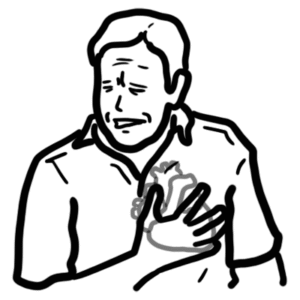
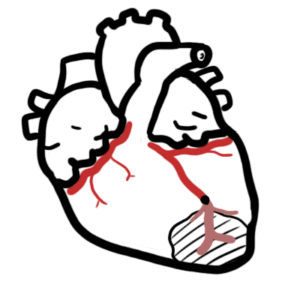
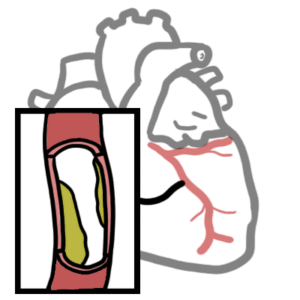
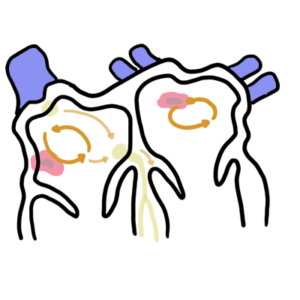
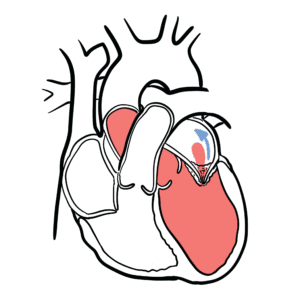
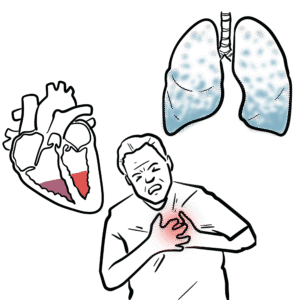
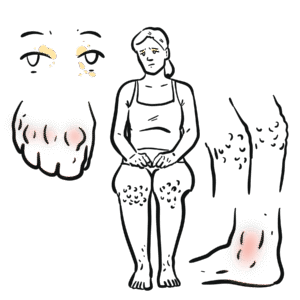
0:00 Hello, in this video, we're going to talk about acute compartment syndrome. 0:09 This is an overview and introduction. 0:12 In this specific video, we're going to talk about the leg affected by acute 0:16 compartment 0:17 syndrome, but the same principles apply to any part of the body, essentially. 0:23 Before moving on, it is important to know that the muscle groups of the human 0:28 limbs 0:29 are divided into sections or compartments. 0:32 And so, compartment syndrome occurs when there's increased in pressure within a 0:37 compartment, 0:38 which compromises circulation and function to the tissues within that area. 0:45 Compartment syndrome can actually be acute, such as from trauma or chronic, 0:50 which occurs 0:50 in elite athletes. 0:52 We're mainly concentrating on acute compartment syndrome, and the common sites 0:57 for acute 0:58 compartment syndrome is the leg, as well as the forearm. 1:04 Here I'm drawing the leg of a person, and on the right, we can see, obviously, 1:08 an enlarged 1:09 leg, which is meant to represent a compartment syndrome. 1:14 Before going into acute compartment syndrome, let's talk about the compartments 1:18 of the leg 1:19 as an example. 1:20 In reality, it can be any compartments, such as the forearm or the thigh. 1:25 We're just using a leg in this video, remember? 1:29 So first, let us look at normal compartments in a leg to get an idea. 1:34 So here is a cross-section of the leg. 1:37 Here is the tibia, bone in T, and the fibula bone in F. These are the bones of 1:45 the leg. 1:47 Now the muscle compartments of the leg can be divided into four. 1:51 We will not look at what the names of the muscles are within the compartments. 1:55 We will mainly focus on the compartments themselves. 1:59 Now the leg compartments include the posterior compartment, the lateral 2:04 compartment, the anterior 2:05 compartment, and another posterior compartment. 2:09 This one is the deep posterior compartment, whereas the previous one was the 2:14 superficial 2:14 posterior compartment, which includes the soleus and the gastroc muscles. 2:20 So in summary, the leg has four compartments, and in each compartment, you have 2:25 muscles 2:25 that run through them. 2:28 Within each compartment, you also have neurovascular bundles, which includes 2:32 the archery, the vein 2:33 and the nerve. 2:34 Why is this so that the muscles can be supplied by them? 2:39 Each compartment has a thick fascia around it, but fascia also surrounds each 2:44 individual 2:45 muscle. 2:46 Here is an example of a muscle with fascia around it. 2:49 The muscle is made up of smaller units of muscle bundles, which are also 2:52 surrounded by fascia. 2:55 Each muscle bundle is made up of even smaller units called muscle fibers. 2:59 These are the muscle cells. 3:02 The muscle altogether supplied by nerves, arteries and veins that supply that 3:09 area. 3:10 In acute compartment syndrome, there is a build-up in pressure in one or more 3:15 compartments of 3:16 a particular limb, in this case the leg. 3:19 Here is a diagrammatical representation of all the compartments in the leg 3:23 swelling up 3:24 because of the increase in pressure. 3:30 This increase in pressure that we see in compartment syndrome leads to 3:34 compression of the neurovascular 3:35 bundles, which further increases the pressure, and also can lead to devastating 3:41 consequences 3:42 if not corrected. 3:45 The pathophysiology behind compartment syndrome, to put it simply, here in blue 3:50 is the vein 3:51 that drains from the muscle and from the extremities. 3:55 Here in red is the artery that supplies the muscle with oxygen, and here in 3:59 yellow in 4:00 the middle is the muscle itself, the compartment, essentially. 4:05 Many things can trigger acute compartment syndrome, but let us say for 4:08 simplicity's sake there 4:09 is direct damage to the muscle, or arterial injury in the muscle. 4:16 This will all cause some form of inflammatory process and reaction, which will 4:21 eventually 4:22 cause fluid to shift into the muscles, causing compartment edema. 4:28 This increases the pressure. 4:30 When there is increase in pressure, eventually the arterial supply will be 4:34 reduced to that 4:35 area, because blood cannot go through, and this will eventually lead to the 4:40 death and 4:41 the crisis of that area. 4:45 When there is death of the cells, this further triggers an inflammatory 4:49 reaction, causing 4:50 further edema, and further increasing compartment pressure. 4:54 It's like a vicious cycle. 4:57 What actually aggravates this whole process even more is when the increase in 5:02 pressure 5:03 in the muscle compartment actually inhibits the drainage of the veins from the 5:07 distal 5:08 extremities. 5:10 Because the veins cannot drain properly, it just pools, the blood pools causing 5:14 further 5:14 edema, and this can occur in the extremities as well as in the compartment. 5:20 And all this will further increase pressure. 5:23 The lymphatics will initially try to compensate by draining some of this fluid, 5:26 but it just 5:27 soon overwhelmed. 5:29 And so with this build up in pressure and inflammation process, we see the 5:34 signs and 5:35 symptoms of acute compartment syndrome, which includes mainly pain out of 5:40 proportion to 5:40 the apparent injury, haryesthesia, and deep burning constant pain. 5:48 What is more important is the clinical findings. 5:52 History examination is very important for acute compartment syndrome. 5:56 Examination involves looking at the six Ps. 6:00 These six Ps include pulse, pulse can be present even with acute compartment 6:07 syndrome. 6:08 Haryesthesia is common. 6:10 Pain is probably the most important initial finding. 6:14 Pain can even be aggravated by passive stretching of the affected compartment. 6:20 For example, if there is posterior compartment involvement, dorsiflexion will 6:25 stretch the 6:26 posterior compartment, aggravating the pain on the posterior compartment. 6:30 Similarly, acute compartment syndrome occurring in the anterior leg compartment 6:35 can be aggravated 6:36 by plantar flexing, which stretches that compartment. 6:42 Pala is the fourth P, and in compartment syndrome, pala is uncommon. 6:47 What is more common is pink, because the limb still has some form of blood 6:54 supply. 6:54 The fifth P is pressure. 6:57 Pressure includes pain when touching the affected limb. 7:01 Also very important, patients with acute compartment syndrome is often 7:04 described as feeling 7:05 wood-like on palpation, because of the increase in pressure. 7:10 The final sixth P is paralysis, which is the latest finding. 