Mitral Regurgitation (Incompetence)
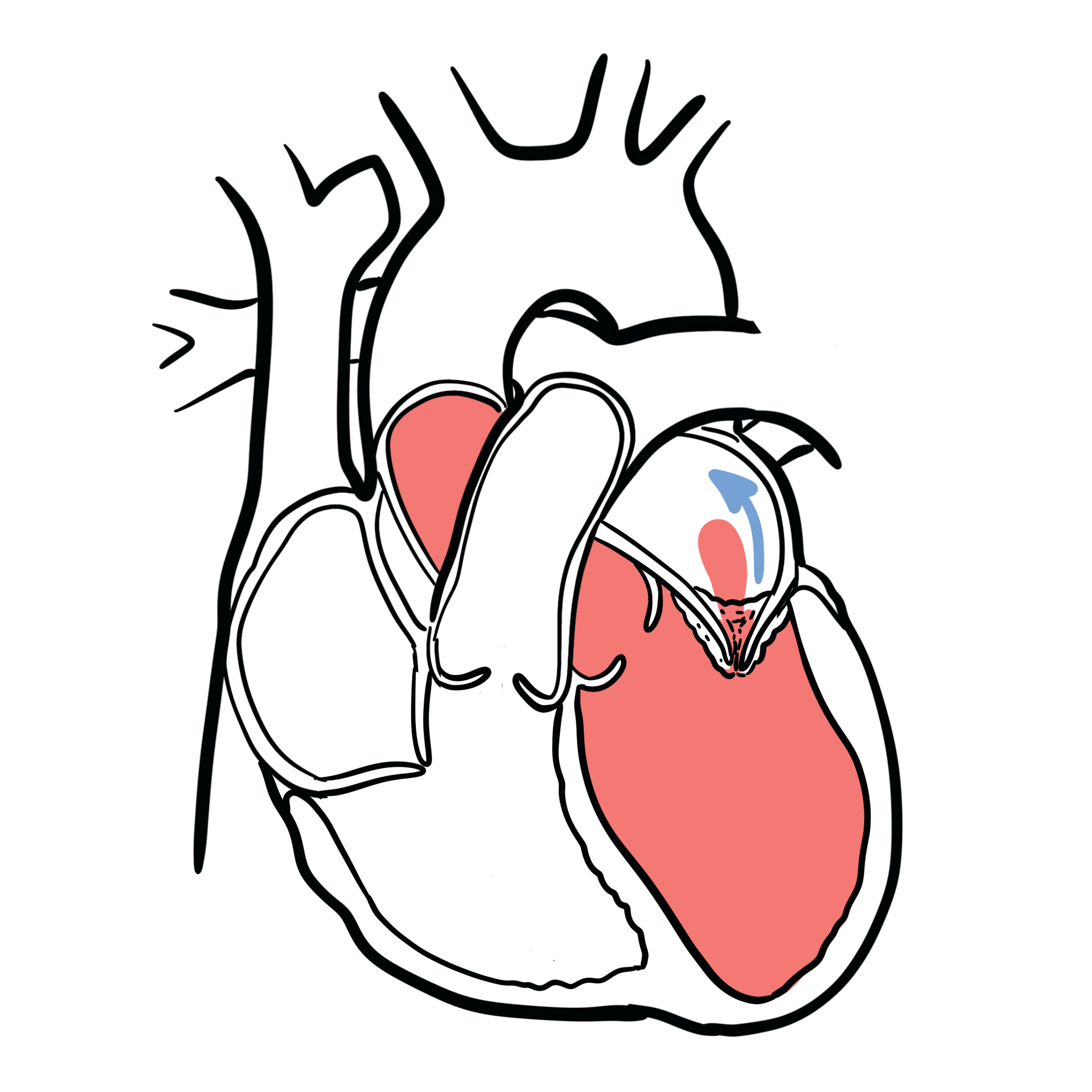
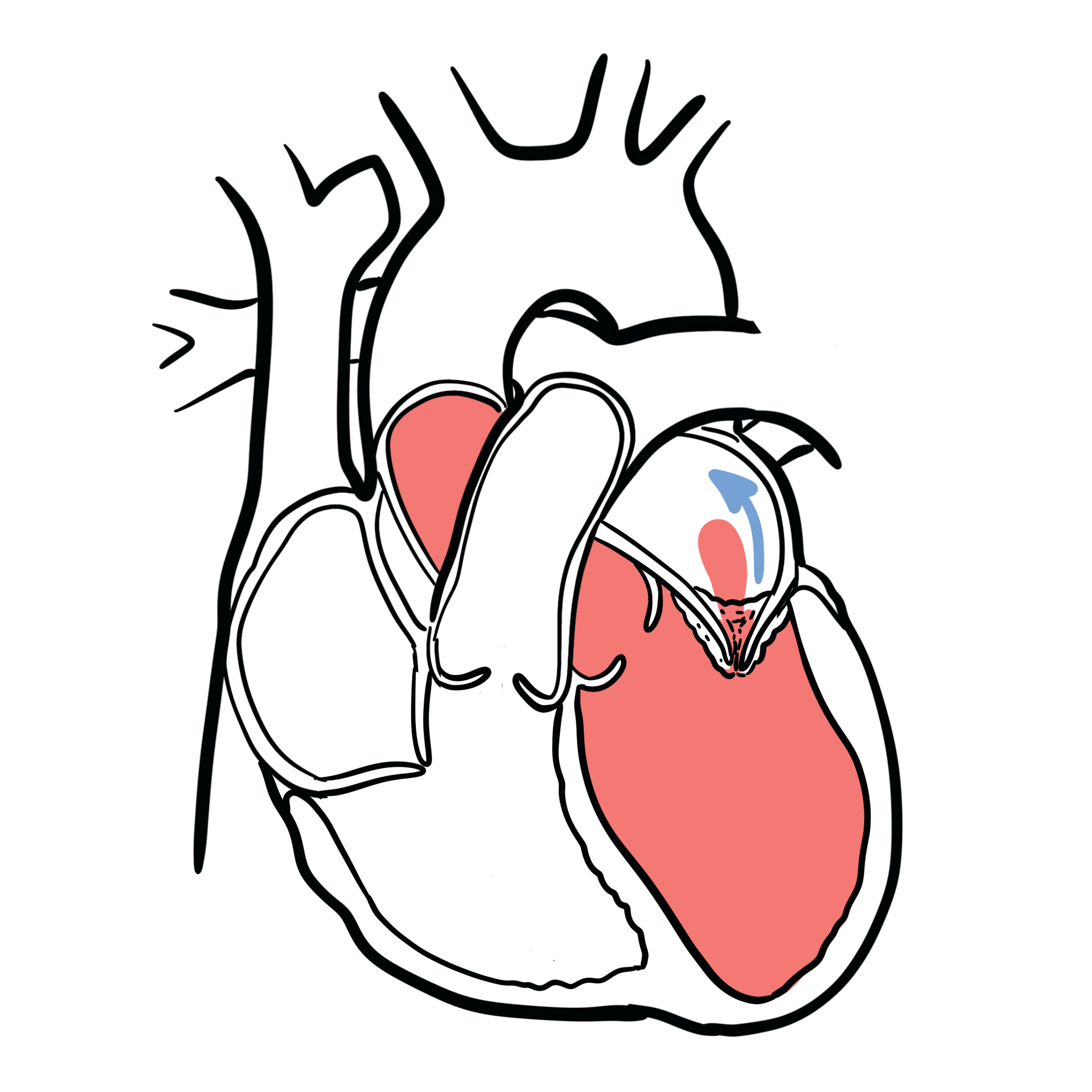
Mitral regurgitation (MR), which is also known as mitral insufficiency, is a common heart valve disorder. When MR is present, blood leaks backwards through the mitral valve when the heart contracts. This reduces the amount of blood that is pumped out to the body. Patients with acute mitral regurgitation (MR) are often gravely ill with significant haemodynamic abnormalities that require urgent medical and usually surgical treatment.
MR can be acute (pulmonary oedema), chronic compensated or chronic decompensated.
Heart Valve
The heart has 4 valves:
The Mitral and tricuspid valves are atrioventricular valves meaning they allow blood to move from the atrium to the ventricles of the heart. This occurs with ventricular diastole.
The aortic and pulmonary valve are tricuspid valves which when open allow blood to move to the aorta and pulmonary system respectively. This occurs during ventricular systole when the heart contracts.
Surface anatomy of the heart valves
All of the heart valves except the mitral valve are usually tricuspid. However, there can be congenital bicuspid valves which can predispose one to valvular disease later on. The heart valves can be heard most prominent in the following regions of the chest
There are three basic mechanisms of Mitral regurgitation:
Another way of thinking about aetiology. Primary causes include abnormality of dysfunction of any component of the mitral valve apparatus. Secondary causes (functional MR) abnormality of dysfunction of the left ventricle.
| Risk Factors |
| Mitral valve prolapse |
| History of rheumatic heart disease |
| Infective endocarditis |
| History of cardiac trauma |
| History of ischemic heart disease/ MI |
| Congenital heart disease |
| Hypertrophic cardiomyopathy |
| Anorectic/dopaminergic drugs |
