Inflammatory Bowel Disease


Inflammatory bowel disease is a common condition. It is divided into two types: Crohn disease and Ulcerative colitis. Both these condition differ in pathology, progression and complication, but they do share a lot similar characteristics as well.
Colitis: Inflammation of the colon, which may be due to infectious, autoimmune, ischemic, or idiopathic causes.
Inflammatory Bowel Disease: Autoimmune-mediated intestinal inflammation primarily due to either Crohn disease or ulcerative colitis.
| Ulcerative Colitis | Crohn’s Disease | |
| Both | Gender | Male<Female |
| 2-19/100,000 | Incidence (per year) | 21-20/100,000 |
| 15-40yo | Onset | 15-40yo |
| Distal colon | Location | Dital ileum and caecum |
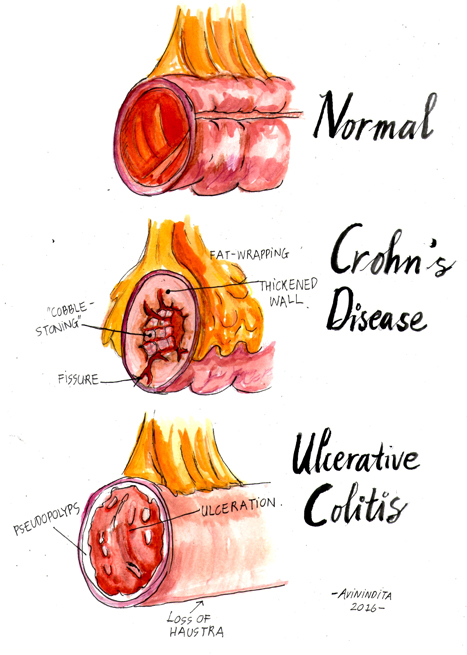
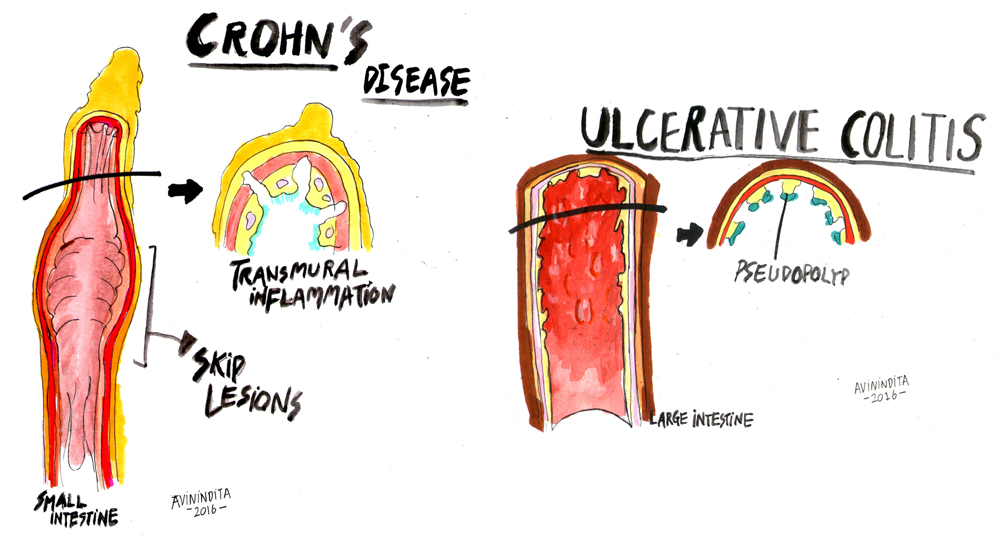
| Continuous superficial inflammatory lesion | Pathology | Discontinuous, patchy transmural inflammatory skip lesions |
| Severe bleeding, toxic megacolon, perforation, colon cancer | Complications | Stenosis, abcess formation, fistula, strictures, colon cancer |
| Risk Factors | |
| Ulcerative Colitis | Crohn’s Disease |
| Family history of inflammatory bowel disease | White ancestry |
| HLA-B27 | Family history |
| Infection | High sugar diet |
| NSAIDs | Oral contraceptive pill, NSAIDs |
| Not smoking or former smoker | Cigarette smoking |
| Not breastfed | |
| ULCERATIVE COLITIS CLINICAL PICTURE | |||
| Proctitis (50%) | Left-sided colitis (30%) | Pancolitis (∼20%) | |
| Area affected | Inflammation of the rectum | Inflammation from rectum up to the splenic flexure | Inflammation of the entire colon |
| Rectum and deification | Rectum always involved. Symptoms of urgency and frequency due to rectal irritablity. | Rectal irritation | |
| Stool | Blood mucus mixed with loose stools (frank bloody diarrhea rare) | Bblood mucus in stools, often leading to diarrhea | Diarrhea |
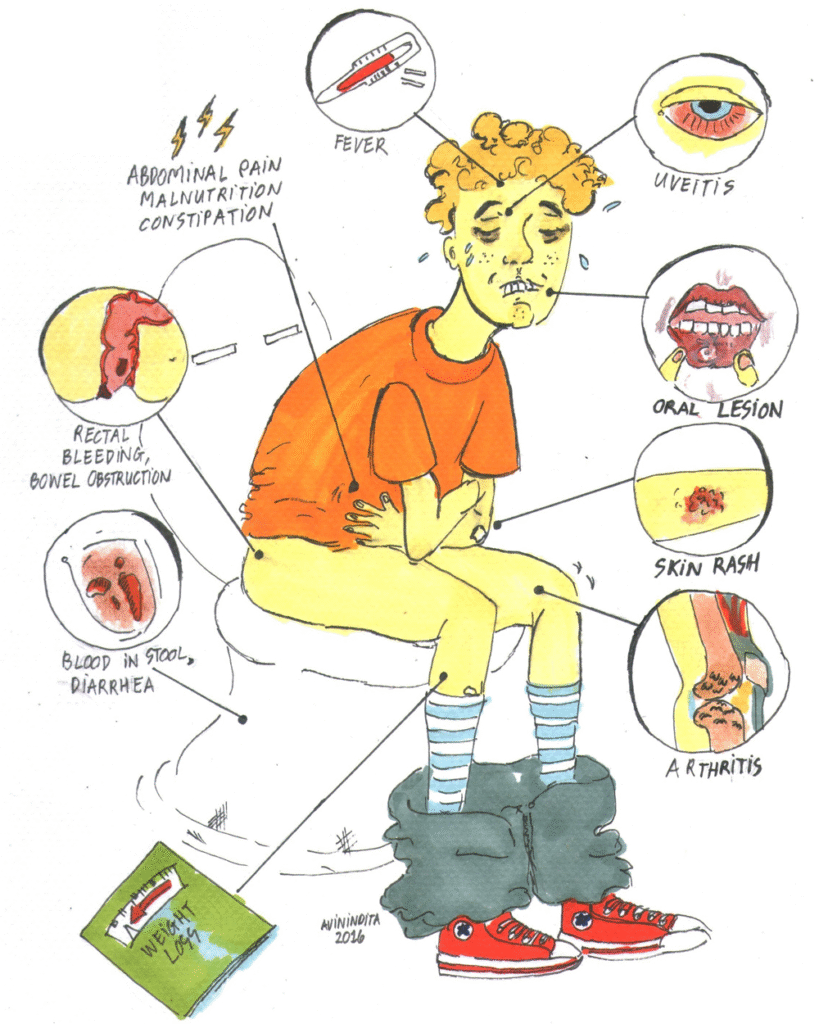
Ulcerative colitis typically presents in young adults with relapsing bloody diarrhoea, malaise, fever and weight loss. Crohn’s can have similar presentation or have a more insidious onset with other complications such as malabsorption and pain.
