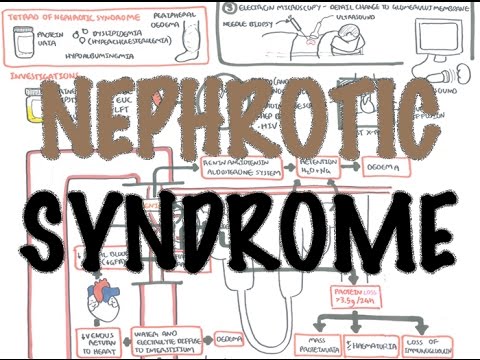
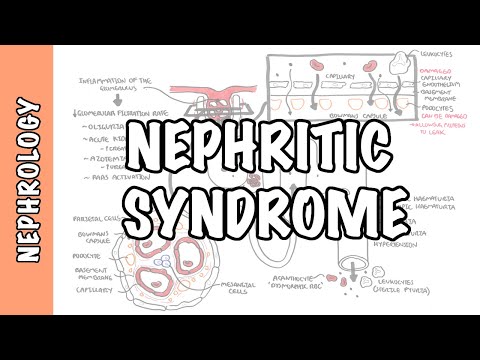
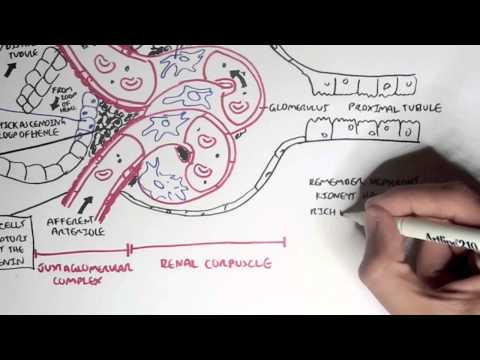
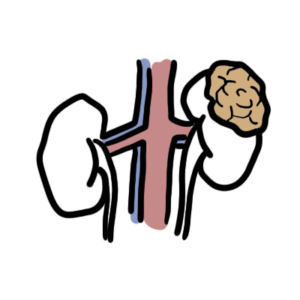
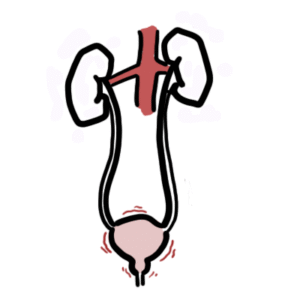
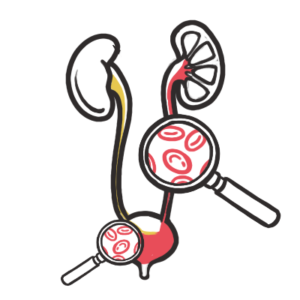
0:00 Hello, in this video, we're going to talk about glomerular nephritis and we are 0:19 focusing 0:20 on nephrotic syndromes. 0:22 Remember, nephrotic syndrome is where you have the classic triad of signs and 0:27 symptoms, 0:28 which is hypercholesterolemia, hypo albuminemia, protein urea, greater than 3.5 0:38 grams in 24 0:39 hours, and peripheral edema. 0:43 This is all a result of kidney damage, specifically the damage to the 0:49 functional units of the 0:51 kidneys called nephrons. 0:53 Now the damaged nephrons usually filter things out to make up urine. 1:00 This urine contains, unfortunately, the unwanted proteins and sometimes blood 1:07 hematuria. 1:08 The site that is damaged in nephrotic syndrome is at the head of the nephron, 1:13 where blood 1:13 vessels go to, to filter things into the tubule part of the nephron, and this 1:21 area is called 1:22 the glomerulus. 1:23 So here is the tube of the nephron, the bowman's capsule, which is the head of 1:28 the nephron. 1:29 The glomerulus is a group of vessels that come from the afferent arterial, 1:35 which is 1:36 bringing blood into the nephron, and the blood vessels leaving the nephron is 1:40 the efferent 1:41 arterial, which later will essentially form the renal vein. 1:48 To understand nephrotic syndrome and the different types, we need to revise the 1:53 anatomy of the 1:54 head of the nephron. 1:57 So let us cut a cross section of the glomerulus and the bowman's capsule. 2:02 To orientate ourselves, the head of the nephron itself is made up of special 2:08 cells called 2:09 cryotal cells, and these are essentially squamous epithelial cells, which forms 2:15 the bowman's 2:16 capsule. 2:18 In the bowman's capsule is the glomerulus, the group of blood vessels that are 2:23 all lined 2:24 up together. 2:26 The vessels are made up of fenestrated endothelium, which allow for filtration. 2:35 Putting the fenestrated endothelium is the glomerular basement membrane. 2:40 Then surrounding the basement membrane are cells called podocytes, with their 2:46 foot projections. 2:49 The podocytes are important because in a way they help with the filtering 2:56 process. 2:57 They help by maintaining the integrity and structure of the glomerulus. 3:03 Then of course, around the vessel, around the podocytes, you have the bowman's 3:09 capsule, 3:10 which houses the glomerulus. 3:14 So you can say the deepest layer is the fenestrated endothelium of the vessel, 3:22 which contains within 3:24 it the blood and other blood stuff. 3:27 And moving out to the next layer we have the glomerular basement membrane, or G 3:34 BM. 3:34 Then we have the podocyte and its foot projections, the bowman's capsule, and 3:40 finally the pryotal 3:41 cells that houses the glomerulus. 3:46 Let us pull one of these vessels out, and as you can see, the podocytes are 3:51 surrounding 3:52 it with the foot projections. 3:55 Then below it is the glomerular basement membrane, and then the fenestrated 4:00 endothelium, the most 4:02 inner layer. 4:04 And within the blood vessel we can find proteins and we can find red blood 4:11 cells. 4:12 Another important cell in this area are the mesangial cells, here in blue, 4:17 which you can 4:18 think of as contractile cells that help regulate the blood flow in the area. 4:24 In some nephronic conditions these cells are affected. 4:30 Let us now look at a section of the glomerulus, and see the layers again in a 4:35 different view. 4:40 So normally you have the fenestrated endothelium here. 4:44 Above it, again, is the glomerular basement membrane, then you have the pod 4:50 ocytes and 4:51 the surrounding bowman's capsule. 4:55 Red blood cells and other proteins around this area cannot get filtered. 5:00 Red blood cells cannot get filtered because they are way too big for the capill 5:06 aries. 5:06 The fenestrated endothelium. 5:08 The proteins cannot get filtered because one, they are still too big, and two, 5:14 the podocytes 5:15 prevent protein from passing through. 5:18 The podocytes does this because it has negatively charged surface, which repels 5:23 the negatively 5:25 charged protein ions. 5:35 In nephrotic syndrome there is essentially injury to the podocytes due to many 5:41 reasons, 5:42 mainly either from immune-complex deposition or complement protein activation, 5:49 which leads 5:50 to subsequent damage. 5:52 The proteins that are not usually able to pass through this, these layers, can 5:57 now pass 5:58 through towards the bowman's capsule and into the tubule, leading to protein 6:05 uria. 6:06 Sometimes blood can even get through if the damaged area also includes the gl 6:11 omerular 6:12 invasive membrane and capillaries. 6:16 So that was an overview of what happens in nephrotic syndrome. 6:21 You have immune-complex and complement proteins leading to damage to the pod 6:26 ocytes, which 6:28 normally would prevent protein from getting through. 6:32 But there are different types of nephrotic syndromes, and these types of neph 6:36 rotic syndromes 6:37 can be divided into primary or secondary nephrotic syndromes. 6:43 The main primary nephrotic syndromes are minimal-change disease, membranous gl 6:48 omerular nephritis, 6:50 and focal segmental glomerular sclerosis. 6:55 Secondary nephrotic, as the name suggests, occurs because of another disease or 7:01 another 7:01 cause. 7:03 Common examples include systemic lupus erythmatosis, diabetic nephropathy, amyl 7:11 oidosis, hepatitis 7:13 B, hepatitis C, and HIV. 7:17 If there is an exam question, "What is the most common cause of chronic kidney 7:22 disease?" 7:22 The answer is diabetic nephropathy. 7:26 If there is a question, "What is the most common nephrotic syndrome?" 7:30 The answer is diabetic nephropathy. 7:35 Diabetic nephropathy will be hopefully discussed in another video, but it's 7:38 very important 7:38 to be aware of this condition. 7:41 We will focus on primary nephrotic syndromes, beginning with minimal-change 7:46 disease. 7:47 Minimal-change disease causes the majority 70-90% of nephrotic syndrome in 7:55 childhood. 7:57 Eliminal biopsy shows minimal change in light microscopy, hence the name. 8:03 Immunofluorescence shows occasional IgM immunoglobulin in the mesangium. 8:11 Electron microscopy shows a facement of podocyte foot processes and cells. 8:19 So here we have the capillary vessel, the glomerular basement membrane, and the 8:24 podocyte 8:24 effacement, and you can see loss of foot projections. 8:30 The loss of foot projections allows protein from the glomerulus to be filtered 8:35 through 8:36 and enter the bromase capsule and into the tubule. 8:41 Next, membranous glomerular nephritis. 8:44 It accounts for 30% of nephrotic syndromes in adults. 8:54 Renal biopsy shows in light microscopy, mesangial expansion, and capillary wall 9:02 thickening. 9:04 Immunofluorescence shows IgG and complement 3 protein. 9:11 Electron microscopy will reveal glomerular basement membrane thickening. 9:16 So drawing it out, again here we have the endothelial wall and surrounding it a 9:22 thick 9:23 glomerular basement membrane. 9:25 Then surrounding the glomerulus, there are subepithelial deposits of immunocom 9:32 plexes formed 9:33 by, as mentioned, complement 3, C3, and IgG. 9:39 These are termed spikes because they look like spikes on electron microscopy. 9:45 So they deposit here, filling in the spaces within the glomerulus, forming 9:52 these spikes. 9:53 The immune deposits actually damages the podocytes and the foot projections. 10:00 And because there's damaged podocytes, proteins that were previously unable to 10:05 pass through 10:06 are filtered through from the glomerulus into the bromase capsule and into the 10:11 nephron's 10:11 tubule. 10:13 The last type of primary nephrotic syndrome we're going to talk about is focal 10:18 segmental 10:19 glomerular sclerosis. 10:22 Renal biopsy, the light microscopy will show focal segmental sclerosis of the 10:28 glomerulus. 10:29 Immunofluorescence will really not really show anything. 10:33 And electron microscopy can reveal glomerular basement membrane thickening. 10:42 When drawing it out, we have a thickened glomerular basement membrane and 10:47 sclerosis of a focal 10:49 area, which actually results after some time in a decrease in your own output 10:55 because of 10:56 the decrease in filtration to parts of the glomerulus. 10:59 Further, the sclerosis can damage surrounding podocytes contributing to protein 11:05 uria. 11:12 You