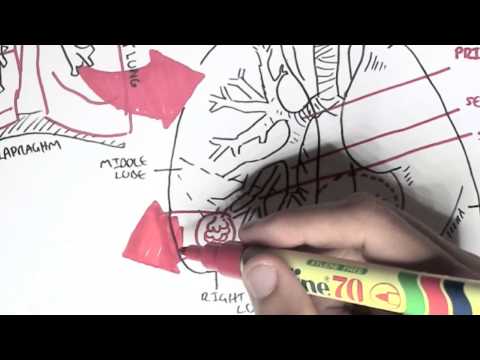
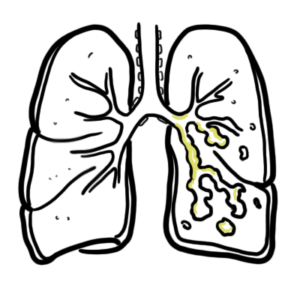
0:00 In this video we're going to look at pneumonia which is the infection as well 0:08 as the inflammation 0:09 of the lungs. 0:11 So here's a person with pneumonia. 0:14 Signs and symptoms of pneumonia include malase, confusion, fever and chills, 0:20 rigor, tachycardia, 0:23 dyspnea or dyspnea, cough can be productive, vomiting as well as diarrhea. 0:30 Risk factors for pneumonia are old patients or people older than 65 years of 0:37 age, smokers 0:38 are being malnourished, having an underlying lung disease, being immunocomprom 0:43 ised, certain 0:44 medications contribute to pneumonia as well as a recent respiratory infection 0:49 also as 0:50 a risk factor. 0:53 Before looking at the pathophysiology of pneumonia, let us first look at the 0:56 function of the lungs 0:57 and the normal defence mechanisms within the lungs. 1:01 So here's the lung and most distal end that make up the lungs are the alveoli. 1:07 Here we are cutting a section of the alveolus with its terminal bronchiol. 1:13 Oxygen is moving in and carbon dioxide is exhaled out, there is mucous lining 1:17 the bronchioles. 1:19 The lower respiratory tract is sterile to commensal organisms as well as any 1:24 organisms. 1:25 We do have microorganisms residing in the upper respiratory tract however. 1:31 Within some alveoli there are alveolar macrophages which help keep the area 1:37 sterile. 1:37 If we look at the trachean bronchins, we see they are made up of special c 1:42 iliated columnar 1:43 epithelial cells. 1:45 There are also goblet cells around the respiratory, lighting the respiratory 1:51 tract which secrete 1:52 mucus. 1:54 The mucus also contain antibodies, IgA, which help eliminate microorganisms. 2:00 IgA antibodies are part of the mucosal immune system. 2:05 Now interestingly, the ciliated epithelial cells actually are special because 2:11 they make up what's 2:12 called the mucocillary escalator. 2:15 So what they do is essentially the bad stuff can be brushed up like so through 2:22 the use 2:23 of the mucocillary escalator, escalator. 2:28 So if we were to summarize our pulmonary defense mechanisms, they include the 2:34 cough reflex, 2:35 the mucocillary apparatus, the alveolar macrophages, mucous secretions, IgA 2:42 antibodies, as well 2:44 as the microflora of the upper respiratory tract and the nose hairs, or nose 2:50 hairs. 2:51 And mouth acidity if you want to include that as well. 2:55 So these pulmonary defenses help us fight off microorganisms at once every day. 3:01 Yes, we do have microorganisms living within our respiratory tract, but these 3:06 guys are 3:07 commensals. 3:08 You do no harm unless you are immunocompromised or unless they just grow wild 3:15 out of control. 3:16 Regardless, again, the lung defenses help protect us. 3:21 Problems or deficiency in these defenses can make people more susceptible to 3:27 lung infection 3:28 such as pneumonia. 3:31 Now, the causative agents of pneumonia in summary can be divided to bacteria, 3:38 viruses 3:38 and fungi. 3:40 Fungi are less common and fungal pneumonia is usually more often seen in those 3:48 who are 3:48 immunocompromised. 3:52 Bacteria is the most prevalent cause of pneumonia. 3:54 Some major bacteria, causative bacteria include strep pneumonia, chemophilus 3:59 influenza, Legionella 4:01 pneumonia, staphylococcus aureus, and mycoplasma species. 4:06 Viruses include the influenza virus, respiratory syncytial virus, and cytomeg 4:11 ally virus. 4:11 Okay, so those are some examples of the big players in pneumonia, the big caus 4:16 ative agents 4:17 in pneumonia. 4:18 Again, these guys are more likely to cause infection of the lung when there is 4:22 a problem 4:23 in the pulmonary defenses or if the person is immunocompromised for that matter 4:28 . 4:29 So let us look at a lung with pneumonia. 4:35 So a person can have personal and environmental risk factors which predispose 4:42 them to having 4:43 pneumonia or the causative agent, the microbes, can have special, virulent 4:50 factors that allows 4:51 them to cause pneumonia. 4:53 So it can be two way. 4:55 If you're looking at a lung that has pneumonia, let us look at an impaired 5:01 pulmonary defense, 5:03 which makes a person more susceptible to pneumonia. 5:06 So here, I'm just drawing the lungs again, the alveolar, and the terminal bron 5:10 chioles. 