopic appearence (nucleus, vesicles)
- Immunological markers - differentiate B and T cell ALL as both have different sets of CD markers
- Cytogenetics - Chromosomal analysis, looks at mutations in genes which gives a prognostic value.
- Good prognosis
- Poor prognosis - Philadelphia chromosome
| Philadelphia chromosome is a balanced translocation between chromosome 9 and 22 which leads to the formation of the BCR/ABL fusion gene. This chromosome is seen mainly in Chronic myeloid leukaemia and sometime in ALL. In ALL it signifies a poorer prognosis |
Risk Factors
- Radiation
- Chemicals - Benzene
- Infection - human T-cell lymphoma/leukemia virus-1 (HTLV-1)
- Inherited syndromes
- Down syndrome
- Klinefelter syndrome
- Fanconi anemia
- Bloom syndrome
- Ataxia-telangiectasia
- Neurofibromatosis
- Race/ethnicity - more commone in african americans
| PROGNOSIS FEATURES IN CHILDHOOD ALL | ||
| Risk Factors | Favourable | Unfavourable |
| Age | 1-10yo | <1 or >10 yo |
| Gender | Female | Male |
| Race/ethnicity | Caucasian, Asian | Black, Hispanic |
| White blood cell count | <50000/ul | >50000/ul |
| Immunophenotype | B-precursor | T cell, Mature B cell |
| Genetic features | Hyperdiploidy, Translocation (12:21) | Philadelphia gene (9:22), Hypodiploidy |
| Extramedullary involvement | No | Yes |
Signs and Symptoms
Initial presentation
- Fever
- Anorexia
- Fatigue
- Bone and joint pain especially lower extremities
Bone marrow Failure
- Anaemia
- Infections
- Bleeding, brusing
- Fatigue
Infiltration (extramedullary haemtopoesis)
- Hepatomegaly
- Splenomegaly
- Lymphadenopathy
- Superficial or mediastinal
- Orchidomegaly
- CNS involvement - Cranial nerve palsy
Differential Diagnosis
- Acute Myelogenous Leukemia (AML)
- B-Cell Lymphoma
- High-Grade Malignant Immunoblastic Lymphoma
- Mantle Cell Lymphoma
- Non-Hodgkin Lymphoma
Investigations
- Full Blood Count - ↓Hb, thrombocytopaenia
- Blood Smear - reveals lymphoblasts
- Chest X-ray and CT scan - check for chest involvement
- Lumbar puncture - check for CNS involvement
Management
Chemotherapy Program
- Remission Induction - destroys 99% of "cancerous" cells
- Consolidation - destroys further 99% of "cancerous" cells
- CNS and Orchid prophylaxis - IV or intrathecal methotrexate
- Maintenance - continuation of chemo up to 2 years - destroys remaining 99% of "cancerous" cells just to be sure
| Side note Haemotological remission means no presence of lymphoblasts on peripheral blood smear, normal bloods and <5% blasts in regenerating bone marrow |
Complications and Prognosis
Complications
- Pancytopaenia
- Febrile neutropenia
- Pneumocystis carinii pneumonia and other infections
- Tumour lysis syndrome
- Chemotherapy adverse effects
- Gastrointestinal
- Alopecia (hair problem)
- CNS toxicity
- Avascular necrosis
- Vincristine-related neuropathy
- Relapse (increased ICP or isolated cranial nerve involvement)
| Remember Patient with cancer with recent chemotherapy (white cell count significantly down) spikes serious fever give antibiotic - Tazocin |
Prognosis
- Good in children. Adults not as good
Acute Lymphoblastic Leukaemia and Acute Myeloid leukaemia
| DIFFERENCES BETWEEN ACUTE MYELOID LYMPHOBLASTIC LEUKAEMIA | ||
| Acute Myeloid Leukaemia | Acute Lymphoblastic Leukaemia | |
| Blast size on blood smear | Medium to large, uniform | Variable small to medium |
| Cytoplasm | Fine granules maybe present | Usualyl scant, a few coarse granules may be seen (morphology L3 - eosinophilic like) |
| Auer rods | Present | Absent |
| Nuclear chromatin | Finely Dispersed | Fine to corase |
| Genetic markers | Myeloid peroxidase present (only found in myeloid cells) | TDT marker present (only found in lymphoblasts) |