7:16 We briefly looked at the pathophysiology, the signs and symptoms, and clinical 7:20 examination 7:20 of acute compartment syndrome. 7:23 Let us look at what can cause acute compartment syndrome. 7:27 Some of these are also the risk factors. 7:30 The etiology or cause of acute compartment syndrome include fractures, which 7:35 make up the 7:35 majority, 75% of cases, thermal burns, crush injury, penetrating injury. 7:44 Non-traumatic causes of acute compartment syndrome are less common, and include 7:49 thromosis, 7:50 bleeding disorders, and vascular disease. 7:53 Finally, illicit drug use, chronic use abuse, is also a cause because of the 7:59 use of tourniquets 8:00 or injury by needle puncture. 8:05 Investigations include full blood count, creating kinase, which is raised 8:08 because of the damage 8:09 to the muscle cells. 8:11 It is important to remember rhabdomilysis in this case. 8:15 Rhabdomilysis is where you have injury or damage to muscle tissue. 8:20 This leads to similar findings to acute compartment syndrome. 8:25 Rhabdomilysis also has elevated creatinine kinase. 8:29 Rhabdomilysis can lead to acute compartment syndrome because it is essentially 8:33 muscle injury. 8:36 In Rhabdomilysis, myoglobin is also increased in urine. 8:41 And so another investigation for acute compartment syndrome, suspicion, is 8:46 urine analysis using 8:47 dipstick, which will show red blood cells, which correlates to the myoglobin in 8:52 this case. 8:54 Finally, a pressure measurement may be used, which is mainly done by surgeons 8:59 to assess 9:00 severity and the need to operate. 9:03 The management of acute compartment syndrome is important. 9:07 Please have the suspicion of acute compartment syndrome if someone presents 9:10 with acute muscle 9:11 pain with the background of a fracture. 9:15 A immediate contact to a surgeon is necessary if acute compartment syndrome is 9:20 suspected 9:21 and the management will really depend on what the surgeon wants to do. 9:25 It can be conservative if not too serious and is improving. 9:30 It is important to hydrate and achieve urine output for adults greater than 0.5 9:35 milliliters 9:36 per kilogram per hour plus minus urine alkalization. 9:40 The problem is that elevated C, creating kinase and myoglobin is actually toxic 9:45 to the nephron, 9:47 to the kidneys, and so you want to flush it out. 9:51 Morphine is also important for pain relief, but the main form of treatment is 9:56 surgery, 9:56 which is a fasciautomy, and as the name suggests, it's essentially opening up 10:01 the fascia layer. 10:03 The main goal of fasciautomy is to decrease the pressure in that compartment 10:08 that the 10:09 fascia surrounds. 10:12 For example, let's go back to the same scenario, the same image where we have 10:17 all the compartments 10:18 of the leg having increased pressure. 10:21 A fasciautomy aims to make the least number of cuts to the body to decrease the 10:26 compartment 10:27 pressure. 10:28 For the leg, therefore, the incisions are made on either side of the tibia, 10:32 which will 10:33 cover all four compartments, and thus decrease pressure in all four comp 10:38 artments. 10:39 Zooming in, by performing a fasciautomy, pressure is decreased in the 10:43 compartment, which will 10:44 allow proper flow of arteries and veins and nerves that were previously 10:49 compressed. 10:49 Finally, if the surgeon thinks the limb is not viable, because it was detected 10:54 too late, 10:54 for example, and there is gangrene, then the limb amputation is performed. 11:03 Thank you.