5:10 So impaired pulmonary defense include loss of the cost of coffee reflex, acet 5:15 ing coma, 5:16 use of anesthetic, injured mucosideri apparatus, due to smoking, decrease in al 5:23 veolar macrophages 5:25 from alcohol and smoking, pulmonary congestion edema, and accumulation of 5:29 secretions such 5:30 as an acystic fibrosis. 5:33 Again these are examples of impaired pulmonary defenses which again makes one 5:38 more susceptible 5:39 to lung infections. 5:41 Okay, so now let's look at quickly how these, the different causative agents 5:46 that we talked 5:47 about actually causes pneumonia. 5:50 So we'll look at mainly bacterial, viral, and fungi, which can enter and infect 5:56 the respiratory 5:57 tract through inhalation of these foreign particles, for example. 6:04 So they enter the lungs. 6:05 Now let's look at each one of these individually. 6:08 So let's begin with bacterial. 6:10 So the bacteria enters the distal part of the alveolar, the respiratory tract, 6:15 which is the 6:16 alveolar line. 6:17 Here we have an alveolar line, we have macrophages reciting, if you remember, 6:21 and here are the 6:22 capillaries. 6:23 So the bacteria enters the alveolar line and it essentially initiates an immune 6:27 response. 6:27 The macrophages reciting here will recognize the bacteria and begins to create 6:32 cytokines 6:32 including TNF alpha into lukein 1. 6:35 Essentially cytokines result in many things, mainly vasodilation of vessels, as 6:42 well as 6:42 increasing vascular permeability. 6:45 Now this will actually result in fluid shifting from the vascular space into 6:54 the alveoli and 6:55 thus will lead to congestion. 6:57 So that was bacterial pneumonia. 6:59 Now let's look at viral, which is quite kind of similar. 7:02 Here again we have the alveoli, we have the macrophages reciting in it and we 7:06 have the 7:06 capillaries here. 7:07 So the viral particles actually infects the respiratory cells itself. 7:13 And so this virus here, if we zoom in, it will infect this respiratory cell and 7:18 it will release 7:18 its genetic material within the cell. 7:21 The genetic material of the virus, it uses the host's proteins and stuff to 7:27 essentially 7:27 replicate and what it essentially creates is many more new viral particles. 7:34 And with many more new viral particles, this essentially causes the cell, the 7:39 respiratory 7:39 cell to lice, releasing these newly formed viral particles. 7:43 So if this happens within the alveoli, you get cellular debris because of the 7:49 dead cell 7:50 and this will initiate again an immune response. 7:53 The macrophages here will release cytokines, which will cause vasodilation, 7:59 increase in 7:59 vascular permeability, resulting in congestion. 8:03 So that was bacterial and viral. 8:05 Lastly, let's look at fungal. 8:07 So fungal pneumonia is kind of different. 8:09 So the spores from fungi, we inhale it or it gets within into our lungs somehow 8:15 and it 8:15 travels down the alveoli as we see. 8:18 And essentially it will, the environment here allows it to grow and it can grow 8:25 into what's 8:25 known as a fungal ball. 8:28 And a fungal ball is essentially, you have fungus, you have mucus and you have 8:32 cellular 8:33 debris all into this big ball. 8:36 And this is what you can see in imaging, this fungal ball. 8:40 Further, the fungi can actually spread, it can go into the vasculature and 8:47 disseminate, 8:48 it can spread, causing systemic effect, which is very, very life-threatening. 8:56 So I hope you understood, that was just a quick overview of how these different 9:00 causative 9:01 agents can lead to pneumonia. 9:03 Now let's go back to the main diagram and talk more about the infected lung. 9:09 So in a lung infection that is pneumonia, we see fluid-filled alveoli. 9:15 We see narrowing of the airways, bronchoconstriction and increase in mucus 9:22 secretion. 9:24 The fluid-filled alveoli is known as congestion. 9:28 In radiological terms, in radiography it's called consolidation, and usually 9:32 occupies 9:33 a lobe of a lung. 9:35 It occupies a lobe because what happens is that the fluid-filled alveoli 9:40 spreads back 9:41 in backflows, causing fluid to flow to other alveoli and so on until the 9:48 consolidation, 9:50 the congestion occupies the whole lobe. 9:54 If we were to define consolidation, it is the process that fills essentially al 9:59 veoli 9:59 with fluid, pus, blood cells, resulting in loba, diffuse opacity. 