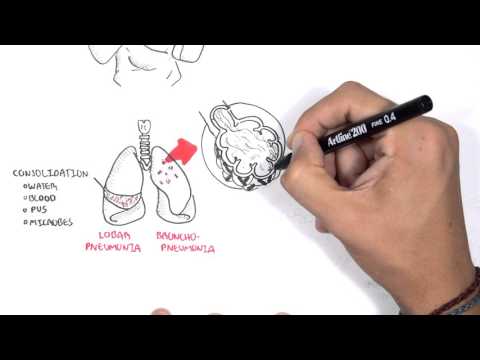
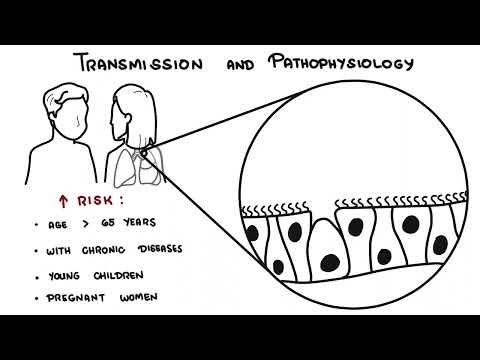
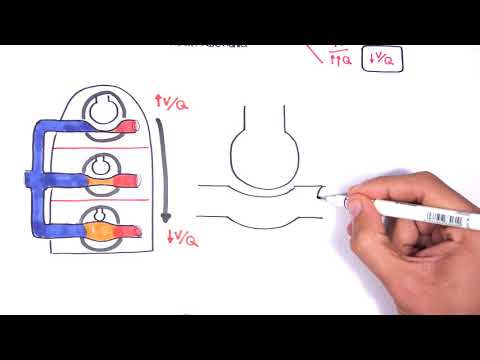
0:00 Hello, in this video, we're going to talk about community acquires pneumonia, 0:10 or cap 0:11 for short. 0:12 This is an overview and introduction. 0:15 So community acquired pneumonia is pneumonia acquired outside hospital in a 0:20 person who 0:21 is not immunocompromised. 0:24 The choice of antibiotics is usually empirical because the etiology or the 0:29 cause of the pneumonia 0:30 is not known for at least 48 hours after admission. 0:34 And severity of the pneumonia is considered using the core or curb or the smart 0:41 cup. 0:42 And this is used to determine severity. 0:46 So in summary, what to do with community acquired pneumonia, it's important to 0:51 assess, stabilize 0:51 the patient, take a history, examination, chest x-ray, and remember to take 0:57 oxygen saturation. 1:00 The clinical presentation of pneumonia include chest pain, dyspnea, a wet cough 1:06 , or a dry 1:07 cough, fever and headache. 1:12 Looking at a lung with pneumonia, it can present as either infection 1:16 inflammation affecting 1:18 a lobe of the lung, this is known as lobar pneumonia, or the inflammation 1:24 infection can 1:26 affect patches throughout the lungs within the airway itself, and this is known 1:32 as bronchod pneumonia. 1:34 These findings might not be visible on the chest x-ray, and it's important to 1:38 know this. 1:40 So let's look at the functional units of the lungs, which are the alveoli. 1:47 The alveoli are clear, they're allowed for exchange of oxygen with carbon 1:52 dioxide. 1:53 In lobar pneumonia, these alveoli are filled with fluid, made up of bacteria, 1:58 pus, blood, 1:59 or fluid, and this fluid substance is called within the alveoli, it's called 2:04 consolidation. 2:06 And it's due to infection, the inflammatory process that occurs within the 2:12 lungs. 2:13 In pneumonia, we get consolidation of the lung, paracimer. 2:18 In bronchod pneumonia, similar things are happening, except the site of 2:21 consolidation 2:22 is really mainly along the airways, the bronchioles, and this can later move 2:28 towards the alveoli 2:29 eventually, leading to lobar pneumonia. 2:33 There are many causes of pneumonia, there can be viral causes, bacterial, 2:37 parasitic, 2:38 or fungal. 2:41 You'll talk more about the etiology or the causes of pneumonia later on in this 2:46 video. 2:46 Now not everyone develops pneumonia, some people are more susceptible than 2:51 others. 2:52 Risk factors for developing pneumonia include smoking, recent antibiotic use, 2:56 age greater 2:57 than 60, a recent respiratory tract infection, having an existing respiratory 3:04 lung disease, 3:05 being immunocompromised and having travelled recently. 3:10 The next question is to ask, is how do these microbes actually cause the 3:15 infection, the 3:16 pneumonia? 3:17 Let us see what forms of barrier we have in our respiratory system that 3:22 prevents these 3:23 infections from occurring. 3:25 So normal pulmonary defences, normal lung respiratory tract defences include 3:30 the nostrils, 3:31 the cough reflex, commensal microorganisms that fight for the area, the mucoc 3:38 illary apparatus 3:39 that sweeps bad things out of the respiratory tract. 3:43 Deep in the lung tissue, we have reciting alveolar macrophages that clean up 3:49 the area. 3:50 We cannot forget our innate immune system, including the antibodies that are 3:56 present, 3:57 the dendritic cells and the mass cells, all which are important in defending 4:01 our respiratory 4:02 tract. 4:04 The pathogenesis of pneumonia occurs when there are personal risk factors, 4:08 environmental 4:09 risk factors or the microbes the causative agents themselves have virulent 4:14 factors which 4:15 enable them to cause an infection, to cause pneumonia and cause consolidation. 4:24 The microbes, the causative agents, have a few modes of entry into the lungs. 4:31 The causative agents can be inhaled which is the most common root of entry. 4:35 The microbes can be aspirated from the upper respiratory tract, this is called 4:40 micro aspiration. 4:42 All the microbes can enter from the GIT and this is known as macro aspiration. 4:50 Microbes can enter the lungs via hematogenous spread, direct inoculation or 4:54 there can be 4:55 activation of dormant infections such as in TB. 5:00 In summary, the microbes have multiple roots of entry into the lungs and 5:04 together with 5:05 its virulent factors and the personal factors and environmental risk factors, 5:12 the microbe 5:13 can cause an infection in the lung and this will lead to pneumonia. 5:20 On examination, a patient with pneumonia can be tachycardic, have a high fever, 5:25 sweating, 5:26 disorientated. 5:27 They have decreased lung expansion on the infected side. 5:33 They can have reduced air entry and bronchial breath sounds. 5:40 Its dullness on percussion on the affected lobe and also increased vocal 5:47 resonance. 5:48 After taking the history and examination, there is an important step which is 5:53 to assess 5:54 the severity of the pneumonia or to assess the severity of how sick the person 6:01 is. 6:01 There are a few methods out there that can be used including Kerbs 65 or Corb 6:06 65 in Australia 6:07 or SmartCop. 6:09 Let's look at Kerbs 65 or Corb 65. 6:13 See, it stands for confusion. 6:16 You, you're looking at urea. 6:19 Greater than 7 millimoles per liter is dangerous or for oxygen sat, less than 6:26 92 is dangerous. 6:28 R is for respite, greater than 30, B is for blood pressure, less than 90 syst 6:35 ole or less 6:35 than 60 diastole and 65 is the number of years or age. 6:43 So each one of these things gives you one point and depending on how many 6:47 points the 6:48 person has can help you predict the severity. 6:53 So zero, a patient who scores zero can likely go home with some oral 6:59 antibiotics for example. 7:01 If a patient scores one to two, you consider hospitalization and if a patient 7:06 scores greater 7:07 than three, they require urgent hospitalization. 7:11 Remember that this is only meant to help assist with assessing severity and 7:15 should not be 7:16 used as gold standard. 7:18 Clinical judgment is important and necessary. 7:22 We talked about the causative agents of community acquired pneumonia, being 7:27 bacteria, viral 7:28 parasitic fungal. 7:30 Now let's talk more about these causative agents but focus on bacteria and 7:35 viruses specifically 7:36 because they are the main causes of community acquired pneumonia. 7:41 In order to look at the causative agents of community acquired pneumonia, we 7:47 can divide 7:48 them into infections in the neonate, children, adults and the elderly. 7:57 In neonates the common agents include streptococcus pneumonia, respiratory syn 8:02 cedial virus, RSV. 8:05 acute B streptococcus and listeria are also common causes of neonatal pneumonia 8:12 and these 8:13 most likely are acquired from the mother after delivery. 8:18 For children, viral causes are the most common including respiratory syncedial 8:23 virus and influenza. 8:25 Common bacterial causes include streptococcus pneumonia and also the atypical 8:30 micropliasm pneumonia. 8:33 Using side point, regular penicillin will not work against micropliasma. 8:39 Tell me why. 8:42 For adults, the main causative agents include streptococcus pneumonia, hemoph 8:48 ilus influenza, 8:49 more accella caralis, micropliasm pneumonia. 8:54 In the elderly, streptococcus pneumonia again and there's also legionella 8:58 species which 8:58 are common. 9:02 Another important point to make is that there is an increased rate of infection 9:06 caused by 9:07 staphylococcus aureus as well as the burdensome methicillin-resistant staphyl 9:12 ococcus aureus 9:13 or MRSA and these are common problematic causes of pneumonia acquired from the 9:24 hospital. 9:26 So in summary, we just looked at the common causes of pneumonia depending on 9:29 the age groups. 9:31 Let us now look at the common causes of community acquired pneumonia depending 9:36 on the severity. 9:38 So mild, moderate, severe. 9:45 Streptococcus pneumonia can cause mild, moderate to severe pneumonia depending. 9:52 Micropliasm pneumonia can cause mainly mild or moderate community acquired 9:56 pneumonia. 9:57 Neuros influenza similarly mild or moderate. 10:01 Plamidophilia pneumonia similarly mild or moderate. 10:05 Respiratory viruses including RSV and influenza usually cause mild to moderate 10:12 community acquired 10:13 pneumonia. 10:19 Other causes of severe pneumonia pneumonia include enteric gram negative 10:24 bacteria usually 10:25 from aspiration and enteric meaning from the GIT. 10:30 There are also other common causes of severe pneumonia include staphylococcus a 10:34 ureus and 10:34 legionella species. 10:40 Investigations for community acquired pneumonia include chest x-ray which may 10:45 reveal consolidation 10:47 in one of the lobes or bronchon pneumonia or nothing at all in the chest x-ray. 10:52 Neuropliasm pneumonia often show by high luck consolidation. 10:57 Performing an ABG is important to check for metabolic acidosis as acidosis is 11:02 associated 11:02 with severe pneumonia. 11:05 Serology tests includes your standard FBC for blood count, liver function tests 11:10 and 11:10 electrolyte urea creatinine. 11:13 Blood cultures and sputum cultures and sensitivity is useful to check for the 11:19 type of bacteria 11:20 and what antibiotic they are susceptible to. 11:25 Microbial investigation interesting point the microbial cause of community 11:30 acquired pneumonia 11:30 is not found in majority of cases. 11:35 Other investigations that can be performed can be performed for specific 11:40 microbes to identify 11:41 specific microbes so for pneumococcal pneumonia urinary antigen testing can be 11:47 done similarly 11:48 for legionnaires disease urinary antigen for serotype A can be performed. 11:54 For viruses immunofluorescent tests can be performed through swabs of the 11:59 throat and upper 12:00 respiratory tract. 12:02 Micropliasm pneumonia you can use complement fixation tests as well as direct 12:07 diagnostic 12:07 techniques. 12:12 The management of community acquired pneumonia include oxygen, fluids, IV, 12:19 analgesics such 12:20 as paracetamol or non-steroidal anti-inflammatory drugs for pain. 12:27 Antibiotic therapy is empirical for diagnosis of community acquired pneumonia. 12:33 In general IV antibiotics is used for moderate to severe community acquired 12:40 pneumonia. 12:41 Finally when patients can tolerate switch to oral antibiotics. 12:46 Oral antibiotics is usually given straight away from mild community acquired 12:53 pneumonia. 12:54 Talking a bit more about antibiotics in general for community acquired 12:59 pneumonia two antibiotic 13:01 types are given empirically. 13:03 This is to target two different groups of bacteria which are unknown. 13:07 Beta lactams is to target the gram positives and the macrolides or amino glycos 13:13 ides are 13:13 to target gram negatives as well as gram positives. 13:17 There's also metronidazole which can be given specifically to target anaerobic 13:23 organisms 13:23 if you suspect aspirational pneumonia. 13:30 After treatment or discharge it is important to follow up at six weeks with a 13:35 chest x-ray 13:35 to the family doctor. 13:37 It is also recommended especially in the elderly to get annual vaccination to 13:42 prevent any further 13:44 pneumonia. 13:51 Now finally let's get all that we've learned and put it all into an algorithm 13:57 into a pathway. 13:58 So first you have clinical history examination which is suggestive of pneumonia 14:03 . 14:03 Nothing to do is order a chest x-ray. 14:06 The chest x-ray can show no consolidation or consolidation. 14:10 If no consolidation consider other diagnosis plus minus pneumonia still. 14:15 If the chest x-ray showed consolidation pneumonia is most likely. 14:20 Assess the severity using the CORB65 or CORB65 or SMART COP. 14:26 Now depending on the severity the patients can then either be treated as an 14:30 outpatient 14:31 or as an inpatient. 14:34 The investigations done on a mild on a patient who has mild severity include 14:41 just bloods 14:42 such as full blood count. 14:46 If all point to mild community acquired pneumonia just treat with amoxicillin 14:50 oral and or doxycycline. 14:54 For patients who require hospitalization it is important to perform other 14:58 investigations 14:59 such as blood cultures, sputum cultures and possibly other specific microbi 15:04 ological tests. 15:06 And then it's important to assess the severity again and the patient will be 15:11 either moderate 15:12 or severe. 15:15 For moderate cap community acquired pneumonia treat with benzyl penicillin IV 15:20 plus either 15:21 doxycycline oral or roxythro myosin oral. 15:27 For severe community acquired pneumonia treat with IV antibiotics all the way. 15:32 IV antibiotics include benzyl penicillin IV plus genta myosin IV or keftriax or 15:38 an IV 15:39 plus azithromycin. 15:44 Again remember to follow up with a chest x-ray at 6 weeks to see if lungs are 15:49 clear. 15:50 Now please know that this pathway I just showed it comes from the Australian 15:54 guidelines from 15:55 2016 and this is most likely going to change and it's most likely different in 16:00 your country 16:01 so just beware thank you.