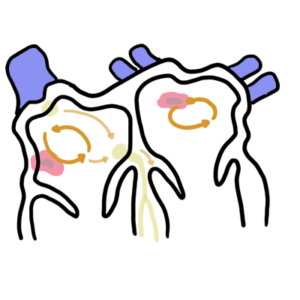
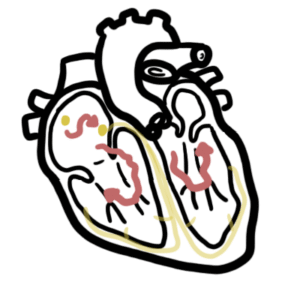
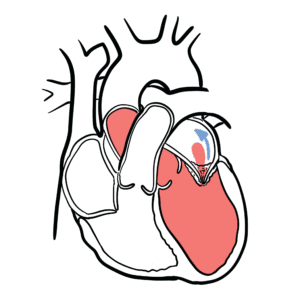
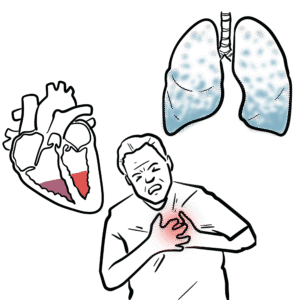
0:00 Atrial fibrillation is the most popular arrhythmia and diagnosed by the finding 0:16 of an irregularly 0:18 irregular ventricular rhythm without discrete p-waves. 0:26 Atrial fibrillation is a supraventricular tachycardia. 0:33 In atrial fibrillation or AF for short, the atria do not contract in a synchron 0:39 ous rhythm. 0:41 Instead they quiver or fibrillate. 0:44 This means that they beat very rapidly and irregularly. 0:48 The most concerning thing about atrial fibrillation is clot formation and embol 0:53 ism due to stasis 0:54 in the atrium. 0:56 The left atrium is commonly involved in clot formation resulting in embol 1:01 ization to the 1:02 brain causing a stroke. 1:10 The sino atrial node is a dominant pacemaker in the heart which sends impulses 1:15 to the atrium 1:16 causing atrial contraction in a synchronous pattern. 1:21 Atrial contraction is represented by the p-wave on the ECG. 1:28 From there, the impulse arrives at the atrial ventricular node. 1:33 The atrial ventricular node conducts the impulse slower. 1:37 It is the gatekeeper to the ventricles. 1:40 From the atrial ventricular node, the impulse travels rapidly along the bundle 1:45 of hiss, 1:46 bundle branches, and perkinje fibers, where the impulse travels causing vent 1:52 ricular contraction. 1:55 Ventricular contraction is represented by the QRS complex on the ECG. 2:03 AF is a result of an initial trigger thought to be from a local ectopic foci 2:11 firing rapidly 2:13 from the pulmonary veins or a single localized re-entry circuit in the atrial 2:20 myocardium. 2:21 Let us take a look at these two mechanisms and how they lead to atrial fibr 2:26 illation or 2:27 AF. 2:32 Ectopic foci are pacemaker cells which initiate an impulse from another 2:37 location than a normal 2:39 conduction system route. The ectopic foci most often occurs from the left at 2:45 rium in the 2:46 muscular sleeves of the pulmonary veins, less often in the right atrium near 2:51 the superior 2:52 vena cava or the inferior vena cava. 3:01 The ectopic foci will fire rapid impulses to the atrial ventricular node and 3:07 other parts 3:08 of the atria, canceling out the normal impulses that are generated. Thus, the 3:15 atrial ventricular 3:16 node will pick up impulses irregularly, resulting in an un-synchronized rhythm 3:23 and a rapid ventricular 3:25 rate. 3:31 The initial trigger for AF could also be as a result of a re-entry circuit. 3:37 A re-entry circuit can form as a result of ischemic heart disease, age, 3:43 hypertension, 3:45 which all changes atrial morphology. It changes the atrial shape and anatomy. 3:55 In AF, the re-entry circuit originates in the atrial myocardium, which have now 4:03 varying 4:04 conductivity and excitability. An example of this morphology change could be an 4:12 atrial 4:13 myocardium, which has slow conducting properties surrounded by normal 4:19 conducting areas. 4:21 The slow conducting myocardium typically have a short refractory period, 4:27 meaning they are 4:28 able to rest and be re-excited faster, whereas the normal conducting myocardium 4:34 have a longer 4:35 refractory period. They require a longer time to rest before being activated. 4:41 So when another impulse from the atrial node arrives to the slow conducting 4:45 area, they 4:46 can be re-excited again. Thus, the slow conducting area can then re-excite 4:52 other normal surrounding 4:53 myocardial tissue as well, which can trigger a re-entry circuit. Once the re- 4:59 entry circuit 5:00 is formed, the impulse generated here will collide and cancel out other 5:06 impulses around. 5:08 The atrial ventricular node will thus capture the impulses irregularly 5:14 resulting in an 5:15 un-synchronized rhythm and a rapid ventricular rate. An ectopic foci may fire 5:26 impulses and 5:26 encounter atrial myocardium with varying conductivity and excitability as well. 5:32 When the impulses from 5:33 the ectopic foci encounter these areas, they can then also trigger a re-entry 5:45 circuit. 5:47 Early in atrial fibrillation, the initial trigger is usually a few ectopic foci 5:53 that 5:53 will terminate within seven days. This is termed paroxysmal atrial fibrillation 6:01 . 6:02 When atrial fibrillation lasts over seven days, it is known as persistent AF. 6:09 In permanent 6:10 AF, restoration to sinus rhythm is impossible. Persistent and permanent atrial 6:15 fibrillation 6:16 is due to progressive conduction and anatomical remodeling in the atria. 6:23 Continuous and recurrent 6:24 atrial fibrillation itself will induce electrical conduction and anatomical 6:28 changes in the atrium, 6:30 which will increase the number of ectopic foci and re-entry circuits, thus 6:36 increase 6:36 the risk for triggering and maintaining atrial fibrillation. Other causes of at 6:43 rial remodeling 6:45 include ischemic heart disease, heart failure, pulmonary hypertension, obstruct 6:51 ive sleep 6:52 apnea, obstructive pulmonary disease. All of these are risk factors for atrial 7:00 fibrillation. 7:02 The classic ECG findings in AF are absent P waves with irregularly irregular 7:08 ventricular 7:10 rate. The isoelectric baseline is not straight and is characterized by F waves, 7:20 which are 7:21 fibrillatory waves. F waves can be very small or large, but these must not be 7:28 mistaken for 7:29 atrial flutter. The heart rate will vary between everyone and can range from 7:35 100 to 180 beats 7:36 per minute. If the heart rate is fast, this is termed atrial fibrillation with 7:43 rapid ventricular 7:44 rate. Atrial fibrillation is a supraventricular tachycardia, and thus the QRS 7:50 complex is narrow. 7:55 Diagnosis of paroxysmal atrial fibrillation is by halter monitor, or implant 7:59 able loop 8:00 recorder, if really necessary. For persistent atrial fibrillation, this can be 8:05 diagnosed 8:06 with an ECG, of course. When thinking of management of atrial fibrillation, it 8:14 's good to think 8:15 about it as acute or long-term management. Let's talk about acute management of 8:22 atrial 8:23 fibrillation. In an acute setting, anyone who is tachycardic and is unstable 8:29 requires 8:30 electrical cardioversion. Synchronized cardioversion picks up the QRS complex 8:36 and delivers a shock, 8:37 and it targets the R waves in the ECG. Electrical cardioversion is followed by 8:43 an ameodron 8:44 infusion typically. Following the electrical cardioversion, hopefully the at 8:49 rial fibrillation 8:50 will revert back to sinus rhythm. If the patient's stable, electrical cardio 8:59 version can be done 9:00 later, or chemical cardioversion can be done instead, using antirethmics. There 9:08 are a number 9:08 of antirethmic agents that can be used for chemical cardioversion, and it's 9:13 based on 9:13 the Singh-Vagan-Williams classification, which targets different parts of the 9:19 cardiac's 9:20 action potential. Common medications for chemical cardioversion used include 9:26 flecanide, which 9:27 is a class 1 antirethmic, inhibiting sodium influx in phase 0, and thus inhib 9:34 iting the 9:35 action potential, slowing the heart rate down. Sotylol is a class 3 antirethmic 9:41 and 9:42 inhibits potassium efflux. This prolongs the action potential and increases the 9:48 time 9:49 before another electrical signal can be generated in the ventricle myocytes. Am 9:56 eodron is another 9:57 class 3 antirethmic agent, and works the same way as Sotylol, but with other 10:03 mechanisms 10:04 as well. In summary, chemical cardioversion will slow the conduction down and/ 10:12 or prolong 10:13 the action potential. Patients who are cardioverted with chemical or electrical 10:20 cardioversion 10:21 means the heart will hopefully go back to normal sinus rhythm. It's very 10:27 important 10:27 to know that if the atrial fibrillation has been going on for over 48 hours, or 10:33 you are 10:34 unsure, a thrombus could have potentially formed from the stagnation and the st 10:39 asis 10:40 of blood in the atrium. If AF has been going on for a while and is reverted 10:47 back to sinus 10:48 rhythm suddenly, the thrombus that has been formed can actually lodge, dislodge 10:54 into the 10:55 cerebral arteries causing a stroke or into the mesenteric arteries causing gut 11:01 ischemia. 11:01 And so to prevent this, before performing cardioversion, a trans esophageal ech 11:07 ocardiogram 11:08 is done to look for a thrombus in the left atrium or left atrial appendage 11:13 prior to cardioversion. 11:15 Alternatively, anticoagulation for four weeks should be done to break any clots 11:21 in the atrium 11:22 prior to a cardioversion. Here's an example of a trans esophageal echocardi 11:31 ogram. Note 11:32 that sometimes patients with AF can have a thrombus form usually in the left at 11:41 rium. 11:42 As from cardioversion, in an acute setting, if the patient is stable, it's 11:47 important 11:48 to rate control the atrial fibrillation. Because atrial fibrillation with a 11:53 rapid ventricular 11:54 response would cause uncomfortable symptoms such as palpitations, dystonia, 12:01 fatigue, 12:02 chest discomfort, as well as dizziness or lightheadedness. There are three main 12:08 classes 12:09 of heart rate medications used in atrial fibrillation. These are beta blockers, 12:15 calcium 12:16 channel blockers and dejoxin. All these drugs affect the atrial ventricular 12:21 node. It slows 12:23 the conduction through the atrial ventricular node, and this results in fewer 12:28 atrial impulses 12:29 being conducted to the ventricles, slowing down the heart rate. 12:36 The outcome of acute management for AF will either be one, the person has 12:41 reverted back 12:42 to normal sinus rhythm, or two, the person still has atrial fibrillation, which 12:48 will 12:49 either be paroxysmal or persistent. Regardless, there needs to be a long-term 12:54 management plan 12:55 for each of these outcomes. 13:00 So for long-term management, patients who have returned to sinus rhythm may 13:05 develop atrial 13:06 fibrillation again later. There needs to be a decision whether long-term rhythm 13:11 or rate 13:11 control strategy is needed, as well as stroke prevention using anticoagulation. 13:18 There is 13:18 no difference in survival between using a rate or rhythm control management in 13:23 the long-term. 13:25 The choice really depends on the side effect profile and contraindications of 13:29 these medications. 13:30 So for rate control, drugs used include beta blockers such as metropolis, 13:35 calcium channel 13:36 blockers and dejoxin. These drugs inhibit sympathetic activation, as well as 13:42 slow down 13:43 the atrial ventricular node conduction. 13:47 Rhythm control drugs include sotylol or amiodrone. These drugs we've already 13:53 talked about earlier, 13:54 and they target different parts of the cardiac action potential. But 13:58 essentially, they will 13:59 slow conduction and/or prolong the action potential. 14:09 Long-term anticoagulation should be initiated if the person has significant or 14:15 sufficient 14:16 risk factors for a stroke. The most common way of assessing this is by using 14:21 the Chads 14:21 Vascular, which are a series of risk factors that get assigned a point and then 14:27 they get 14:27 either put into low, medium or high risk of stroke. 14:33 Low to medium Chads Vascular do not support anticoagulation use, as risk of 14:38 bleeding tends 14:39 to be higher. A high Chads Vascular supports anticoagulation. 14:47 There are different types of anticoagulants used for atrial fibrillation, and 14:52 they are 14:52 really based on whether someone has valvular atrial fibrillation or non-valv 14:58 ular atrial 14:59 fibrillation. It's very important to know the difference. Valvular atrial fibr 15:04 illation 15:04 is when someone has atrial fibrillation and also have mitral valve stenosis or 15:10 they have 15:11 a mechanical valve or they have rheumatic heart disease. Wolfren is the main 15:17 stay anticoagulant 15:19 if patients have valvular atrial fibrillation. It is also used in people who 15:24 have atrial 15:25 fibrillation and who have chronic kidney disease as well. 15:34 Your non-valvular atrial fibrillation, DO-X, also known as NO-X, are used. 15:40 These include 15:40 factor 10A inhibitors such as river oxaban and epixaban, or direct thrombin 15:47 inhibitors 15:48 such as the bigotran. 15:53 Finally, catheter ablation is a highly effective treatment for paroxysmal at 15:58 rial fibrillation. 15:59 In paroxysmal AF there are a few ectopic folkis that can be localized in the 16:04 pulmonary veins 16:06 and eliminated with ablation therapy. However, as AF progresses these ectopic 16:12 sites become 16:13 more complicated and require more complex ablation procedures. 16:18 Thank you for watching. I hope you enjoyed this video on atrial fibrillation. 16:29 [BLANK_AUDIO]