10:07 So again, consolidation is a radiological term. 10:12 It's basically congestion. 10:15 Smoking is a major risk factor for pneumonia. 10:18 If we see the trachea here, where we have, we find normal, where we normally 10:23 find ciliated 10:23 columnar epithelial cells, smoking actually damages the cilia and so disrupts 10:28 the mucociliary 10:29 escalator, which is normally very important for the pulmonary defense. 10:35 And there's also an increase in mucus secretion as a result of smoking. 10:40 Okay, so pneumonia can be classified or categorized into so many different 10:45 types. 10:45 One way it can be categorized is into the areas of lung affected. 10:51 It can affect one lobe. 10:53 This pneumonia is called lobon pneumonia. 10:56 In lobon pneumonia, we see consolidation of a lobe. 11:01 Or pneumonia can affect patches throughout the respiratory tract. 11:06 This is called bronchon pneumonia. 11:09 There is also multi-lobon pneumonia and interstitial pneumonia, which I have 11:13 not added here for 11:14 simplicity. 11:16 So the two types we will look at are lobon pneumonia and bronchon pneumonia. 11:22 Let us look at lobon pneumonia first. 11:25 So again, if we were to look at the alveoli, we see fluid-filled spaces that 11:31 move from 11:31 alveoli to alveoli until it occupies the whole lobe, essentially. 11:37 Lobon pneumonia affects a section of a lobe of the lung. 11:42 It starts distally and spreads throughout the lobe of the lung. 11:48 There is a staging for lobon pneumonia and it can be divided into four stages. 11:55 First is congestion, red hepetization, gray hepetization and resolution. 12:02 So congestion is congestion. 12:04 Red hepetization is a red liver type appearance. 12:08 Gray is a gray type appearance in pathological terms, and then resolution is 12:14 just it resolves. 12:15 So these are essentially staging of lobon pneumonia based on pathological view. 12:25 So if we were to do a physical examination on a patient who has consolidated 12:32 lobe, so 12:33 congested lung, we would most likely find the following things, a decrease in 12:40 chest 12:41 expansion on the affected side, that side of the lung consolidation is dull to 12:50 percussion, 12:51 and we can also hear bronchial breath sounds and also include vocal resonance. 12:59 Now let us look at bronchon pneumonia. 13:02 As we know, it affects patches throughout the lungs, starting with the bronch 13:06 ials, hence 13:07 the name bronchon pneumonia. 13:09 So the problem of congestion begins from the bronchials and moves towards the 13:14 alveoli. 13:14 So whereas low bar pneumonia begins alveoli and moves proximally, bronchon 13:21 pneumonia begins 13:23 proximally and then moves distally towards the alveoli. 13:29 N pneumonia affects patches throughout both lungs. 13:32 Infections spread along airways and finally reaches distal areas. 13:36 So that was looking at lobon pneumonia and bronchon pneumonia, which are two 13:44 types of 13:45 pneumonia based on the areas of lung affected. 13:50 So now we will look at how we can assess the severity of a person, a patient 13:55 with pneumonia, 13:56 and when to hospitalize them. 13:59 So when to hospitalize a patient, we will be specifically looking at community 14:03 acquired 14:04 pneumonia, but it can be, honestly, any type of pneumonia, I think. 14:09 So when to hospitalize patients, we use a score called the CURB65 or CORB in 14:16 Australia 14:17 or PSI. 14:19 We will be looking at CURB65 and each of these letters stand for something we 14:25 are trying 14:25 to find. 14:27 So C is for confusion, U is for urea over 7 millimoles per liter, R is for 14:33 respiratory 14:34 alkalosis and B is blood pressure lower than 90 systole. 14:40 In Australia, we use CURB, so it's the same thing, confusion, but instead of u 14:45 rea, we 14:45 use oxygen less than 90 percent, so hypoxemia. 14:52 R is for respiratory rate greater than 30, so tachypneic and blood pressure is 14:57 the same. 14:59 So each one of these are given a score of one point. 15:03 So if we tally up these points and if it is greater than 2, the patient needs 15:06 to be hospitalized, 15:08 that's basically it. 15:10 Another factor to consider is if the patient is older than 65, this would 15:14 indicate the 15:15 patient would most likely need hospitalization. 15:22 Thank you.