Overview
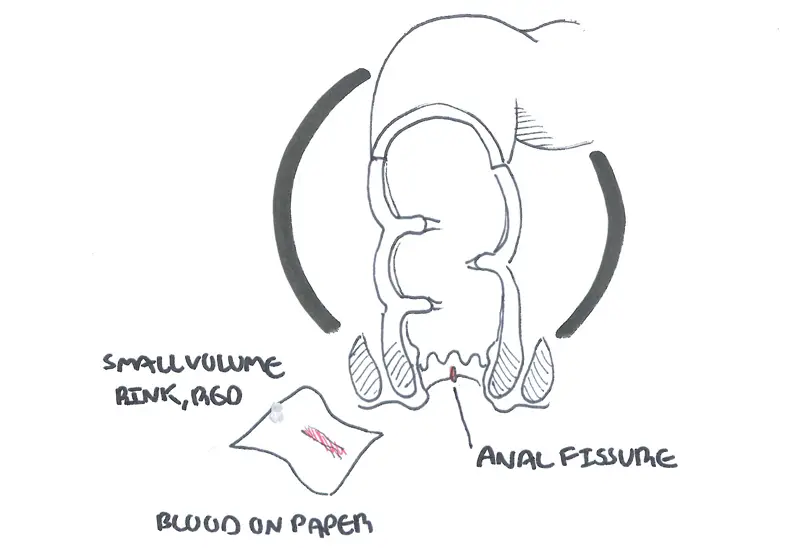
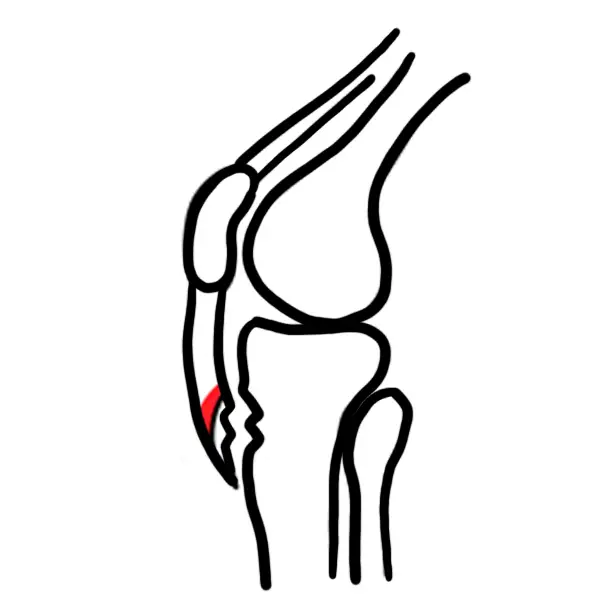
Overview Anal fissure is one of the most common lesions to consider in differential diagnosis of anal pain. Think about them as vertical ulcers usually occurring in the posterior midline of the skin just outside the entry to the rectum. Its persistence is due to spasm of the internal sphincter muscle. It can be associated with Crohn's disease. It typically causes episodic pain that occurs during defecation and for one to two hours afterwards. Anal fissures usually occur in the anterior or posterior parts of the anus and underlies the internal anal sphincter.
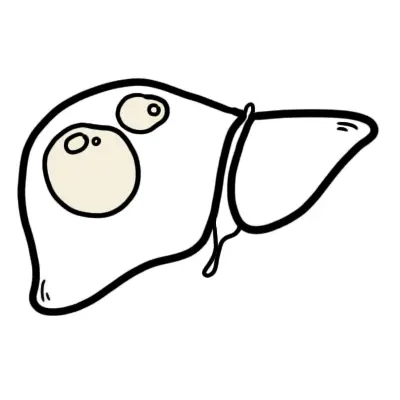
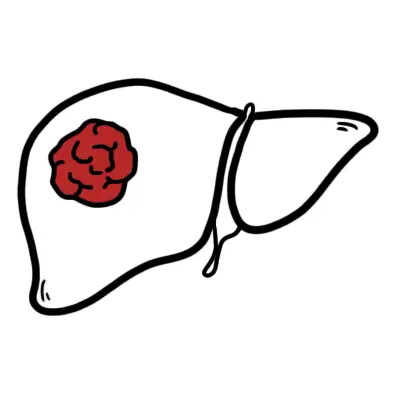
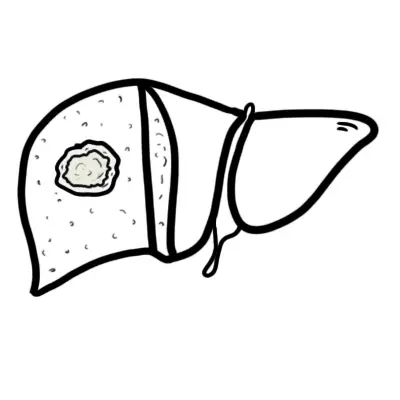
| Definition Anal Fissure: A superficial linear tear in the anoderm distal to the pectinate line (dentate line) commonly caused by passage of hard stool Fistula in ano: abnormal communication between the anorectal lining and perineal or vaginal epithelium. Nearly always associated with anal abscess Perianal abscess: Abscess within the soft tissues surrounding the anal canal Anal haemorrhoids: Dilation of haemorrhoids plexus either internal or external. |
Anorectal Anatomy
Anal Sphincters
- Internal sphincter
- Continuation of the circular fibers of the colon. Thus, the internal sphincter is under autonomic control (Autonomic nervous system)
- Involuntary control
- Surrounds upper 3/4 of anal canal
- External sphincter
- Voluntary control
- Surrounds entire length of anal canal
- Consists of three parts - subcutaneous, superficial and deep
Intersphincteric Plane
- Between the external sphincter muscle laterally and the longitudinal muscle (inner sphincteric muscle) medially
- Contains anal glands
- The plance can be opened up surgically to provide access for operations on the sphincter muscles
Anal glands
- Apocrine glands
- Glands are occasionally infected and acts as a source of anal fistula
Pectinate line (dentate line)
- Muco-cutaneous junction of anal canal
- Divides anal canal into upper and lower lowers which differ in
- Blood supply
- Lymph drainage
