Overview
Overview Hypothyroidism is a clinical state resulting from underproduction of the thyroid hormones T4 and T3. Most cases (95%) are due to primary hypothyroidism, a failure of the thyroid gland to produce thyroid hormones. Autoimmune thyroiditis (Hashimoto's disease) is the most common cause of primary hypothyroidism. It affects women much more than men. In the developing world, iodine deficiency is a major cause of hypothyroidism. Drugs that can cause hypothyroidism include lithium and amiodarone. Six percent of post-partum women develop lymphocytic thyroiditis, which causes transient primary hypothyroidism.
| Remember Primary hypothyroidism is decreased production of thyroid hormones because of thyroid gland disease (most common is hashimoto's thyroiditis). Secondary hypothyroidism is a problem in the Pituitary gland or hypothalamus resulting in ↓TSH leading to ↓Thyroid hormone production. |
Anatomy and Physiology
The thyroid gland is butterfly shaped endocrine organ that sits and wraps around the trachea. Anteriorly the thyroid glands are joined by the Isthmus. Developmentally, the thyroid isthmus can give rise to a structure contiguous called the pyramidal lobe, which extends upward.
Posteriorly the thyroid gland does not connect, however 4 parathyroid glands are attached onto the thyroid gland posteriorly.
The gland is in visceral compartment of the neck, along with the trachea, oesophagus and pharynx. The compartment is enclosed in the pre- tracheal fascia, which anchors the thyroid gland to the trachea, so that the thyroid moves up on swallowing.. The thyroid gland stands at the vertebral level C5-T1.
Embryologically, the thyroid gland begins its development at the base of the tongue before descending down to the trachea. This is the reason why thyroid ductal cysts can occur higher up on the neck, anywhere along the path of descent.
Arterial blood supply:
- Superior thyroid artery ← External Carotid
- Inferior thyroid artery ← Thyrocervical trunk
- Ima Artery (~3% of people) ← Brachiocephalic artery
Venous drainage:
- Superior thyroid vein → Internal Jugular
- Middle thyroid vein → Internal Jugular
- Inferior thyroid vein → Brachiocephalic Vein
Physiology The thyroid gland produces 3 hormones:
- Tridothyronine
- Thyroxine
- Calcitonin
Aetiology
Nongoitrous
- Thyroidectomy
- Post Radiation
Goiterous
- Hashimoto's Thyroiditis (Autoimmune thyroiditis)
- Iodine Deficiency
- De Quervain's Thyroiditis (Sub-acute granulomatous thyroiditis)
- Drug induced - Lithium, amiodarone, aminoglutethimide, interferon alpha, thalidomide
- Post-partum thyroiditis
Risk Factors
- Iodine deficiency
- Female sex
- Middle age
- Family History
- Autoimmune disorders
- Graves' disease
- Post-partum thyroiditis
- Turner's and Down's syndromes
- Primary pulmonary HTN
- Multiple sclerosis
- Radiotherapy
- Iodine deficiency
- Amiodarone use and lithium use
Signs and Symptoms
General Hypothyroidism
- Insidious nonspecific onset
- Fatigue, lethargy
- Pseudodementia
- Constipation
- Cold intolerance
- Muscle stiffness, cramps, carpal tunnel syndrome
- Menstrual irregularity - Menorrhagia, later oligo- or amenorrhea
- Slowing of intellectual and motor activities
- ↑Appetite and weight gain
- Dry skin, hair loss
- Deep hoarse voice
- ↓Visual acuity
- Obstructive sleep apnea
- Depression
| Remember Hashimoto's Thyroiditis is associated with other autoimmune diseases including myasthenia gravis |
Clinical Examination
- General: Deep hoarse voice, mental and physical sluggishness, dry skin
- Face: Puffy eyes, thinning of scalp hair, tongue swelling, xanthelasma
- Thyroid: +/- Goitre
- Cardiovascular: Hypertension, bradycardia, small volume pulse, pleural effusion
- Neurological: proximal muscle weakness, hyporeflexia, carpal tunnel syndrome (bilateral)
| Side note Hypothyroidism has slow deep tendon reflex |
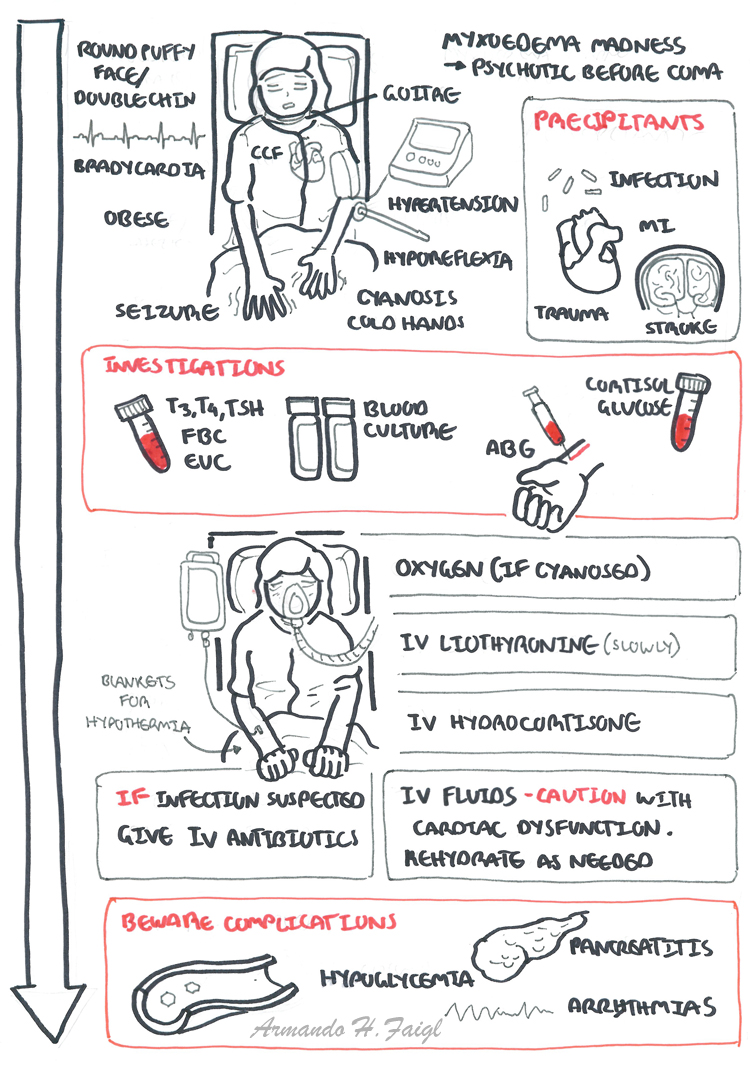
Myxoedema (Medical Emergency) more info down the bottom
- Dull, expressionless face, sparse hair, periorbital puffiness, macroglossia
- Pale, cool skin that feels rough and doughy
- Enlarged heart (dilation and pericardial effusion)
- Megacolon/intestinal obstruction
- Cerebellar ataxia
- Prolonged relaxation phase of deep tendon reflexes
- Peripheral neuropathy.
- Encephalopathy
- Hyperlipidemia
- Hypercarotenemia (also caused by hyperlipidemia, diabetes mellitus,and porphyria)
- Psychiatric symptoms (e.g. depression, psychosis)
Differential Diagnosis
- Primary Hypothyroidism has many causes - identify the cause with investigations
- Secondary Hypothyroidism
- Pituitary adenoma
- Malignancy of the hypothalamus
- Depresssion
- Alzhiemer's Dementia
- Anaemia
Investigations
- Thyroid function test
- TSH - increased
- T3, T4 - decreased
- Serum cholesterol
- FBC
- Glucose
- Antithyroid peroxidase antibodies - for autoimmune thyroiditis (hashimoto's disease)
| Think Secondary hypothyroidism you will have ↓TSH as well as a ↓T3,T4. Might see decrease in other pituitary hormones. |
| Remember If TSH is normal it is always euthyroid |
Pathophysiology
Not up yet guys sorry!
Management
The goal of treatment is reduction of symptoms and prevention of long-term complications.Treatment is given upon establishing the diagnosis and is lifelong. Factors that affect drug dose must be considered.
- Levothyroxine (T4) - lifelong
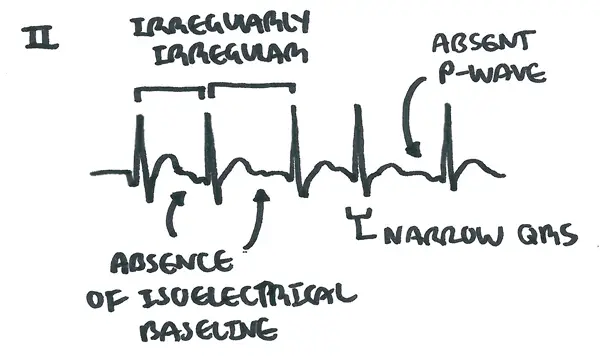
| Pharmacology Levothyroxine (L-thyroxine) is a synthetically made thyroid hormone, mimicking T4. Side effects include increased risk of osteoporosis and atrial fibrillation. High doses can mimic hyperthyroidism state |

Myxoedema before and after treatment. note periorbital oedema, hyperpigmentation of the hand, puffy face and sluggishness - Credit: Popular Science Monthly Volume 51
Complication and Prognosis
Myxoedema crisis (coma)
Overview Myoxedema coma is a serious emergency, due to severe untreated hypothyroidism, and typically presents with impaired consciousness, hypoventilation and hypothermia. Hospitalizations is essential for initial treatment.