Extra-intestinal Manifestations
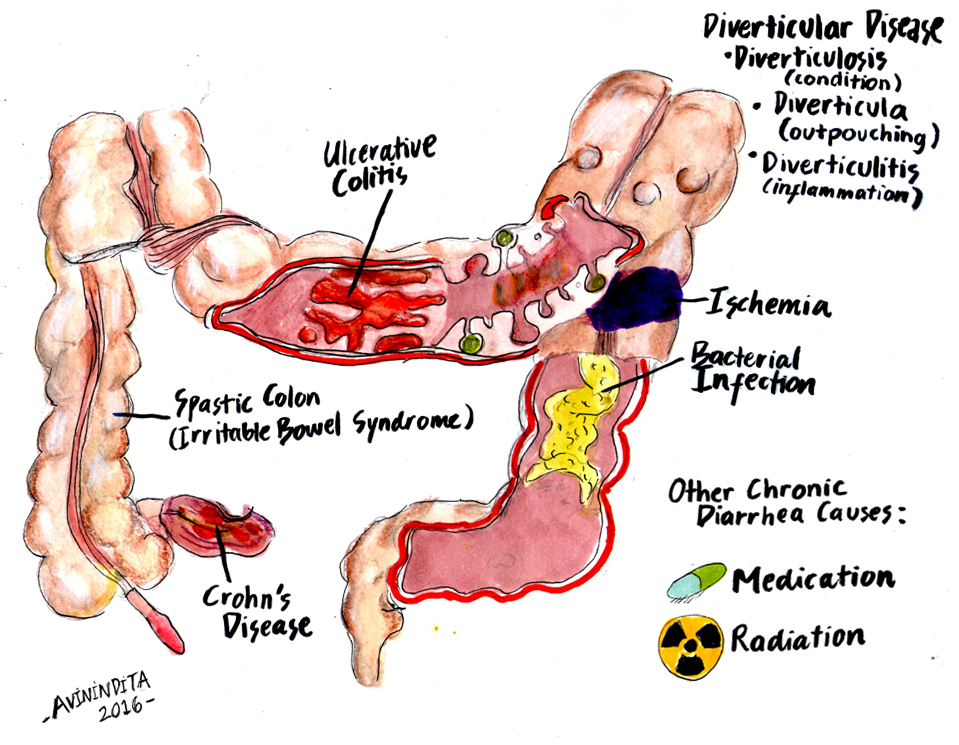
The differential diagnosis of inflammatory bowel disease includes other causes of chronic diarrhoea
Infection must be excluded, and it is necessary to check for infections with organisms such as Entamoeba histolytica, Salmonella, Shigella, E coli, and Campylobacter, as well as Clostridium difficile, which can occur in the absence of prior antibiotic exposure.
Causes of Colitis (inflammation of the colon)
General
Specific for Ulcerative Colitis
Specific for Crohn’s Disease
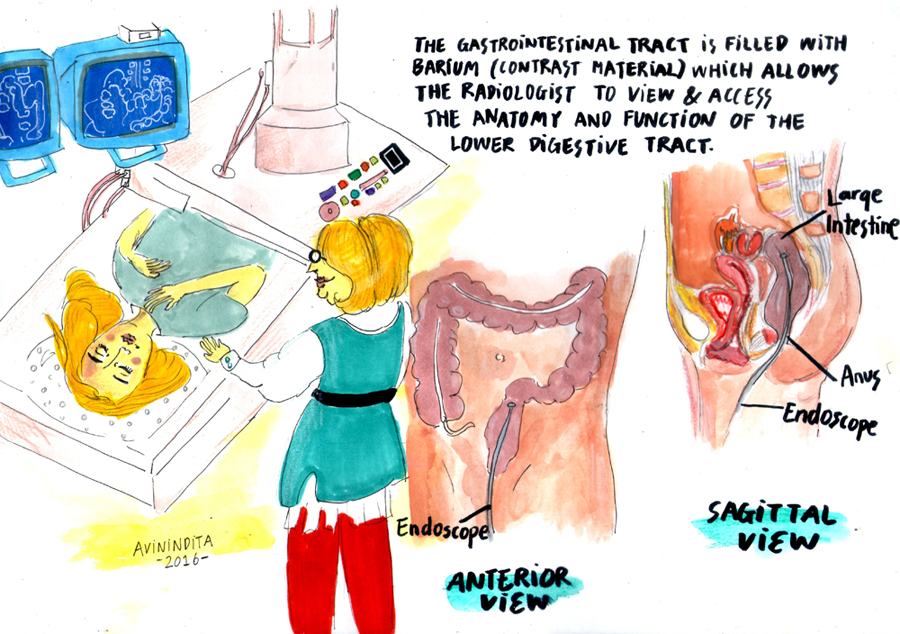
Diagnosis
| Ulcerative Colitis | Crohn’s Disease |
| Superficial inflammation. Disease present in the distal colon and rectum and spread proximally with increasing extend of disease. | Transmural inflammation. Disease commonly focused in the terminal ileum and caecum, but may affect the anus, colon, or entire small bowel. |
| Acute neutrophil infiltration in the mucosa and submucosa | Lymphoid aggregates, particularly in the subserosal tissues (Crohn’s rosary). |
| Mucosal crypt abscess with goblet cell mucin depletion | Mucosal crypt ulceration, and fissuring ulceration. |
| More severe inflammation, there can be aphthous ulcers, granulation tissue -> pseudopolyps | Mucosal thickening and cobblestone. |
| Chronic ‘burnt out’ disease leads to a pale, featureless, ahaustral pattern to the colon. Transmural inflammation may occur in sever cases. | Extensive fibrosis and muscle hyperplasisa may occur, giving rise to stenosis. Perforation, fistulation, and abscess formation are occasional sequelae of transmural inflammation. |
The management differs for UC and CD. CD is more severe and encounters more complications. The principles of medical treatment is to reduce inflammation and prevent complications.
