Atrial Fibrillation
Atrial fibrillation, AF is a chaotic, irregular atrial rhythm at 300-600bpm; the AV node responds intermittently, hence an irregular ventricular rate. AF is the most common sustained dysrhythmia; characterised by absent P waves, irregularly irregular heart rate, narrow QRS (typically). It is common in the elderly. The main risk of AF is embolic stroke either in the mesenteric artery, brain tissue or limb extremities.
Supraventricular tachyarrhythmia: Arrhythmia arising from the conduction system above the ventricles, possibly the AV node, atria or SA node.
Atrial Fibrillation: A supraventricular tachyarrhythmia. It is characterised by uncoordinated atrial activity on the surface ECG, with fibrillatory waves of varying shapes, amplitudes, and timing associated with an irregularly irregular ventricular response when atrioventricular (AV) conduction is intact.
Acute Atrial Fibrillation: Defined as a new onset or a first detectable episode of AF, whether symptomatic or not.
Chronic Atrial Fibrillation: is defined as experiencing atrial fibrillation more than once. It may be paroxysmal, persistent, long-standing persistent, or permanent.
The cardiomyocytes contract moving blood around and out of the heart. Many factors affect cardiac output, one of which is heart rate.
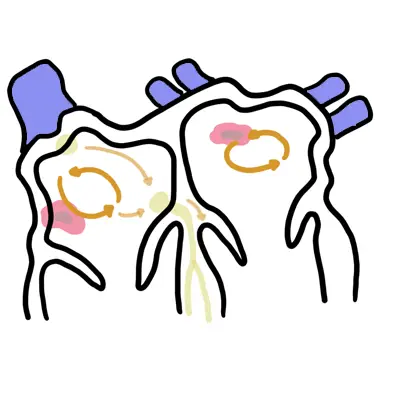
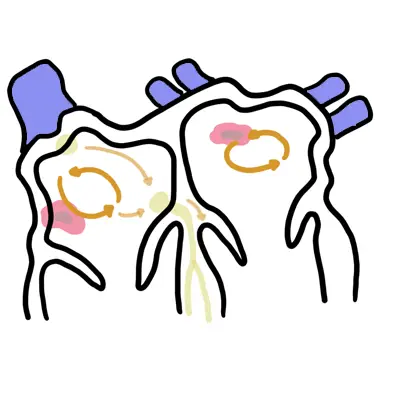
Conduction system The heart rate is controlled by the heart’s own special conduction system. The Sino atrial node (SAN) is the boss and sits high in the lateral right atrium (RA) just below the superior vena cava. The SAN is richly innervated with sympathetic and parasympathetic fibres, which alter the rate of depolarization hence controlling the heart rate. This is also the same for the Atrioventricular node which is found in the RA anterior to the mouth of the coronary sinus and directly above the insertion of the septal leaflet of the tricuspid valve. The AV node then sends conduction signals to down to the ventricles through the his-purkinje system.
Three clinical patterns (3Ps) All patterns have a risk of thromboembolism.
Chronic AF is having atrial fibrillation more than once. It may be paroxysmal, persistent, long-standing persistent, or permanent.
Clinical Presentation
Atrial fibrillation may cause chest pain, palpitations, dyspnea, or faintness. Signs include irregularly irregular pulse and possible signs of left ventricular heart failure. 30% of patients present with AF as an incidental finding only
AF may be associated with non-cardiac disease (ie. pneumonia and hyperthyroidism).
Examination
Palpitations
Wolff-Parkinson-White syndrome is a condition in which there is an extra electrical pathway in the heart (accessroy pathway). The condition can lead to periods of tachycardia.
ECG shows absent p waves, irregularly irregular rhythm, QRS (typically narrowed). Rate is usually about 150bpm
The treatment of atrial fibrillation needs to be considered under three seperate headings:
Haemodynamically unstable AF
Acute AF but haemodynamically stable
Chronic AF – ongoing management
Warfarin (international normalized ratio (INR) >2) reduces strokes in AF by 60%, regardless of underlying risk.
| CHADS2 Scoring system to assess risk of stroke in AF (nonvalvular) | |
| 1 point each | 2 point each |
| Congestive Heart Failure | Stroke or TIA previously |
| Hypertension | |
| Age >75yo | |
| Diabetes | |
| CHA2DS2 – VASc Scoring system to assess risk of stroke in AF (nonvalvular) | |
| 1 point each | 2 point each |
| Congestive Heart Failure | V |
| Hypertension | Age >75 |
| Age >65yo | Stroke or TIA previously |
| Diabetes | c |
| Sex – female | |
| Vascular disease | |
Warfarin is an anticoagulant. It is used for AF, valvular heart disease and pulmonary embolism. Mechanism of action: Vitamin K antagonist inhibiting the production of coagulation factors VII, IX, X (these require Vitamin K to be produced). Side effects: Allergy, acute bleeding. When bleeding occurs as a result of warfarin this can be reversed by administering Vitamin K.
Digoxin is used for Heart failure and AF. Digoxin works by inhibiting the Na/K+ pump in cardiomyoctyes, this causes ↑intracellular Na+ together with Ca+ causes stronger contractions at a slower rate. Side effects: Nausea, vomiting, headache, dizziness/vertigo, loss of appetite, diarrhea, Digoxin toxicity (arrythmias).
Amiodarone is a K+ channel blocker (class III antiarrythmic). It acts on the myocardium to delay repolarization and increase duration of the action potential. It also decreases SA and AV conduction rate. Side effects (6Ps): Prolongs action potential duration, Photosensitivity, Pulmonary fibrosis and inflammation, Pigmentation of skin, Peripheral neuropathy, Peripheral conversion of T4 to T3 is inhibited (Hypothyroidism, but it also can cause hyperthyroidism).
Complications
6Ps of Amiodarone side effects (6Ps): Prolongs action potential duration, Photosensitivity, Pulmonary fibrosis and inflammation, Pigmentation of skin, Peripheral neuropathy, Peripheral conversion of T4 to T3 is inhibited (Hypothyroidism).
Prognosis depends on several factors, such as the precipitating event, underlying cardiac status, risk of thromboembolism, and whether the nature of the AF is paroxysmal, persistent, or permanent.
UpToDate
Best Practice
Oxford Handbook of Cardiology

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion