Overview
Overview Inflammatory bowel disease is a common condition. It is divided into two types: Crohn disease and Ulcerative colitis. Both these condition differ in pathology, progression and complication, but they do share a lot similar characteristics as well.
| Definition Colitis: Inflammation of the colon, which may be due to infectious, autoimmune, ischemic, or idiopathic causes. Inflammatory Bowel Disease: Autoimmune-mediated intestinal inflammation primarily due to either Crohn disease or ulcerative colitis. |
| Ulcerative Colitis | Crohn’s Disease | |
| Both | Gender | Male<Female |
| 2-19/100,000 | Incidence (per year) | 21-20/100,000 |
| 15-40yo | Onset | 15-40yo |
| Distal colon | Location | Dital ileum and caecum |
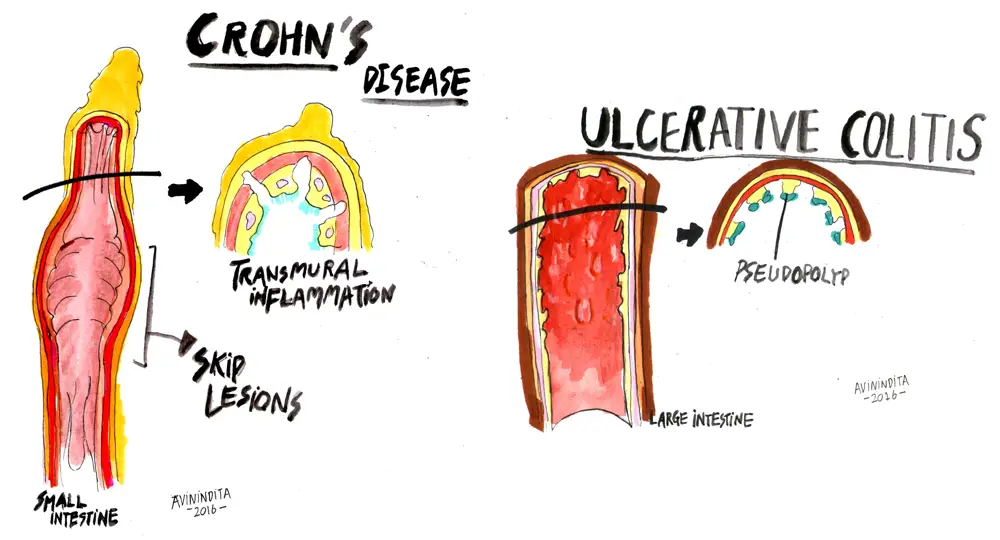
| Continuous superficial inflammatory lesion | Pathology | Discontinuous, patchy transmural inflammatory skip lesions |
| Severe bleeding, toxic megacolon, perforation, colon cancer | Complications | Stenosis, abcess formation, fistula, strictures, colon cancer |
Risk Factors
| Risk Factors | |