- Nerve supply
- Corresponds with position of anal valves
- Situated at the middle of internal sphincter
| PECTINATE LINE (DENTATE LINE) | ||
| Distinction | Above Pectinate line | Below Pectinate line |
| Embryological origin | Endoderm | Ectoderm |
| Epithelium | Colomnar epithelium | Stratified squamous epithelium |
| Lymph drainage | Internal iliac lymph node | Superficial inguinal lymph nodes |
| Artery | Superior rectal artery | Middle and inferior rectal arteries |
| Veins | Superior rectal veins | Middle and inferior rectal veins |
| Innervation | Inferior hypogastric plexus | Inferior rectal nerve |
| Haemorrhoids | Internal haemorrhoids | External haemorrhoids |
| Hilton's Line also called while line/anocutaneous line indicates lower end of the internal sphincter. Ischiorectal abscess when communicates with anal canal usually opens at or below Hilton's line. |
Risk Factors
- Low intake of dietary fiber
- Massive shits
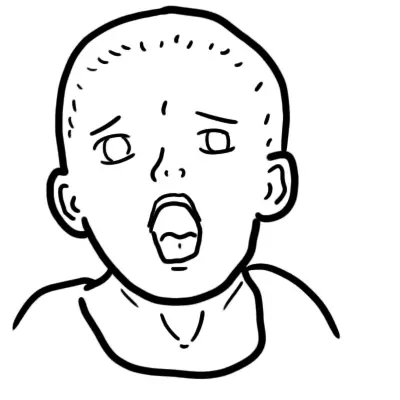
Signs and Symptoms
Clinical Presentation
- Severe pain, patient does not want to go to the toilet
- Stabbing pain during defection
- Deep throbbing pain
- Anal pain during and for one to two hours after defecation - distinguishing feature to other anal pain differentials
- Bleeding in toilet paper
| Side note Acute fissures typically heal with medical management after 4 to 6 weeks, chronic fissures persist beyond 6 weeks. |
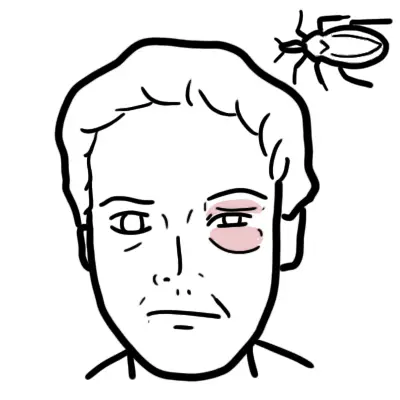
Examination - Location of fissure
- Posteriorly midline (90~%)
- Anterior midline (~10% more common in women)
- Anywhere else - Fissures located off the midline suggest the presence of underlying pathology such as anal cancer, Crohn's disease or syphilis.
- OFTEN TO PAINFUL TO PERFORM PER RECTAL EXAMINATION!
Differential Diagnosis
- Haemorrhoid
- Anal fistula
- Rectal ulcer
Secondary anal fissures (pathological causes)
- Crohn's disease
- Tuberculosis
- Sarcoidosis
- HIV
- Syphilis
| Side note Fissure that do not occur midline are possibly due to an underlying pathology. Often there fissure are multiple |
Investigations
Not usually indicated, unless diagnosis uncertain or secondary fissure suspected.
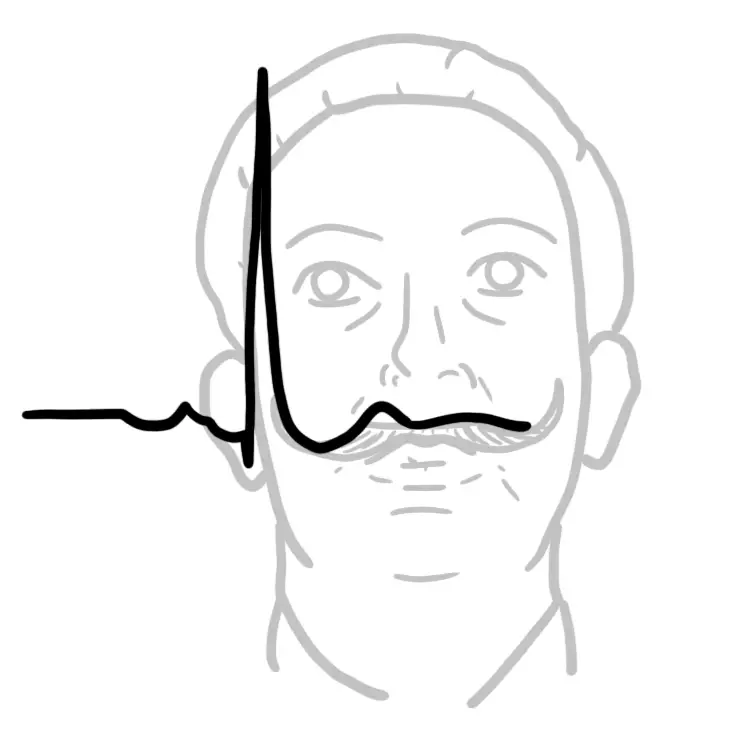
Pathophysiology
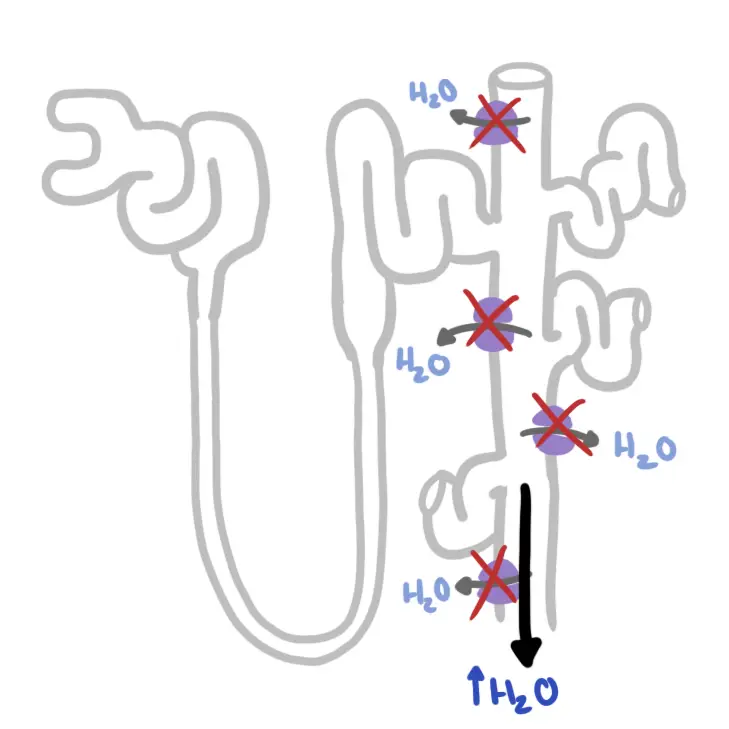
Anal fissures usually occur in the anterior or posterior parts of the anus and underlies the internal anal sphincter. Muscles spasm are due to contraction of the internal anal sphincter causing ischaemia → pain
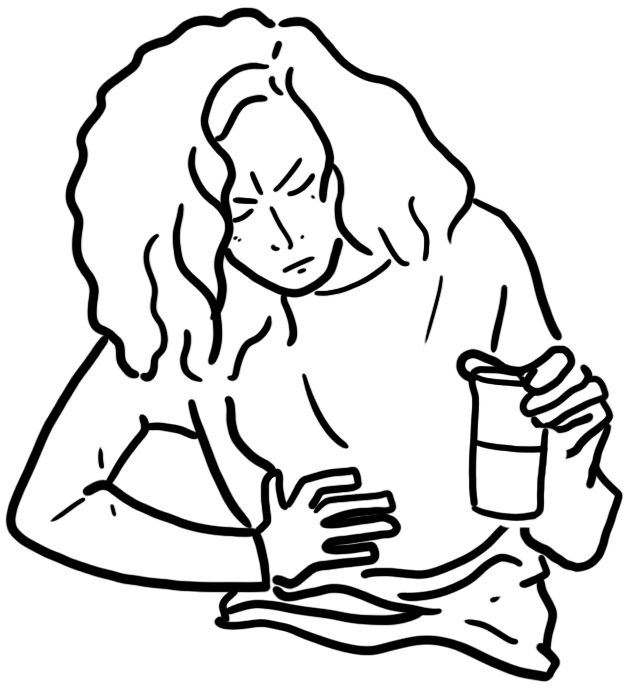
Management
- Conservative management
- Increase fibre intake
- Sitz bath
- Topical GTN
- Botulinum toxin (BOTOX)
- Sphincterotomy
| Pharmacology GTN (common medication for angina). Mechanism of action is by activting guanylyl cyclase increasing cGMP causing smooth muscle relaxation reducing muscle spasms in the perianal area. Side effects of topical GTN: headaches |
Complications
- Faecal incontinence due to sphincterotomy