Overview
- Aortic valve stenosis is characterised by obstruction of left ventricular outflow, resulting in inadequate cardiac output, decreased exercise capacity, heart failure, and death from cardiovascular causes.
- Mild to moderate aortic stenosis is usually a symptomatic, but occasionally can be found on routine examination
- Locations of stenosis - Valvular (common), supravalvular and subvalvular
- Aortic Stenosis produces a "Mid Systolic Murmur", which is a murmur heard between the first heart sound (S1 - AV valve closure) and ends before the second heart sound (S2 - Aortic and Pulmonary valve closure)
- Most common valvular heart disease in western countries and prevalence increase with increasing age
Cardiac valves
The heart has 4 valves:
- Aortic valve
- Pulmonary valve
- Tricuspid valve
- Mitral valve (bicuspid valve)
The Mitral and tricuspid valves are atrioventricular valves meaning they allow blood to move from the atrium to the ventricles of the heart. This occurs with ventricular diastole.
The aortic and pulmonary valve are tricuspid valves which when open allow blood to move to the aorta and pulmonary system respectively. This occurs during ventricular systole when the heart contracts.
All of the heart valves except the mitral valve are usually tricuspid. However, there can be congenital bicuspid valves which can predispose one to valvular disease later on. The heart valves can be heard most prominent in the following regions of the chest
- Aortic valve - Right 2nd intercostal space parasternal
- Pulmonary valve - Left 2nd intercostal space parasternal
- Tricuspid valve - Left 4th intercostal space parasternal
- Mitral valve - Left 5 intercostal space mid-clavicular (below the nipple)
Risk factors
- Age >60
- Congenitally unicuspid, bicuspid valve
- Rheumatic heart disease
- Chronic Kidney Disease
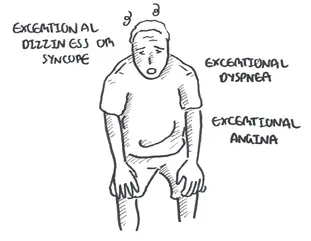
Signs and symptoms
Cardiovascular Examination
- Slow rate of rise in carotid pulse (parvus and tardus)
- Auscultation - Aortic Valve (right second intercostal space parasternal)
- Ejection systolic murmur - Mid to late peak intensity of the murmur generally begins after S1 and ends before S2 (mid systolic murmur)
- Reduced intensity of S2, closing of the aortic valve
- Atrial contraction, S4, maybe heard
- Auscultation - Apex (Left fifth intercostal space mid-clavicular)
- Murmur may radiate to apex of heart
- High frequency and louder murmur (Holosystolic murmur) can be confused with mitral regurgitation (Gallavardin phenomenon)
Cardiac Examination findings include parvus and tardus of the carotid artery and mid-systolic ejection murmur heard over the left second intercostal space parasternal. Murmur can radiate to the carotids.
Signs of severity
- Parvus et tardus
- Aortic thrill
- Length, harshness and lateness of the peak of the systolic murmur
- Atrial contraction, S4
- Parodical splitting of the second heart sound (delayed left ventricular ejection and aortic valve closure)
- Left ventricular failure
| Think Squatting increases venous return and accentuate the murmur |
| Side note - Clinical Auscultation | ||
| Murmur | Heart Sound | |
| Mitral Stenosis | High pitched early-diastolic murmur | Loud S1 |
| Mitral Regurgitation | Pansystolic murmur radiates to the axilla | Soft S1 loud S2 |
| Aortic stenosis | Ejection systolic "crescendo decresendo" murmur radiating to the carotids | Soft S2 |
| Aortic regurgitation | early diastolic murmur | Soft S2 |
Differential Diagnosis
Differential Diagnosis include other causes of mid-systolic murmurs
- Mitral valve dysfunction
- Hypertrophic cardiomyopathy
- Aortic sclerosis
- Atrial septal defect
- Pulmonary stenosis
Investigations
- Transthoracic echocardiogram - elevated aortic pressure
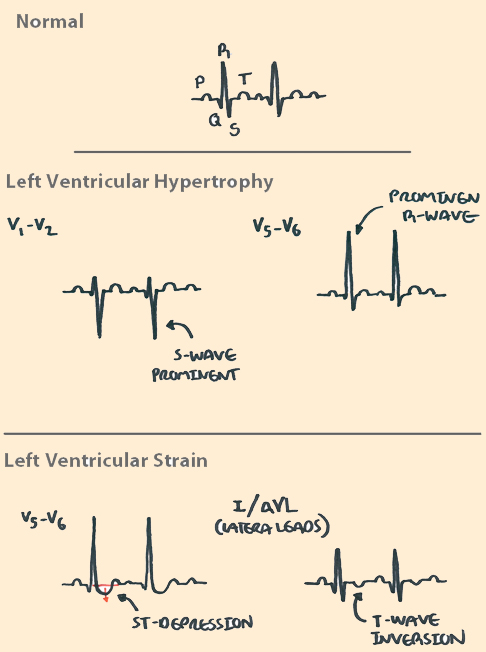
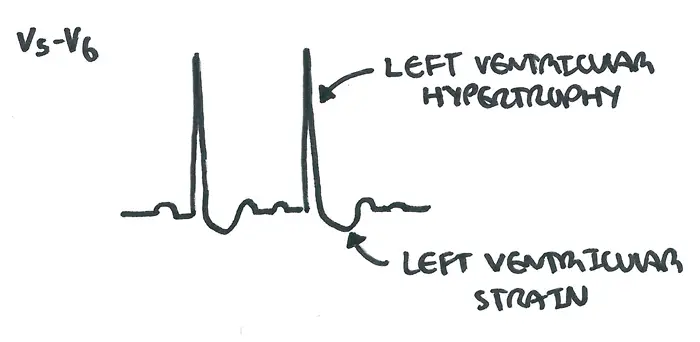
- ECG - left ventricular hypertrophy and absent Q wave
- X-ray - valve calcification
- Cardiac MRI
- Cardiac catheterisation - allows for direct measurement of the pressure gradient
Diagnosis
- Echocardiography is the primary test in diagnosis and evaluation of aortic stenosis
- 50% stenosis of aortic valve
Aetiology
- A congenitally abnormal valve (bicuspid or rarely unicuspid) with superimposed calcification
- Calcific disease of a trileaflet valve
- Age related
- Typically in patients >65years
- Rheumatic valve disease
- Congenital aortic stenosis (rare)
- congenital stenosis - abnormal valve is present from birth
- acquired stenosis - abonrmal calve beomes stenotic overtime
Pathophysiology
The natural history of AS begins with a prolonged asymptomatic period.
Pathology
- Calcified, stiff aortic valve leaflets
- Calcification and dilation of the ascending aorta
- Left ventricular hypertrophy
- Possible left atrial enlargement
- Mitral annular calcification -> mitral regurgitation
Management
| Indications for surgery |
| Symptomatic |
| Critical obstruction based on catheterisatin |
- Long term anticoagulant (following valve replacement)
- Long term antibiotic prophylaxis
- Balloon valvuloplasty (for inoperable patients)
- 80% re-stenosis in 1 year
- ~14% develop mild/moderate reguritation
- Transcatheter aortic valve replacement (for inoperable patients)
- Surgical aortic valve replacement
- mechanical
- bioprosthetic
Emergency (unstable)
- Surgical aortic valve replacement
- Transcatheter aortic valve replacement
Complication and Prognosis
Complication
- Sudden Cardiac Death
- Arrythmias
- Endocarditis
- Bleeding tendency
- Systemic Embolism
Prognosis Mortality in patients with AS dramatically increases after the development of cardiac symptoms. The rate of death is 50% at 2 years for patients with symptomatic disease unless aortic valve replacement is performed promptly.