| Ulcerative Colitis | Crohn's Disease |
| Family history of inflammatory bowel disease | White ancestry |
| HLA-B27 | Family history |
| Infection | High sugar diet |
| NSAIDs | Oral contraceptive pill, NSAIDs |
| Not smoking or former smoker | Cigarette smoking |
| Not breastfed | |
Signs and Symptoms
| ULCERATIVE COLITIS CLINICAL PICTURE | |||
| Proctitis (50%) | Left-sided colitis (30%) | Pancolitis (∼20%) | |
| Area affected | Inflammation of the rectum | Inflammation from rectum up to the splenic flexure | Inflammation of the entire colon |
| Rectum and deification | Rectum always involved. Symptoms of urgency and frequency due to rectal irritablity. | Rectal irritation | |
| Stool | Blood mucus mixed with loose stools (frank bloody diarrhea rare) | Bblood mucus in stools, often leading to diarrhea | Diarrhea |
| Side note Ulcerative colitis typically presents in young adults with relapsing bloody diarrhoea, malaise, fever and weight loss. Crohn's can have similar presentation or have a more insidious onset with other complications such as malabsorption and pain. |
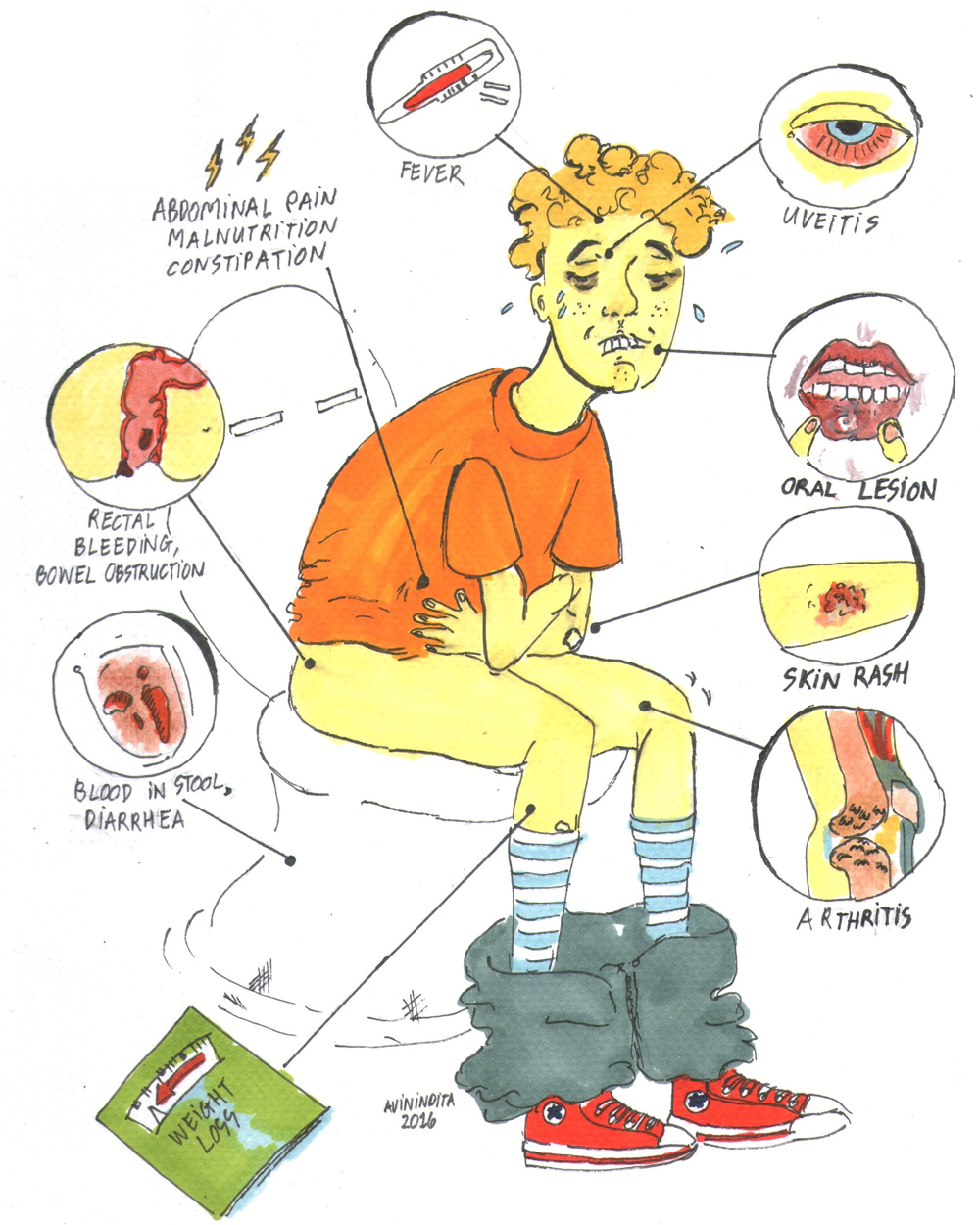
Extra-intestinal Manifestations
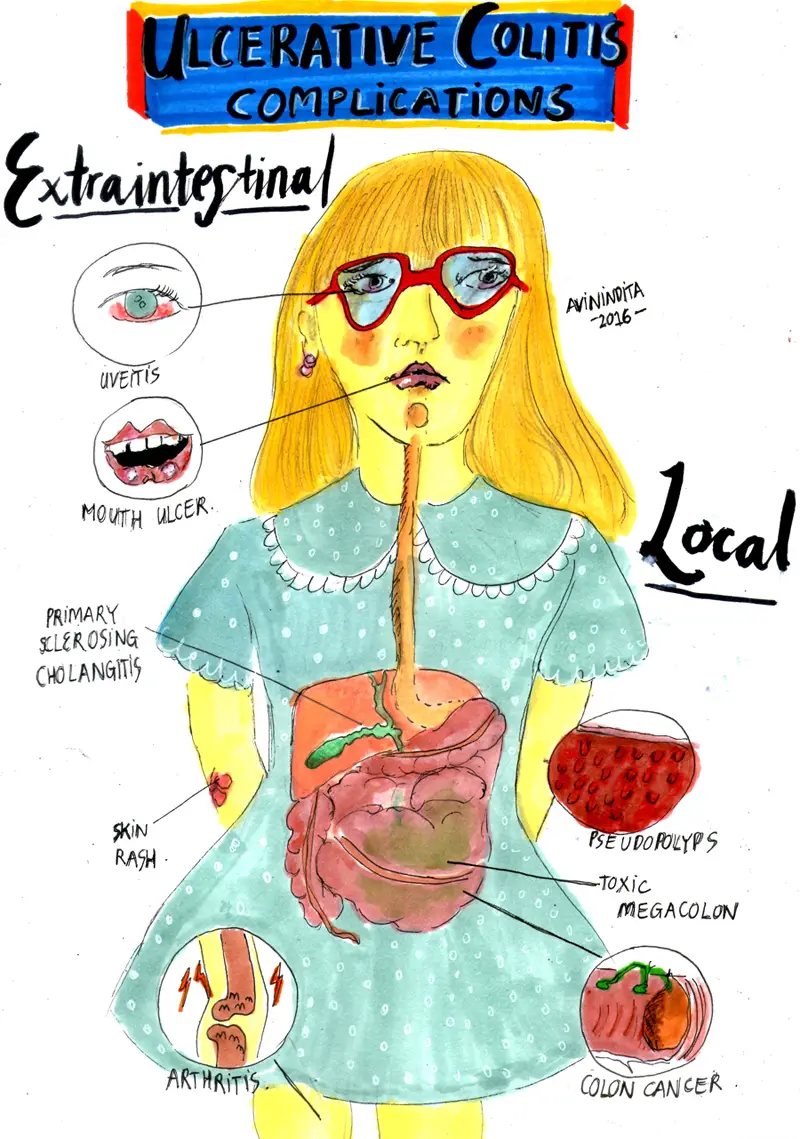
- Both UC and CD
- Uveitis (Iritis/conjuctivitis)
- Mouth ulcer
- Large joint arthritis
- Skin Rash (Erythema nodosum and/or Pyoderma gangrenosum)
- Anaemia
- Ulcerative Colitis
- Liver disease: Primary sclerosing cholangitis, Cirrhosis, Amyloidosis
- Crohn Disease
- Renal disease: stones and amyloidosis
- Gallstones
- Osteomalacia
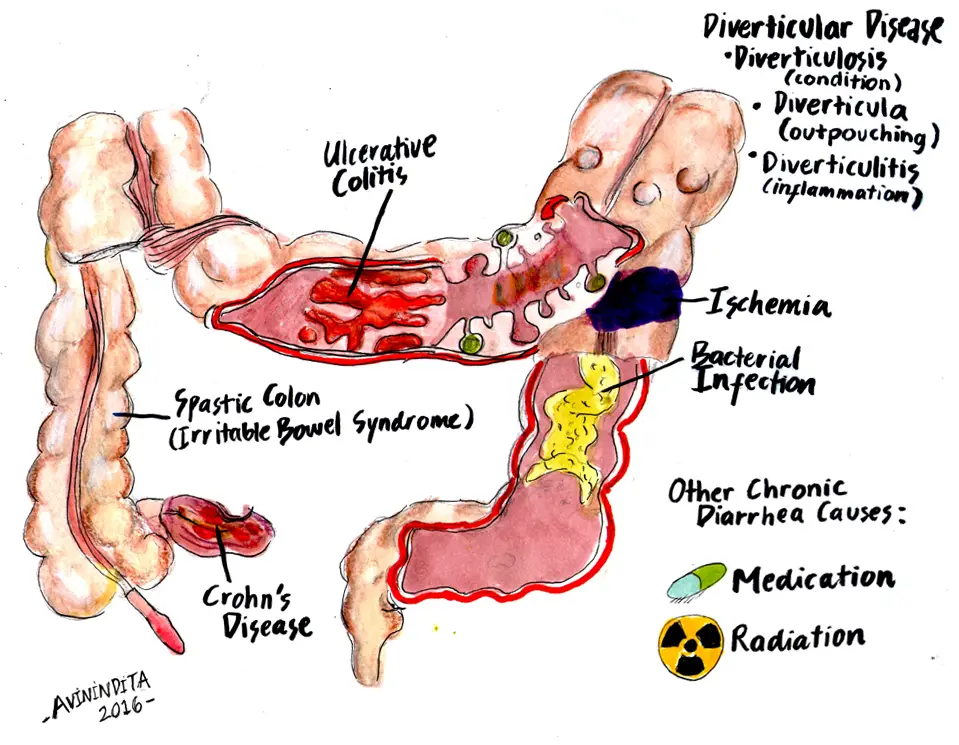
Differential Diagnosis
The differential diagnosis of inflammatory bowel disease includes other causes of chronic diarrhoea
| Remember Infection must be excluded, and it is necessary to check for infections with organisms such as Entamoeba histolytica, Salmonella, Shigella, E coli, and Campylobacter, as well as Clostridium difficile, which can occur in the absence of prior antibiotic exposure. |
Causes of Colitis (inflammation of the colon)
- Inflammatory Bowel Disease
- Infection
- Radiation
- Ischaemic colitis
- Diversion colitis
- Toxic exposure (chemicals)
- Lymphocytic colitis
- Collagenous colitis
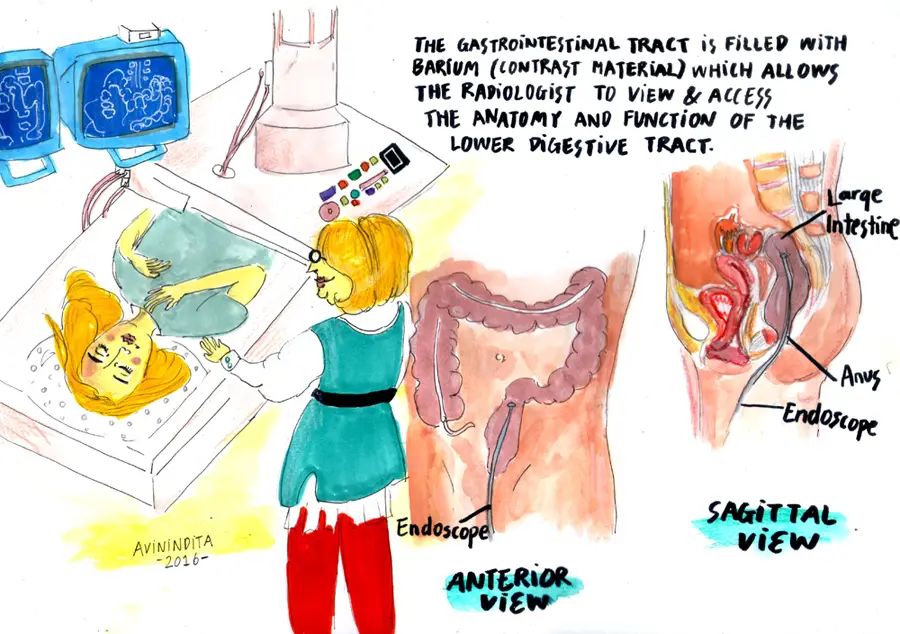
Investigations
General
- Stool culture - to rule out C. difficle colitis
- FBC - increase WCC, decrease Hb
- ESR/CRP - increased
- Serum folate
- Serum vitamin B12
- Abdominal X-ray - may show oedematous colonic mucosa (thumbprinting)
Specific for Ulcerative Colitis
- Colonoscopy – sigmoidoscopy usually shows erythematous, grandular, or frankly ulcerated rectal mucosa with mucus and blood
- Biopsy - check severity and to Exclude Crohn's disease
- Serological markers – ANCA (70% of patients with UC have this)
- Serological marker – ASCA (70% of patients with Crohn’s have this)
Specific for Crohn's Disease
- Double-contrast barium enema (rarely used) - in subacute/chronic presentations to show mucosal irregularity and narrowing.
- CT - may show an inflammatory mass, abscess formation, localised or free perforation
- MRI - for anal disease
- Biopsy - check severity and confirm Crohn's disease
Diagnosis
- Presence of chronic diarrhea for more than four weeks and evidence of active inflammation on endoscopy and chronic changes on biopsy.
- Eliminate differentials with:
- History - risk factors
- Laboratory studies - stool culture for bacteria (C. difficile, Salmonella, Shigella, Campylobacter, Yersinia)
- Endoscopy - continuos inflammatory lesion beginning mainly from the distal colon
Pathology
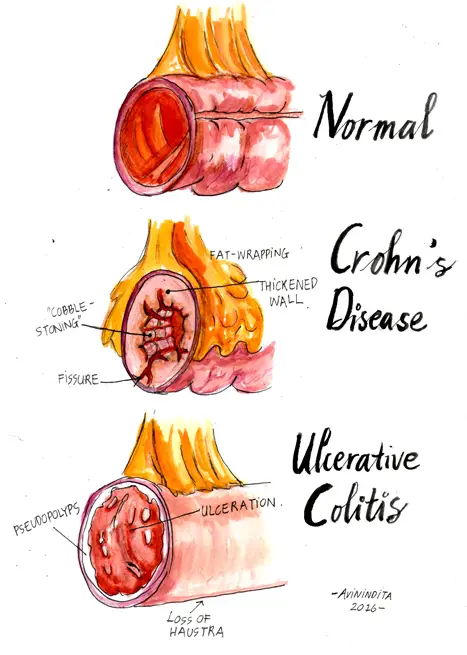
| Ulcerative Colitis | Crohn's Disease |
| Superficial inflammation. Disease present in the distal colon and rectum and spread proximally with increasing extend of disease. | Transmural inflammation. Disease commonly focused in the terminal ileum and caecum, but may affect the anus, colon, or entire small bowel. |
| Acute neutrophil infiltration in the mucosa and submucosa | Lymphoid aggregates, particularly in the subserosal tissues (Crohn's rosary). |
| Mucosal crypt abscess with goblet cell mucin depletion | Mucosal crypt ulceration, and fissuring ulceration. |
| More severe inflammation, there can be aphthous ulcers, granulation tissue -> pseudopolyps | Mucosal thickening and cobblestone. |
| Chronic 'burnt out' disease leads to a pale, featureless, ahaustral pattern to the colon. Transmural inflammation may occur in sever cases. | Extensive fibrosis and muscle hyperplasisa may occur, giving rise to stenosis. Perforation, fistulation, and abscess formation are occasional sequelae of transmural inflammation. |
Management
The management differs for UC and CD. CD is more severe and encounters more complications. The principles of medical treatment is to reduce inflammation and prevent complications.
General
- Close monitoring - bloods
- Acute derangement in blood results should be corrected (ie. blood transfusion for severe anaemia, potassium supplementation, nutrition support).
- Diet modification
- Medical treatment
- Steroids (suppository or systemic)
- 5-ASA
- Oral immunosuppresives (methotrexate, azathiopurine)
- Immunomodulators (anti-TNFa)
- Antibiotcs
- Surgical treatment
- Ulcerative colitis - indicated for acute colitis that fails to respond to treatment and for chronic colitis
- Crohn's disease - deal with septic complications, relieve significant bowel obstruction, and remove as little bowel as possible.
| Ulcerative Colitis Medical and Surgical Treatment | |||
| Proctitis (50%) | Left-sided colitis (30%) | Pancolitis (~20%) | |
| Topical steroids (suppsoitories or foam enema) | + | + | + |
| 5-ASA | + | + | + |
| Systemic Steroids (prednisalone) | - | -/+ | + |
| Oral immunosuppressives (azathiopurine) | - | - | + |
| Immunomodulators (anti-TNFa) | - | - | + |
| Surgery is indicated for acute colitis that fails to respond to treatment and for chronic colitis. Surgical treatment include removing parts of bowel or entire colon. | |||
| Crohn's Disease Medical and Surgical Treatment | |
| Medical Treatment | Surgical Treatment |
| 5-ASA | Acute: Free perforation, sever haemorrhage, acute severe colitis, complete intestinal obstruction |
| Systemic steroids (hydrocortisone, prednisolone) | Subacute: Inflammatory mass, subacute obstruction, abscess formation, symptomatic fistulation |
| Immunosuppressives (azanthiopurine, methotrexate) | Chronic: Steroid dependency or complications, cancer treatment |
| Immunomodulators (anti-TNFa) | |
| Dietary modification | |
Complications and Progns
Local Complications
- Ulcerative Colitis
- Toxic Megacolon
- Perforation
- Massive haemorrhage
- Strictures
- Carcinoma of the colon
- Crohn Disease
- Anorectal Disease
- Obstruction
- Fistula
- Carcinoma of the colon
Extra-intestinal Manifestations
- Both UC and CD
- Uveitis (Iritis/conjuctivitis)
- Mouth ulcer
- Large joint arthritis
- Skin Rash (Erythema nodosum and/or Pyoderma gangrenosum)
- Anaemia
- Ulcerative Colitis
- Liver disease: Primary sclerosing cholangitis, Cirrhosis, Amyloidosis
- Crohn Disease
- Renal disease: stones and amyloidosis
- Gallstones
- Osteomalacia
| Think Because of transmural inflammation, Crohn disease often is complicated by fistula formation. |
Prognosis
Ulcerative Colitis
- Surgery can be curative
Crohn's Disease
- Recurrence of the disease after resection occurs in some 50% of cases within 10 years















