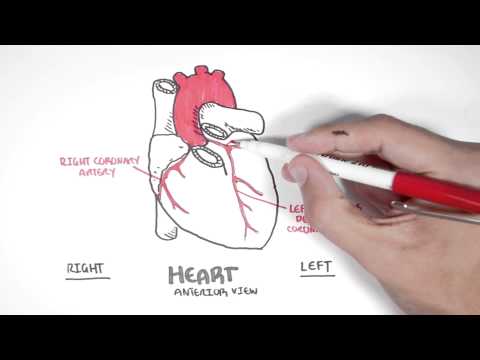
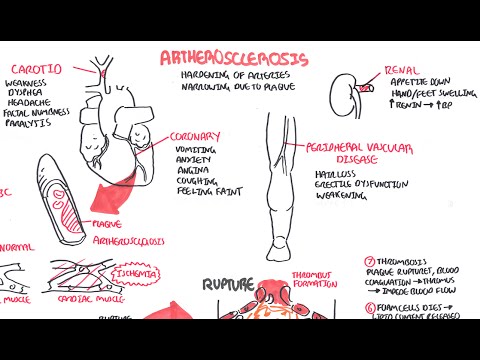
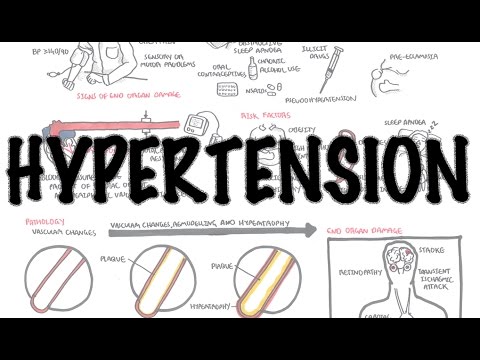
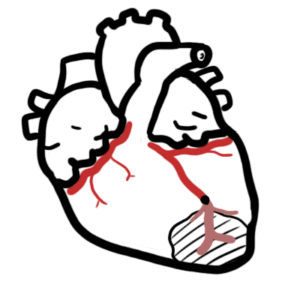
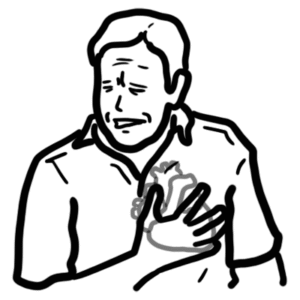
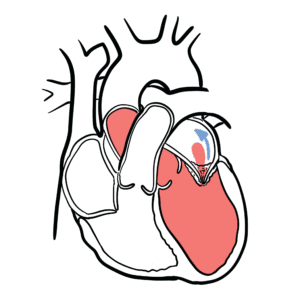
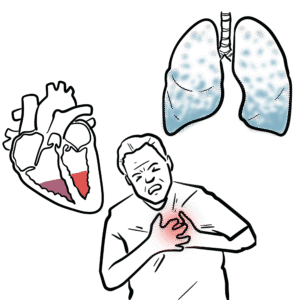
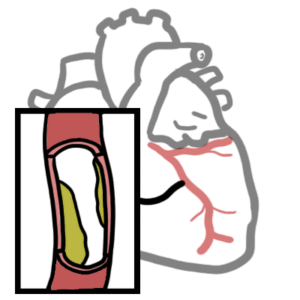
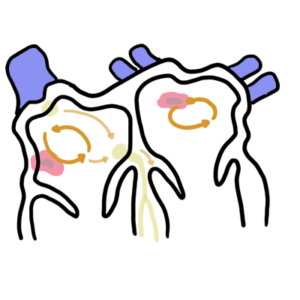
0:00 Hello, in this video we're going to talk about acute coronary syndrome, which 0:08 is a 0:09 syndrome characterized by a reduction or occlusion of blood supply to the heart 0:16 . 0:17 And so we begin by revising the anatomy of the heart just quickly, so the heart 0:21 consists 0:21 of four chambers. 0:24 The left ventricle here will pump blood to the rest of our body via the main, 0:28 big artery, 0:29 the aorta. 0:31 And coming off the aorta are two main arteries which supply the heart muscles 0:38 itself. 0:39 These are the right coronary artery and the left coronary artery. 0:43 The left coronary artery further divides to two main arteries, the left 0:48 anterior descending 0:50 and the left circumflex artery. 0:53 These arteries supply the heart muscles, the cardiomyocytes. 0:58 Zooming into the area, we can see the artery here bringing blood and therefore 1:03 bringing 1:03 oxygen to the cardiomyocytes, thus it will result in a healthy cardiomyocyte. 1:09 However, over time, atherosclerotic plaques can build up within these coronary 1:16 arteries. 1:16 And this is usually due to non-modifiable risk factors, such as aging, male sex 1:25 , family 1:26 history and certain ethnicities such as being Caucasian. 1:30 Now the buildup of plaques can cause a reduction in blood flow to the area, to 1:35 the cardiomyocytes, 1:37 leading to poor oxygen supply. 1:39 This can cause symptoms such as angina, chest pain, when people are exerting 1:45 themselves. 1:46 This is because when you exert yourself, the heart needs more oxygen and so 1:50 needs more 1:50 blood supply, but because the vessels can't meet the demand of the heart, you 1:55 get angina 1:56 as a result. 1:58 Angina can be either stable or unstable. 2:02 In unstable, you have chest pain even when you're resting. 2:07 And this is of course a lot more serious. 2:10 But of course the plaque can get worse, and it can even rupture, causing thromb 2:15 osis. 2:16 But the vessel is not tojly occluded here, and this is what we can call a my 2:21 ocardial 2:22 infarction still. 2:24 The infarction of the myocardial tissue occurs distally to where that vessel 2:29 supplies, and 2:30 so there's ischemia proximally. 2:33 This is referred to as a non-stemmy. 2:37 And usually other risk factors contribute to this progression more rapidly. 2:42 And these risk factors are the modifiable risk factors usually. 2:46 And these include smoking, hypertension, having uncontrolled dyslipidemia, poor 2:52 diet, 2:53 obesity, diabetes, and having a sedentary lifestyle. 2:59 Now the rupture of the plaque can also result in a total occlusion of the blood 3:03 vessel, 3:03 of the archery, and this means no oxygen will go to the hot muscle cell in that 3:09 area. 3:10 This is also a myocardial infarction, causing death of cardiomyocytes distally, 3:16 and then 3:16 it will slowly progress proximally unless the occlusion resolves. 3:23 A complete occlusion of the coronary artery causing an infarction is called a 3:28 stemmy. 3:29 So in an infected muscle cell, you have cardiac muscle cells which undergo nec 3:35 rosis, specifically 3:36 a process called coagulative necrosis. 3:40 Now, stemmy and non-stemmy, as well as unstable angina, are what we refer to as 3:46 acute coronary 3:47 syndrome. 3:48 And again, acute coronary syndrome is a syndrome where you have a reduction in 3:52 blood supply 3:53 to the hot muscles or a loss or total occlusion and so no supply of blood to 3:59 the hot muscle 4:00 cells. 4:02 And so acute coronary syndrome presents with very similar symptoms, and it is a 4:07 medical 4:07 emergency. 4:09 The clinical presentation include central chest pain, usually described as a 4:13 crushing sensation 4:14 or heaviness, as well as tightness around the chest. 4:19 This pain can radiate to the neck, jaw, and left arm. 4:24 You can have diaphoresis because of sympathetic activation, feeling of 4:28 impending doom, and 4:29 nausea and vomiting from parasympathetic response. 4:32 It is important to remember that chest pain that occurs while exerting, and if 4:37 a person 4:37 rests and the pain goes away, this is usually stable angina. 4:43 And remember, unstable angina, you still have pain, chest pain, when you rest. 4:51 Differential diagnosis of a myocardial infarction include those that cause also 4:57 central chest 4:58 pain or pain around the chest. 5:00 And these include pericartitis, inflammation of the pericardium, aortic aneurys 5:06 m, dilatation 5:07 of the aorta, endocarditis, infective endocardium, pericardylifusion or tampon 5:14 ade, which is 5:15 essentially presence of fluid within the pericardial sac, and anxiety is 5:20 another very common 5:21 differential diagnosis. 5:24 You have other ones such as pulmonary embolism, where an emboli lodges in the 5:28 pulmonary arteries 5:29 or the capillaries, and this can cause pleuritic chest pain. 5:34 Finally, there is esophageal rupture, which is another medical emergency, and a 5:38 good differential. 5:39 Now let's look back at the site of infarction. 5:43 Now if a cardiac muscle cell dies, they release things in the blood. 5:47 The cardiac muscle cells are made up of myosin and actin filaments, which are 5:50 very important 5:51 in muscle contraction, as you know. 5:55 Actin have these things called troponin, on them, which usually helps in the 5:58 contraction 5:59 process. 6:00 There's also enzymes around the area, creating kinase Mb, which are important 6:05 for energy 6:06 transfer of ATP within the cell. 6:10 Anyway, when the cardiac muscle cell dies, necrosis, the troponin and the CKMB 6:16 get released 6:17 into circulation, and these are measured to see if the hot muscle necrosis has 6:24 occurred, 6:25 essentially. 6:26 And so if we were to draw a graph with time on the x-axis and serum cardiac 6:31 markers, 6:32 not enzymes, on the y-axis, we can see that troponin levels rise very rapidly 6:38 and peaks 6:39 about day two after the onset of chest pain before dropping down. 6:46 Creating kinase Mb rise also rapidly, but not as high, and drop off a lot 6:53 faster. 6:54 Thus, as you can see, measuring cardiac markers, especially troponin, is very 7:00 useful and important 7:01 to help diagnose a stem-y and also a non-stem-y. 7:07 On a side note, in stable angina and unstable angina, the cardiac mar curves, 7:14 such as troponin, 7:16 are not elevated. 7:19 So if someone presents with those signs and symptoms of acute coronary syndrome 7:23 , such 7:23 as the central chest pain relating to the left, you must perform investigations 7:29 . 7:29 And these include an ECG to check signs of a stem-y or non-stem-y, a full blood 7:35 count, 7:36 EUC, glucose, lipid profile, and of course most importantly, cardiac markers or 7:43 cardiac 7:43 enzymes such as troponin and creating kinase Mb, but usually troponins are the 7:48 only one 7:49 ordered. 7:50 An x-ray is also useful to rule out other differentials, if you suspect them. 7:56 But it is important to not delay treatment. 7:59 On a chest x-ray, you can, you might see signs of cardiomegalae. 8:05 So let us now look at the ECG changes in acute coronary syndrome, beginning 8:10 with unstable 8:11 angina. 8:13 The ECG, also known as the electrocardiogram, is very important to diagnose 8:18 acute coronary 8:19 syndrome. 8:20 Specifically, stem-ys or non-stem-ys, however, 20% of ECGs may be normal 8:25 initially. 8:25 ECG shows five main waves, which correlate with parts of the heart while it's 8:30 contracting 8:30 and relaxing. 8:32 These are the P-wave, QRS complex, and the T-wave. 8:37 In unstable angina, you don't usually see any ECG changes, it is usually normal 8:43 or you 8:43 can see a T-wave inversion, so a dipping of the T-wave. 8:49 To understand the pathophysiology of unstable angina, as well as the other 8:55 acute coronary 8:56 syndrome, let us just recap the coronary arteries and the heart, ventricles 9:02 here. 9:02 So you have the right and left coronary arteries, which are the first two 9:06 branches of the aorta. 9:08 The left coronary artery divides and forms two other big arteries, the left 9:13 anterior descending, 9:14 which supplies the anterior and septal parts of the heart, and then the left 9:18 circumflex 9:18 artery, which supplies the lateral wall of the heart. 9:21 Myocardial infarction or heart attack tends to occur within the left anterior 9:27 descending, 9:28 and then the right coronary artery, and then the left circumflex. 9:34 If we take a cross section of the heart like this, this is what it would look 9:38 like. 9:39 And here is where the right ventricle is, and your left ventricle. 9:44 This in front here is the left anterior descending, which again supplies your 9:49 anterior wall of 9:50 the heart as well as your septum in the middle. 9:53 This is your left circumflex artery, which supplies the lateral wall of your 9:58 heart. 9:59 And at the back, wrapping around is your right coronary artery, supplying the 10:03 right wall and 10:05 posterior wall of the heart. 10:08 But now we will mainly focus on the left ventricle. 10:10 Of course, you have the other layer of the heart called the pericardium, which 10:15 essentially 10:15 is a sheath that wraps around the heart and actually wraps around the coronary 10:19 arteries 10:20 as well. 10:22 Let's take a closer look now at the left anterior descending artery, and what 10:27 happens 10:27 is an unstable angina, which make up one of the three types of acute coronary 10:32 syndrome. 10:33 So here is a cavity of the left ventricle. 10:36 The three layers of the heart from the inside is the endocardium, myocardium, 10:40 and the epicardium. 10:43 Epicardium also make up part of the pericardium as well. 10:48 Again here, we are focusing on the left anterior descending artery, which is 10:51 the most common 10:51 artery affected in heart attacks. 10:54 Now in unstable angina, you get reduction in blood supply to the heart muscle 10:57 as a result 10:58 of the plaque, which is partially occluding the artery. 11:02 And so you get ischemia to the muscle wall, but you don't get infarction. 11:07 And this can occur at rest, and can cause symptoms of angina, the chest pain. 11:13 However, unstable angina can progress to a non-stemmy. 11:18 In a non-stemmy, you get significant occlusion of the artery because of a rupt 11:24 ured plaque, 11:25 subsequent thrombosis leading to poor oxygen supply. 11:28 But the artery is not fully occluded. 11:32 The significant reduction in oxygen supply to the muscle wall causes infarction 11:37 distally 11:38 and ischemia proximally to the artery supply. 11:43 The infarcted area is called a sub-endocardial infarction. 11:49 Interestingly, the endocardium is not infected because it is receiving blood 11:55 straight from 11:56 the ventricle, the cavity where the blood pools essentially. 12:01 Sub-endocardial infarction is a characteristic of non-stemies. 12:07 Non-stemmy is called non-stemmy because on ECG you do not see a ST segment 12:12 elevation. 12:13 Rather, you see an ST segment depression, and this is a characteristic finding 12:18 of a non-stemmy. 12:21 A non-stemmy can progress yet further or can result from a transient stemmy. 12:27 A stemmy again is characterized by a ST segment elevation on the STG. 12:37 What happens in a stemmy is you have a complete occlusion of the artery 12:42 essentially. 12:43 Because of the ruptured plaque, subsequent thrombosis causing complete occl 12:48 usion. 12:49 Complete occlusion means you have no blood supply to the myocardium, and this 12:52 means you 12:52 have initially infarction distally to where the vessel supplies, and the infar 12:57 ction will 12:58 progress proximally very rapidly until you get a transmural infarction. 13:06 Perpetual means essentially trans, which is across the myocardium essentially. 13:14 With a transmural infarction, you can also cause damage and rupture of the pap 13:19 illary muscles 13:19 here, which help the heart-valvular function. 13:25 Damage to the papillary muscles results in other complications such as mitral 13:29 regurgitation 13:30 or mitral prolapse. 13:32 With a transmural infarction, it is very important to also look for ecg 13:37 findings which suggest 13:38 a new left bundle branch block. 13:41 To find a left bundle branch block, just remember the name William. 13:46 The L in William suggests a left sort of bundle branch. 13:52 The W and M of William tells you what features to look at at leads V1 and V6 on 14:01 the ecg. 14:02 In leads V1, you see a widened QRS with a W shape, or pointing down, and V6, 14:10 you see 14:10 a widened QRS in an M shape with a QRS pointing up. 14:15 A new left bundle branch block may suggest infarction of the septum of the 14:19 heart, where 14:20 the left bundle branch goes through. 14:23 Remember, the septum is also supplied partially by the left anterior descending 14:29 artery. 14:29 Finally, let's talk about the cardiac markers. 14:33 In a stemi, you see elevation of cardiac markers. 14:39 Similarly, in a non-stemi, you also see elevation of cardiac markers such as 14:44 troponin. 14:44 But in an unstable angina, you've got none. 14:47 You've got no cardiac markers. 14:51 Let's just say you're at the emergency department, and someone has presented 14:54 with the signs and 14:54 symptoms, and the risk factors suggesting acute coronary syndrome, specifically 14:59 a stemi 14:59 or a non-stemi, a heart attack, essentially. 15:03 You perform the investigations and diagnose a stemi or non-stemi. 15:09 You've done this because you looked at the troponins and the ecg findings. 15:13 The management of acute coronary syndrome may differ depending on what country 15:17 you're 15:17 in, but essentially, it's easily remembered as mone, such as moaning. 15:24 This is performed on all suspected cases of acute coronary syndrome, and this 15:29 includes 15:29 M for morphine, or specifically for opioids, intravenously, always for oxygen 15:35 if the oxygen 15:36 is low, A is for aspirin, as well as clopidogryl to protect the heart from 15:41 further insult, 15:42 as well as nitrates to reduce the workload on the heart and to allow for more 15:46 oxygen 15:46 flow to the heart. 15:49 So the initial management was mone, but what's next? 15:53 So after the initial management, it is the definitive management. 15:57 So in a stemi, the ST segment elevated myocardial infarction, emergency reperf 16:04 usion is commenced. 16:06 The first choice or first line is primary percutaneous coronary intervention, 16:10 also known 16:11 as PCI. 16:12 This is where an angiogram is performed. 16:14 The occluded segment is cleared with a balloon and a stent inserted to allow 16:19 blood flow back 16:20 to the myocardial. 16:21 A PCI is always first choice, however, PCI is only good in a certain timeframe 16:26 as a general 16:27 rule, and the faster the time, the faster the better. 16:32 But if a PCI is not available at a hospital, or if it will take too long to get 16:37 to the place 16:38 where the PCI is, or if the person presents too late to the hospital, then it 16:43 is recommended 16:44 to go for the second choice, which is fibronolitic therapy, also known as throm 16:50 bolysis. 16:51 And as the name suggests, you are breaking down the thrombus, lysis, as in 16:54 breaking 16:55 down. 16:56 Agents used include streptokinase, altoplase, and retipylase. 17:02 Now streptokinase is not as popular now because I think it's been shown to 17:06 cause some reactions 17:07 in some people. 17:09 The definitive management for unstable angina or non-stemmy depends on risk 17:14 stratification. 17:16 The risk stratification will basically tell you whether the patient requires a 17:21 certain 17:21 medication or a certain intervention, or whether monitoring is good enough. 17:27 So for example, a high-risk person should be commenced on anti-platelets, ant 17:33 icoagulant 17:34 therapy and beta blockers. 17:36 You can consider glycoprotein to B3A inhibitors and revascularization, which 17:41 includes angioplasty 17:42 and stenting as well. 17:44 However, the low-risk and intermediate patients require just continuous 17:49 monitoring of cardiac 17:50 markers and ECG to see if any changes will occur, and if there are changes that 17:56 might 17:57 suggest them being high-risk, then they go to the high-risk management, and 18:02 that should 18:03 be commenced. 18:04 However, after a while, if no changes have occurred with blood tests and ECG, a 18:09 follow-up 18:10 cardiologist review is suggested. 18:15 And therefore ongoing management, after everything has resolved, of all acute 18:19 coronary syndromes 18:20 include one lifestyle modification, which includes quit smoking, reduce alcohol 18:27 intake, 18:28 but eat healthy eating habits, lose weight and exercise regularly. 18:33 Pharmacological therapy ongoing can be remembered with the pneumatic ABAS. 18:38 So A is for ACE inhibitors or angiotensin receptor blockers, which help reduce 18:43 blood 18:44 pressure and also help reduce workload of the heart. 18:48 B is for beta blockers, which help blood pressure, as well as heart rate, to an 18:54 extent. 18:54 A is for aspirin and plopidogryl to help prevent plots from forming. 19:00 S is for statins to help reduce cholesterol. 19:05 In this part of the acute coronary syndrome video, we will look at the changes 19:09 that occur 19:10 in an ST-elevated myocardial infarction over time. 19:15 So looking at the pathological changes both microvascularly and macrovascularly 19:21 , and then 19:22 look at the ECG correlation, as well as complications of a myocardial infar 19:30 ction. 19:31 So here is the cross-section of the heart, the right ventricle and the left 19:36 ventricle. 19:37 Coronary arteries surround the heart, and here is a pericardium, which wraps 19:41 around 19:41 the coronary arteries as well as the heart. 19:45 Zooming in from where the left anterior descending supplies the anterior wall 19:48 of the heart, 19:50 we can see here is a stemi, which has occurred. 19:55 In a stemi, there is occlusion, total occlusion of the artery that supplies the 19:59 area of the 20:00 heart, and essentially a transmural infarction has occurred. 20:04 The infarction occurs distally to the vessel, and then progresses proxently, 20:08 unless the occlusion 20:09 is stopped or resolved. 20:12 The changes occurring straight away following an occlusion in up to 12 hours 20:20 include cardiomyocyte 20:22 undergoing coagulative necrosis, and then subsequently edema occurs around the 20:29 area. 20:30 This is essentially the beginning of an inflammatory process. 20:34 The ECG changes as we suspect initially is a peaked T-wave, followed by an ST 20:40 segment 20:41 elevation. 20:43 About 12 to 24 hours after a stemi, you have continued coagulative necrosis, 20:49 and a transmural 20:51 infarction has already occurred. 20:54 You begin seeing neutrophils, which are innate immune cells infiltrating the 20:58 area. 20:59 The heart tissue is a site of inflammation and damage. 21:03 ECG changes during this time still present with an ST segment elevation, which 21:08 may already 21:09 form a pathological Q-wave as well, and plus minus inverted T-wave. 21:17 Within the first week following a stemi, there is cardiomyocyte death, necrosis 21:23 of neutrophils 21:24 as well, which have ruptured and died, and so the whole area is just messy, and 21:31 this is 21:32 where the macrophages start coming in to clean up the area and pick up the 21:37 debris. 21:37 The fibroblasts also begin to infiltrate and mature their depositing collagen 21:41 and other 21:42 tissue matrix to the area, to essentially repair the area, repair the myocard 21:48 ium. 21:48 ECG changes during the first week include a pathological Q-wave and T-wave in 21:56 version. 21:57 Within weeks to months following a stemi, you have fibroblasts forming a lot of 22:02 collagen 22:02 and depositing a lot of collagen there forming scar tissue. 22:08 The person may show evidence of a pathological Q-wave on ECG, a sign that he or 22:14 she has had 22:15 a previous myocardial infarction. 22:17 Finally, let's talk about complications following a myocardial infarction. 22:25 So complications post-MI can be divided into early complications occurring 22:30 within the first 22:31 week following a myocardial infarction or late complications occurring weeks 22:38 after MI. 22:39 Early complications that occur within the first week include arrhythmias, 22:41 specifically 22:42 tachycardias, sinus, VF, AF or bradycardia such as sinus bradycardia and heart 22:50 blocks. 22:51 The rupture can also occur, this includes rupture of the ventricular septum 22:55 which can 22:55 later lead to right-sided heart failure. 22:58 There can be rupture of the left ventricular wall which can cause blood to pull 23:03 within 23:04 the pericardial sac causing a cardiac tamponade. 23:08 Or you can have rupture of the papillary muscles which can lead to mitral reg 23:12 urg or mitral prolapse. 23:15 Early complications also include acute heart failure which usually occurs early 23:19 very early. 23:20 For example causing a left ventricular failure which can then subsequently lead 23:24 to cardiogenic 23:25 shot, plus minus death. 23:27 There's also pericarditis and pulmonary embolism which can occur. 23:32 Late complications occur weeks after MI and include a type of pericarditis 23:38 called dressless 23:40 syndrome which is pericarditis following a cardiac intervention or cardiac 23:45 surgery. 23:46 And then of course another long-term complication post MI is chronic heart 23:50 failure.