Primary causes abnormality of dysfunction of any component of the mitral valve apparatus
Secondary causes (functional MR) abnormality of dysfunction of the left ventricle
Pathophysiology Acute MR
Pathophysiology Chronic MR
Acute MR presents as a cardiac emergency, however chronic MR typically presents with no symptoms until late stage.
Acute Mitral Regurgitation presents with Left sided heart failure.
Most people with mitral regurgitation (MR) have no symptoms. People with mild to moderate MR may never develop symptoms or serious complications. A trivial amount of mitral regurgitation (MR) is present in up to 70 percent of adults. Significant (moderate to severe) MR is much less common.
Cardiac Examination
Cardiac Examination includes a murmur heard over the left 5th intercostal space mid-clavicular. The murmurs is a flat continuous murmur which radiates to the axilla. There also tends to be a diminished S1.
Clinical Signs of severity
Breathing out as if you were straining (vasalva manoevre) increases intrathoracic pressure -> decreases venous return and accentuates murmur from mitral valve prolapse and hypertrophic obstructive cardiomyopathy.
Clinical history and examination findings of MR. Ultrasound finding of mitral valve insufficiency.
Acute Mitral Regurgitation
Inoperable patients
Operable patients
Chronic Mitral Regurgitation
If in AF, anticoagulate with warfarin (however now NOACs are being more frequently used).
Complication
Mitral Valve Prolapse
Overview Most common congenital valvular lesion. Associated with Marfan’s Syndrome and Ehlor’s Danlos Syndrome.
Clinical Examination
Mitral valve prolapse has a systolic click where as regurgitation does not!
Complications
Leg raise and squatting increasing blood flow back to the heart. Valsalva decrease blood to the heart.
Only Mitral valve prolapse and HOCM murmur increase with murmurs.
Best Practice
UptoDate
Oxford Handbook Clinical Medicine

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion