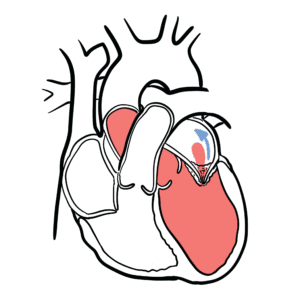
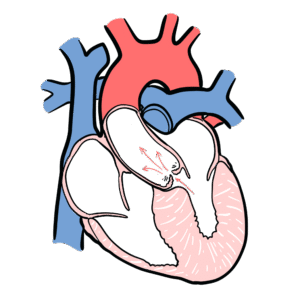
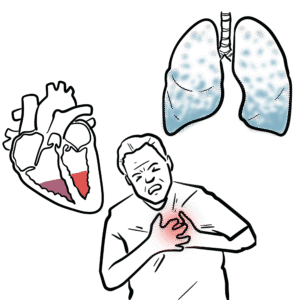
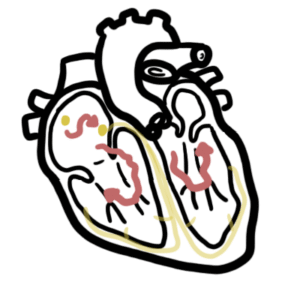
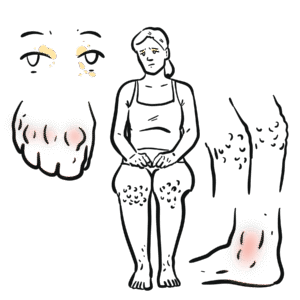
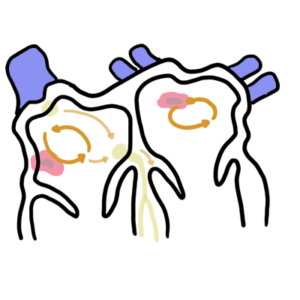
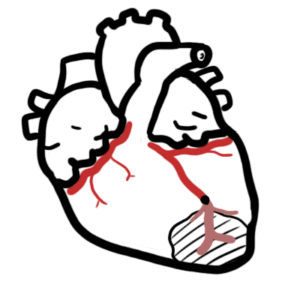
0:00 In this video we are going to look at pericarditis. 0:08 This is an overview and introduction. 0:11 Pericarditis is inflammation of the pericardia. 0:15 Pericarditis can be either fibrous, dry, or effusive, with perlite, serous, or 0:21 hemorrhagic 0:22 exudate. 0:23 The triad of signs for pericarditis include chest pain, pericardial friction 0:30 rub, and 0:31 serial ECG changes. 0:34 Pericarditis accounts for up to 5% of presentations to the emergency department 0:42 for chest pain. 0:43 The pericardium is a membrane that surrounds the heart. 0:51 Here is the heart muscle, the cardiomyocyte. 0:56 The layers of the pericardium include the visceral, parietal, and outer fibrous 1:02 layer. 1:03 Between the visceral and parietal layer is the pericardial space, or cavity. 1:13 In pericarditis there is inflammation of the pericardium, which results in 1:18 narrowing of 1:19 the pericardial space, and possibly some scarring. 1:23 If pericarditis persists and is not treated, pericarditis can lead to pericard 1:29 ial effusion, 1:30 which is a complication. 1:32 Pericardial effusion is when the pericardial space is filled with extra fluid. 1:37 The extra fluid exerts pressure on the heart muscles, resulting in cardiac 1:43 dysfunction. 1:45 The signs and symptoms of pericarditis include fever, myalgia, chest pain, tri- 1:52 putting position, 1:54 which relieves the pain, and signs of right-sided heart failure, including a 2:00 raised JVP, and 2:02 peripheral edema. 2:08 Risk factors, male gender, age between 20 to 50, systemic autoimmune disease, 2:15 having a 2:16 viral and bacterial infection, past and recent cardiac surgery, having had a 2:25 transmural myocardial 2:27 infoxion, and having uremia or being on dialysis. 2:35 Meditations for suspected pericarditis include ECG, which may show global ST 2:41 elevation and 2:42 PR segment depression, serum troponin, ESR, C-reactive protein, full blood 2:51 count, and 2:52 serum urea. 2:54 An echocardiogram is important in ruling out differentials and checking for per 2:59 icardial 3:00 effusion and pericardial damage. 3:03 Performing an X-ray may show a bottle of water shaped enlarged cardiac 3:07 silhouette, which 3:08 is a sign of pericardial effusion. 3:16 The management of pericarditis is to perform pericardio-syntesis if there is 3:22 presence of 3:24 cardiac tamponade or symptomatic pericardial effusion. 3:29 Inpericarditis, inflammation occurs because arachidonic acid is formed through 3:36 phospholipids 3:38 on cell membranes. 3:39 The arachidonic acid produces prostaglandins and thromboxin A2, with the enzyme 3:46 COX. 3:47 These molecules contribute to the fever, pain, and inflammation in pericarditis 3:53 . 3:53 Therefore, the management of pericarditis, NSAIDs, nonsteroidal anti- 3:59 inflammatory drugs 4:00 are useful because they inhibit COX and so stop the inflammatory process. 4:08 However, a side effect of nonsteroidal anti-inflammatory drugs is peptic ulcers 4:14 , and so proton pump 4:16 inhibitors also need to be administered to prevent peptic ulcer formation. 4:22 In recurrent pericarditis, patients can go on nonsteroidal anti-inflammatory 4:28 drugs, proton 4:28 pump inhibitors, plus mitus cultucine, which is common med for gout, and plus 4:35 minus corticosteroids 4:37 for serious cases. 4:41 Complications of pericarditis include pericardial effusion, which we mentioned 4:47 earlier. 4:47 Pericardial effusion can become cardiac tamponade once the fluid builds up and 4:53 becomes so bad 4:53 that it impairs the heart's contractility. 4:57 Another complication can be chronic constrictive pericarditis.