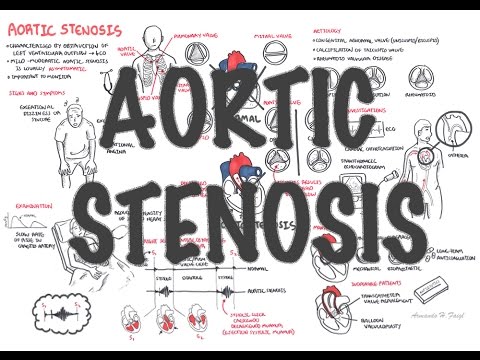
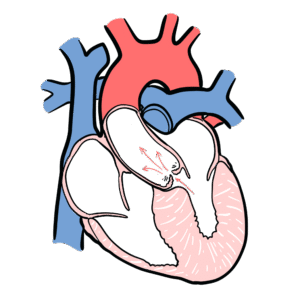
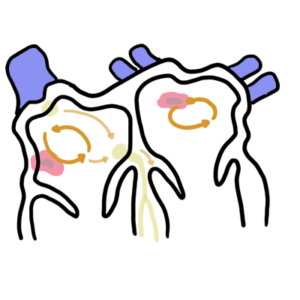
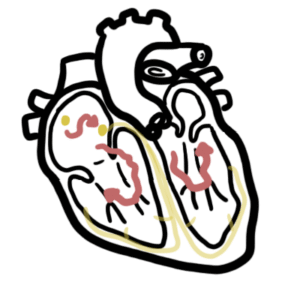
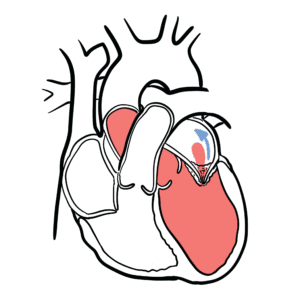
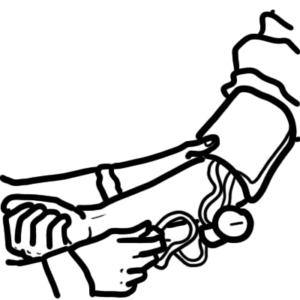
0:00 In this video, we're going to talk about cardiac output, how to calculate 0:15 cardiac output, 0:17 and what factors influence cardiac output. 0:21 So cardiac output. 0:23 Cardiac output is the amount of blood pumped by the heart in one minute. 0:29 Therefore, cardiac output, or CO for short, is measured in milliliters per 0:35 minute. 0:37 Cardiac output can be calculated using two variables. 0:40 The first variable is heart rate, which is the number of heart beats in one 0:46 minute. 0:47 So heart rate, or HR for short, is one variable to calculate cardiac output. 0:54 The second variable is stroke volume, or SV for short, which is the volume of 0:59 blood pumped 1:00 with each ventricle with each beat of the heart. 1:04 This is measured in milliliters per beat. 1:08 So cardiac output, therefore, is the product of HR, heart rate, and SV, stroke 1:16 volume. 1:18 So let's look at an example now of calculating the cardiac output. 1:22 Well, the average heart rate is about 75 beats per minute and the stroke volume 1:27 is about 70 milliliters per beat. 1:30 Cancel the beats out and we can get a cardiac output of 5,250 milliliters per 1:37 minute, 1:37 which is about 5 liters per minute. 1:42 And this is classified as normal. 1:44 The amount of blood passing through the heart each minute is about 4 to 6 lit 1:51 ers. 1:51 And this is quite amazing for an organ that is the size of our fists. 1:56 Now back to the heart rate. 1:59 As we have learned, heart rate is how many beats per minute? 2:04 Well, there are factors that can influence the heart rate. 2:07 There are factors that can positively influence the heart rate, meaning 2:12 increasing the heart rate. 2:14 These are called positive chronotropic factors, and these can result in tachy 2:21 cardia, which is a fast heart rate, over 100 beats per minute. 2:28 Then on the other side, you have the negative influences. 2:31 These are the negative chronotropic factors, and they can result in bradycardia 2:37 , which is the heart rate below 60 beats per minute. 2:45 Let's look at some examples of the positive chronotropic factors. 2:50 Well, the sympathetic nervous system is the main factor, because as we know, 2:54 the sympathetic nervous system is the fight and flight response. 2:58 And so, it would increase heart rate to pump more blood around the body. 3:03 The sympathetic nervous system secretes adrenaline and noradrenaline, or epine 3:09 phrine and norapinephrine, to increase heart rate. 3:14 Then we can have hypercapnia, which is increased carbon dioxide, which would 3:20 increase heart rate, and also a decrease in calcium would increase heart rate. 3:26 The negative chronotropic factors, the main one is the parasympathetic 3:33 stimulation, whose main neurotransmitter is our acetylcholine. 3:40 And then, there is hypoxia, which also decreases heart rate. 3:46 Hypercalcemia will decrease heart rate. 3:52 Now, when dealing with hypercalcemia and hypocalcemia, these usually don't have 3:57 much of an effect on heart rate. 4:00 Rather, they have more of a profound effect on the muscles of the heart, and we 4:05 will talk about it soon. 4:07 So, from this, we know that cardiac output is calculated by heart rate and 4:12 stroke volume, 4:13 and that the heart rate are influenced by positive and negative chronotropic 4:20 factors. 4:21 But stroke volume can also be influenced by many other factors. 4:27 These are preload, afterload, and contractility. 4:32 And because we know stroke volume influences the cardiac output, we can say, 4:39 therefore, there are four total determinants of cardiac output. 4:49 The first determinant of cardiac output is heart rate, as we mentioned, which 4:57 is how many beats per minute. 4:59 The other three determinants of cardiac output are factors that influence 5:03 stroke volume, which in turn affects cardiac output. 5:07 So, one determinant, the second determinant of cardiac output is preload, which 5:14 is the volume of blood entering the ventricles. 5:19 Okay, now let's think about this systematically. 5:22 If we have an increase of blood entering the ventricles of the heart, this 5:29 would mean that we have more stretch of the ventricles, 5:35 and this means that there is an increase in preload. 5:39 And an increase in preload would mean that there is an increase in stroke 5:44 volume, if everything else is normal. 5:49 Now, just to mention, you all probably have heard of the Frank Starling 5:54 mechanism. 5:55 Well, what is it? 5:57 To put it into super simple terms, the amount of blood entering the ventricles 6:03 of the heart would mean that it's the amount of blood ejected from the ventric 6:09 les to the body. 6:10 So, we would say that the end diastolic volume, which is the volume of blood in 6:16 the ventricles prior to ejection, 6:18 will be proportional to the stroke volume. 6:23 If that didn't make sense, don't worry, just the Frank Starling mechanism is 6:29 important, though. 6:31 The third determinant of cardiac output is afterload. 6:36 So, we have had heart rate, preload, and now afterload. 6:40 What is afterload? 6:42 Well, it is the resistance the ventricles must overcome to pump blood around 6:52 the body. 6:54 This means that if someone has high aortic pressure, the afterload would 7:01 increase. 7:02 Because an increase in resistance, which is the aortic pressure, means an 7:07 increase in afterload. 7:10 An increase in afterload means a decrease in stroke volume. 7:16 A decrease in afterload means an increase in stroke volume, and all this will 7:24 influence cardiac output. 7:29 The fourth and final determinant of cardiac output is contractility. 7:34 Now, contractility is to do with the cardiac muscle cells itself, and this is 7:38 pretty straightforward. 7:40 Contractility is how hard the myocardium contracts for a given preload. 7:47 It is basically how hard the heart muscle muscles contract to pump blood out of 7:56 the heart. 7:57 An increase in contractility means an increase in cardiac output, and a 8:01 decrease in contractility means a decrease in cardiac output. 8:05 It is quite straightforward. 8:08 Now, there are factors that actually increase and decrease contractility. 8:14 These are positive ionotropic factors and negative ionotropic factors. 8:21 Let us concentrate on the positive ionotropes first. 8:25 While the sympathetic stimulation can increase contractility, caffeine can also 8:30 do the same. 8:31 An hypercalcemia, an increase in calcium, because calcium is an essential 8:37 component for muscle contraction. 8:42 Then we have the negative ionotropes, which are the parasympathetic stimulation 8:47 , 8:47 a decrease in calcium, hypocalcemia, and an increase in potassium, and in 8:53 particular, myocardial hypoxia, 8:56 where there is not enough oxygen supplying the heart muscle cells. 9:01 Myocardial hypoxia will cause a decrease in contractility. 9:07 Hope that all made sense. 9:09 So that was a brief look at cardiac output and what influences cardiac output. 9:15 So there are four determinants of cardiac output, heart rate, preload, after 9:21 load, and contractility. 9:24 So I hope to enjoy this video on cardiac output. 9:28 The next video we will look at the cardiac cycle as well as the graph. 9:35 Thank you.