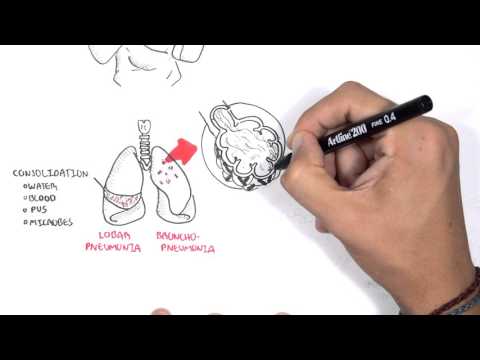
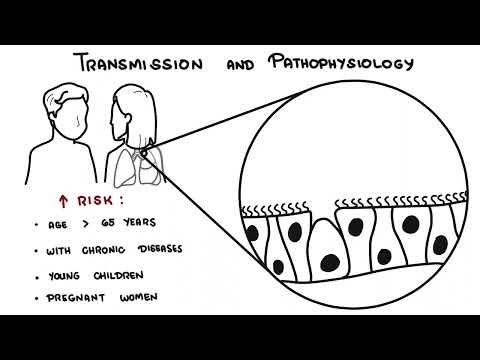
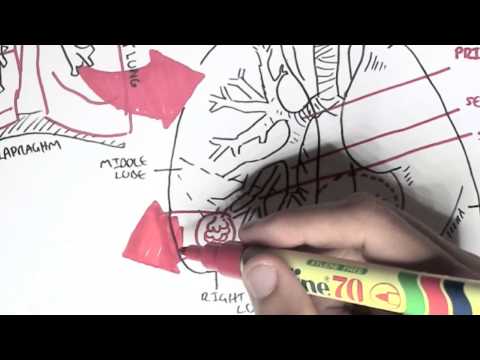
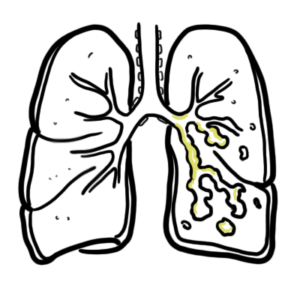
0:00 So here we have the human respiratory tract, the lungs. 0:20 And here is the inferior vena cava descending aorta, the pulmonary arteries and 0:25 the trachea 0:26 and behind the trachea es esophagus. 0:32 Again the causative agents are mainly the bacteria, virus and fungi. 0:36 And these causative agents can cause pneumonia just by being inhaled into the 0:40 lungs, through 0:41 the nose or mouth. 0:44 And they can cause an infection if we have a bad pulmonary defense as we have 0:50 learned. 0:51 But there are ways of transmission, aside from being inhaled into the lungs. 0:58 So the first one is essentially inhalation of infected aerosols, two can be 1:04 aspiration 1:05 of organisms that colonize the oropharynx, three can be aspiration of stomach 1:12 content, 1:13 they can also be hematological spread through the, from the inferior vena cava 1:17 or superior 1:18 vena cava, for example, such as from the, such as, such as spread from a hand 1:24 infection 1:25 or kidney infection. 1:26 So basically pneumonia is a secondary infection. 1:30 They can also be direct inoculation as a way of transmission. 1:35 So we categorize pneumonia before into the areas of lung affected, which is 1:40 into low bar pneumonia 1:42 and bronchine pneumonia. 1:43 But we can also categorize pneumonia into the location where the infection was 1:48 acquired, 1:49 as well as the cause of infection, such as aspiration pneumonia, and also the 1:53 severity, 1:54 chronic pneumonia. 1:56 So the types of pneumonia that we will look at, as well as its causative agents 2:00 are the 2:00 community acquired pneumonia, nosocomial pneumonia, aspiration pneumonia and 2:05 chronic 2:06 pneumonia. 2:07 Let us begin with a community acquired pneumonia. 2:13 Community acquired pneumonia is mostly bacterial viral. 2:16 It's often bacterial infection following an upper respiratory tract infection 2:20 of a viral 2:21 origin. 2:23 Causative agents include streptococcus pneumonia, chemophilus influenza, morax 2:27 cella, carolis, 2:30 as well as influenza virus and RSV. 2:38 Now nosocomial pneumonia, also known as the hospital acquired pneumonia, nosoc 2:43 omial 2:44 pneumonia is pneumonia that is not incubating at the time of admission to the 2:50 hospital and 2:51 develops in a patient hospitalized for longer than 48 hours. 2:55 So essentially it's pneumonia, the lung infection after being admitted to 3:02 hospital. 3:03 So it's a causative agent is from the hospital. 3:06 And these causative agents can be the enterobacteria, pseudomonas species, as 3:11 well as staphococcus 3:12 aureus, also taking into account methicillin-resistant staphylococcus aureus. 3:22 Now aspiration pneumonia, which is also very common in hospital settings. 3:27 So it can be kind of under nosocomial pneumonia. 3:30 But aspiration pneumonia occurs in markedly debilitated or in unconscious 3:35 patients or 3:36 during vomiting, when the patient's vomiting, because they can aspirate stomach 3:41 content 3:41 with gut, with bacteria. 3:44 So aspiration pneumonia often leads to abscess formation, which is bad. 3:49 So let's take a closer look at complications with abscess formation in the 3:55 lungs. 3:56 So lung abscess complications. 3:58 So when you develop a lung abscess from aspiration pneumonia, there can be 4:02 complications such 4:03 as extension to the, it can extend to the plural cavity. 4:08 You can have hemorrhage. 4:09 You can develop brain abscess, meningitis, if it travels, if it can travel 4:14 through the 4:15 blood to the brain, you can also develop secondary amylidosis. 4:21 Now, so back to aspiration pneumonia. 4:27 Aspiration pneumonia usually occurs in the right lung because of the anatomical 4:33 variation. 4:34 So the right lung, it has a wider, essentially, high lung and it's often more 4:41 vertical. 4:42 And so things can get into the right lung, easier. 4:46 Causative agents of aspiration pneumonia include streptococcus and staphylococ 4:50 cus ores and 4:52 also gram negative species from the, gram negative bacteria from the 4:57 gastrointestinal tract. 4:59 Lastly, we will look at chronic pneumonia and it's usually involving fungus, 5:05 fungal, 5:05 causative agents, and occurs usually in immunocompromised patients. 5:11 All things for chronic pneumonia, histoplasmosis, tubericalosis, aspergillus, 5:18 as well as no cardia. 5:20 Okay, so those are the four types we looked at. 5:26 Community acquired, nosocomial, aspiration, and chronic pneumonia. 5:32 And there can be complications of pneumonia. 5:35 These are abscess formation as we have just talked about because it's dangerous 5:40 . 5:40 Abscess formation leads to tissue destruction amongst many other things. 5:46 Emphyema, as well as bacterium dissemination. 5:51 So it can cause complications of pneumonia, it can cause essentially sepsis. 5:56 Okay, so when a patient presents with signs and symptoms of a lung infection, 6:03 it is important 6:04 to perform investigations, to rule out certain things and to, you know, 6:08 diagnose pneumonia. 6:10 So, things that we can do, chest x-ray, we can see and potentially diagnose the 6:15 type of 6:16 pneumonia using a chest x-ray according to where it affects the lungs. 6:22 It can be consolidation to a lobe, it can be consolidated to a lobe, or termed 6:28 lobe 6:28 on pneumonia, or it can be patchy like bronchon pneumonia. 6:32 Another investigation is sputum testing, gram stain, to identify the bacteria 6:37 using microscopic 6:40 culture and sensitivity testing. 6:43 You can also perform urine antigen testing to identify the bacteria, streptococ 6:46 cus pneumonia, 6:47 or lesionella, in case it has spread or is a result of a UTI. 6:55 For blood testing, full blood count, for example, wide blood cells are up or 7:01 down, which will 7:02 indicate severity, utrophilia is indicative of bacterial infection. 7:09 You can also have hemolytic anemia, which suggests microplasma as a causative 7:15 agent. 7:16 E, electrolyte urea creatinine testing. 7:20 Urea high indicates the severity. 7:23 Liver function tests, you can also perform, and it's abnormal if the base of 7:28 the pneumonia 7:29 inflames essentially the liver. 7:34 So the lower portion of the lung inflames the liver. 7:37 You can also perform blood culture for bacteria involvement. 7:41 So if it's bacteria, bacteria, it's pretty severe because it can lead to sepsis 7:48 . 7:49 So next is the management and treatment of pneumonia. 7:52 So here we have a patient with pneumonia, oxygen. 7:57 All patients with tachynesia, hypoxemia, hypertension, and acidosis requires 8:03 oxygen. 8:04 Before looking at the other management, it's important to recap or know the 8:09 cardinal signs 8:10 of pneumonia. 8:11 So we know the signs and symptoms, but the cardinal signs of pneumonia again, 8:15 if you 8:15 can remember, we can remember it as C-D-E-F. 8:19 So C stands for chest pain, D stands for dysnia, E stands for exudate, sputum, 8:25 and F is for 8:26 fever. 8:27 Okay, let's continue with the management. 8:29 So number one, oxygen, two intravenous fluids for severe patients, elderly, and 8:34 those who 8:35 are vomiting, three, we use pain management. 8:41 Insads are usually sufficient, but opioids can be used, but it can be dangerous 8:46 because 8:47 it can lead to respiratory depression, but if it's monitored, it's good. 8:54 Four, use of antibiotics. 8:56 So use of antibiotics can be complicated. 9:00 So essentially, you don't know the causative agent, so you have to do empirical 9:07 therapy. 9:08 When performing empirical therapy, it's important to look at a few factors. 9:13 These are what is the most likely pathogen, the risk for antimicrobial 9:18 resistance, and 9:20 if the person has any medical comorbidities or allergies. 9:26 So the use of empirical therapy is different for, you know, nosocomial, for 9:33 risk community, 9:35 for aspiration, for all the different types of pneumonia, it's usually 9:39 different. 9:40 Some overlap. 9:42 So the use of empirical therapy for community-acquired pneumonia are used two 9:46 things. 9:47 Number one, are beta lactams, such as your penicillins, which will help you 9:51 target your 9:52 gram-positive bacteria. 9:55 The second one, you can use macrolides, which are your myosins. 10:00 Macrolides can help you target your gram-negative bacteria. 10:03 Of course, this is simplistic in that macrolides can also target your gram- 10:08 positive, but essentially 10:10 what you're doing with empirical therapy is that you are trying to cover the 10:16 most likely 10:17 causative agent being the bacteria. 10:23 Of course, it might not be a bacteria, it might be a virus, and so you have to 10:27 perform 10:28 further investigations until you find the causative agent. 10:32 But this is, the empirical therapy is important so that it can cover the main 10:38 culprits, the 10:39 bacteria, if they are the cause. 10:42 So how do these antibiotics work? 10:45 Well, here we're looking at a bacteria with its DNA, its green, but we don't 10:51 know what 10:52 bacteria it is, so we use empirical therapy. 10:55 So firstly, let's look at beta lactams. 10:59 Now beta lactams, essentially what they do is they target the cell wall of the 11:04 bacteria, 11:05 which is essentially a made up of peptidoglycan. 11:10 The beta lactams used for pneumonia include amoxicillin and flu coccycillin, 11:17 specifically 11:19 targeting staph species. 11:31 So in the bacteria, bacteria make proteins all the time. 11:34 Acrylides inhibit this process. 11:38 Macrylides including clathromycin and erythromycin are used. 11:45 After you use empirical therapy, the causative agent might be identified 11:49 following investigations 11:51 such as your blood cultures, your x-rays or whatever. 11:57 And so after you've identified the causative agent, and if it is a bacteria and 12:01 you know 12:02 what type of bacteria it is, you have to change your antibiotic that will 12:05 specifically target 12:06 that bacteria. 12:09 Hope that made sense. 12:11 Now just in summary, for uncomplicated community acquired pneumonia, you use 12:17 oral antibiotics, 12:19 but for complicated pneumonia, community acquired pneumonia, you will use IV 12:25 intravenous antibiotics 12:26 so that it can get into the system faster. 12:29 Hope you enjoyed this video on pneumonia, thank you for watching.