General
| Ulcerative Colitis Medical and Surgical Treatment | |||
| Proctitis (50%) | Left-sided colitis (30%) | Pancolitis (~20%) | |
| Topical steroids (suppsoitories or foam enema) | + | + | + |
| 5-ASA | + | + | + |
| Systemic Steroids (prednisalone) | – | -/+ | + |
| Oral immunosuppressives (azathiopurine) | – | – | + |
| Immunomodulators (anti-TNFa) | – | – | + |
| Surgery is indicated for acute colitis that fails to respond to treatment and for chronic colitis. Surgical treatment include removing parts of bowel or entire colon. | |||
| Crohn’s Disease Medical and Surgical Treatment | |
| Medical Treatment | Surgical Treatment |
| 5-ASA | Acute: Free perforation, sever haemorrhage, acute severe colitis, complete intestinal obstruction |
| Systemic steroids (hydrocortisone, prednisolone) | Subacute: Inflammatory mass, subacute obstruction, abscess formation, symptomatic fistulation |
| Immunosuppressives (azanthiopurine, methotrexate) | Chronic: Steroid dependency or complications, cancer treatment |
| Immunomodulators (anti-TNFa) | |
| Dietary modification | |
Local Complications
Extra-intestinal Manifestations
Because of transmural inflammation, Crohn disease often is complicated by fistula formation.
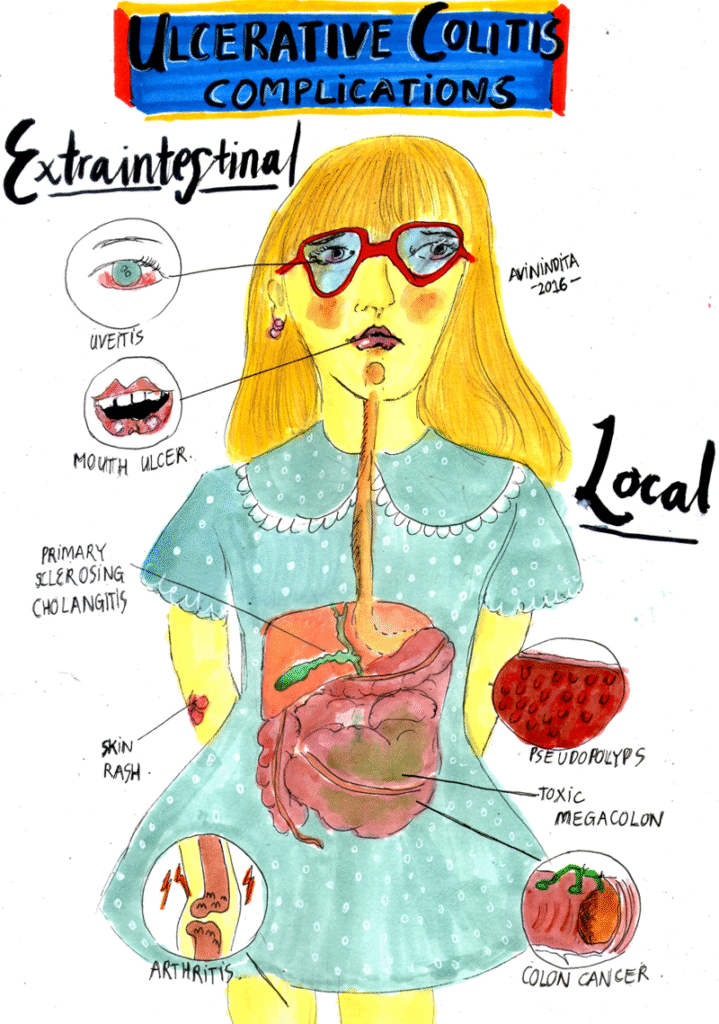
Ulcerative Colitis
Crohn’s Disease
Best Practice
UpToDate
Oxford Handbook of Clinical Surgery
Oxford Handbook of Emergency Medicine
Oxford Handbook of Clinical Medicine

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion