Cervical Cancer
Cervical cancer is an HPV-related malignancy of the uterine cervical mucosa. Most cervical tumours contain HPV DNA (99.7%) . There are many variants of HPV, HPV-16 and 18 are the 2 most common high-risk types. Cervical cancer is proceeded by an idenifiable precursor lesion (cervical intraepithelial neoplasia (CIN1)) that may progress to invasive cancer. CIN can be easily detected by an inexpensive and noninvasive screening test (Pap smear). Pap smears has been hailed as one of the most successful preventative medical strategies. Cervical cancer is the second most common cancer in women.
Cervix: Cylinder-shaped neck of tissue that connects the vagina and uterus.
Transitional zone of the cervix: Dynamic entity formed during puberty and, histologically, is the area where the glandular epithelium is being replaced by squamous epithelium
Squamo–Columnar Junction (SCJ): Point at which columnar and squamous epithelium meet at the cervix.
Pap Smear: Screening tool where samples cells are taken from the junction of the ectocervix and endocervix (the transformation zone or squamocolumnar junction, where 90% of cervicalneoplasias originate) to identify pre-malignant or malignant lesions
High Risk HPV: Also known as oncogenic HPV types (most commonly 16 and 18) are the most common causes of invasive cervical cancers and 50% of high grade lesions
LLETZ: Large loop excision of the transformation zone is a procedure to remove cervical tissue for examination and to treat some precancerous changes of the cervix.
Epidemiology
Cytology (Pap smear) – screening
Rarer:
There are approximately 200 different types of HPV, which are classified according to DNA sequence. Between 40–50 HPV types specifically infect the anogenital area and, less commonly, the oro-pharyngeal area. These genital HPV types are divided into ‘low risk’ and ‘high risk’ according to their association with, and ability to cause, anogenital cancer.
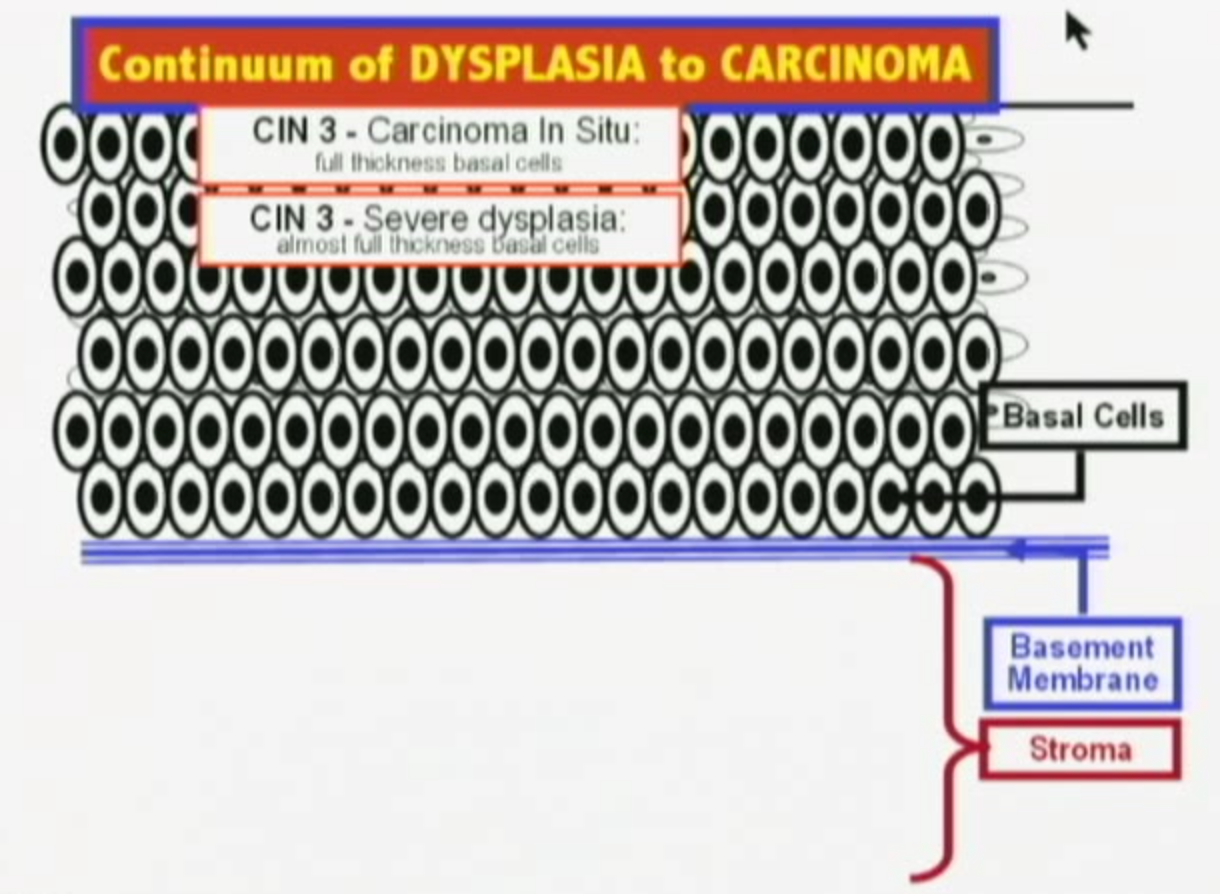
Development of cervical cancer
There are four main steps for the development of cervical cancer:
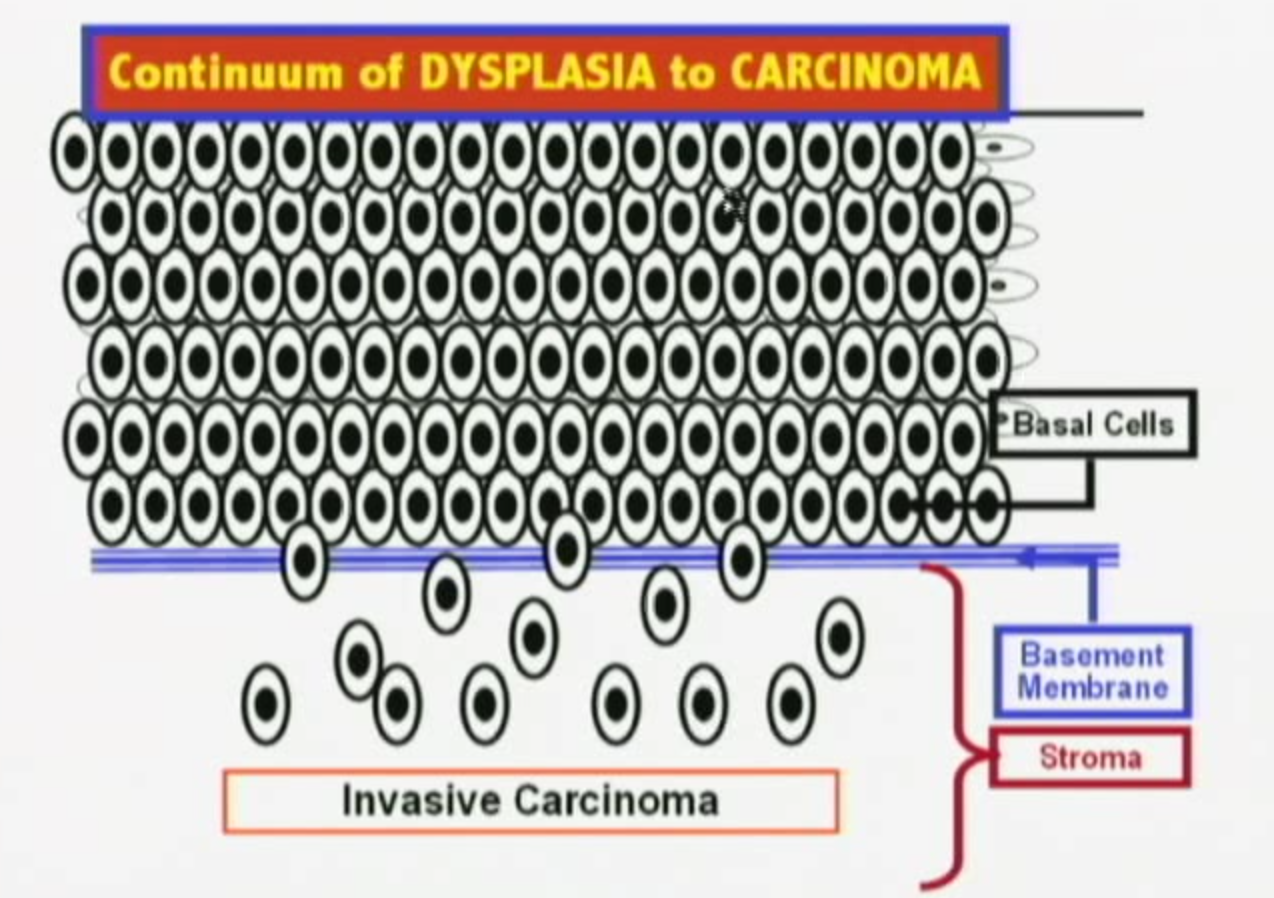
ROUTES OF SPREAD — Cervical cancer can spread by direct extension or by lymphatic or hematogenous dissemination.
Early stage disease is frequently asymptomatic. Pre-invasive lesions are often found only after abnormal routine screening Pap smear. Abnormal vaginal bleeding is the most common presenting symptom of invasive cervical cancer, and in sexually active women, postcoital spotting is common. Mean age of developing cervical cancer is 50yo.
Flank tenderness or leg swelling indicate advanced cervical cancer.
Investigations A cervical biopsy and not pap smear is the best diagnostic test to evaluate a cervical mass. A Pap smear is a screening test and appropriate for a woman with a normal- appearing cervix.
Diagnosis Cervical biopsy is the most important investigation in diagnosing cervical cancer. Cervical cancer is a clinically staged disease
Cervical cancer is a clinically staged disease.
Compare pap smear and biopsy. They should correlate with each other. If biopsy not significant but pap smear significant further investigation is warranted (cone biopsy).
| FIGO (International Federation of Gynecology and Obstetrics) staging of cervical cancer | |
| Stage | Description |
| I | Confined to the cervix (uterine spread not evaluated) |
| II | Cancer invades beyond the cervix but not to the pelvic sidewall, or the distal third of the vagina |
| III | Tumour affixed to pelvic sidewall, or involving the lower third of the vagina, or is associated with a non-functioning kidney or hydronephrosis |
| IV | Carcinoma has extended out of the pelvis, involving the bladder, or rectum. |
Overview
| MANAGEMENT OVERVIEW | ||||
| Biopsy | Observation | Ablation | Excision | Hysterectomy |
| CIN1 | + | + | + | |
| CIN2/CIN3 | + | + | +/- | |
| Cancer | + | |||
Microinvasive Disease (Stage I)
Early Stage Disease (Stage I-II)
Locally Advanced Disease (Stage II-IV)
Metastatic disease (Stage IV)
Most recurrences of endometrial cancer occur within 2 years.
Prognosis The 5-year survival depends on the stage of the tumour:
Vaccination
Vaccination against human papillomavirus (HPV) is recommended due to the link between cervical HPV infection and the development of cervical dysplasia.
Pap smear
Cervical cancer screening (Pap Smear) is very effective. It has been associated with a 70% reduction in cervical cancer mortality in developed countries. The Pap smear samples cells from the junction of the ectocervix and endocervix (the transformation zone or squamocolumnar junction, where 90% of cervicalneoplasias originate) to identify pre-malignant or malignant lesions
In Australia pap test screening is recommended every 2 years for women who have ever had sex and have an intact cervix, commencing from age 18–20 years (or up to 2 years after first having sexual intercourse, whichever is later).
Results can be as follows:
The most common histologic types of cervical cancer are squamous cell (85% of cervical cancers) and adenocarcinoma (10%).
Adenosquamous tumors exhibit both glandular and squamous differentiation. They may be associated with a poorer outcome than squamous cell cancers or adenocarcinomas.
BestPractice
UpToDate
Petignat, P., & Roy, R. (2007). Diagnosis and Management of cervical cancer. The BMJ. 335 (765).
Stella, H. (2014). HPV testing in the National Cervical Screening Program. RACGP. 42 (7). 463-466.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion