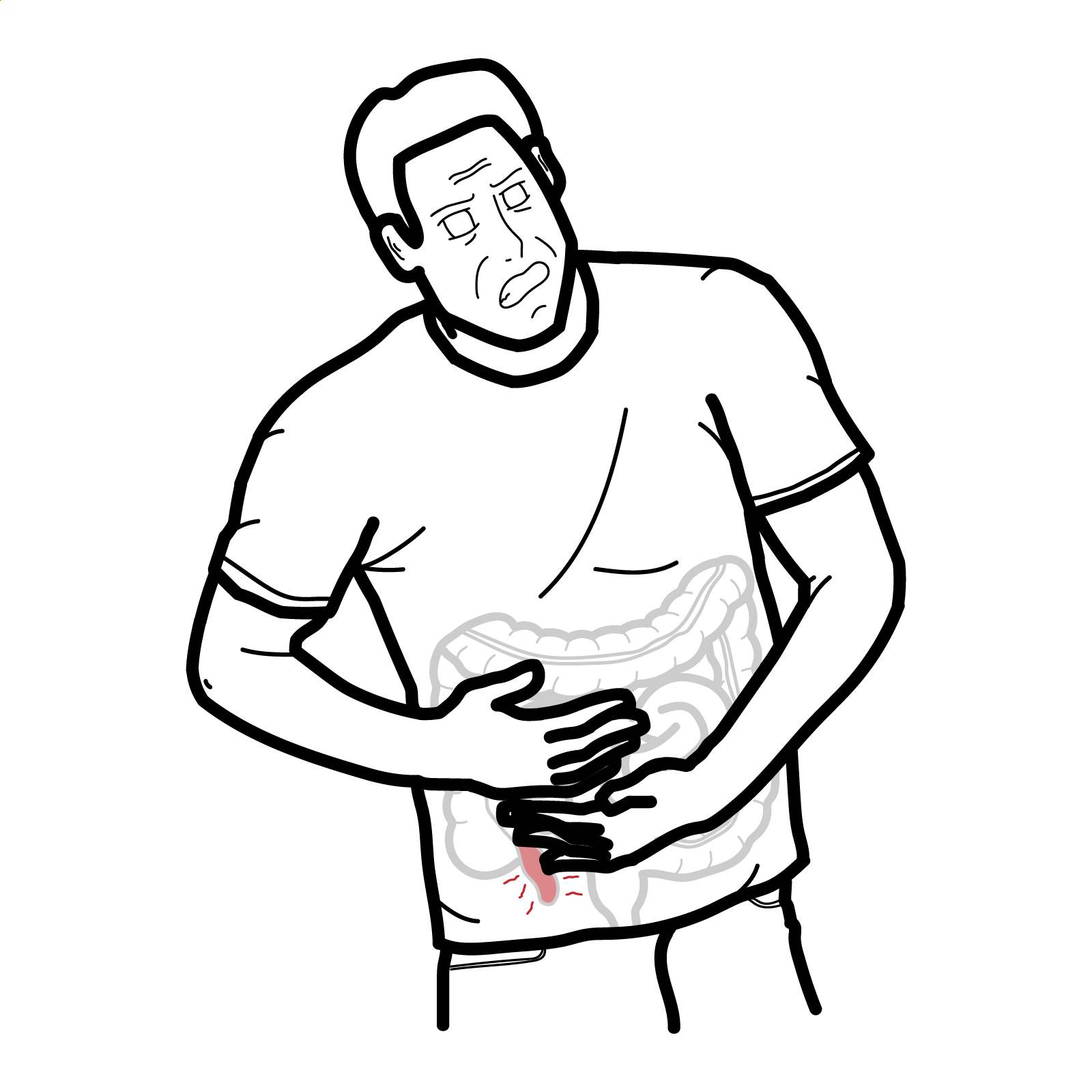
Acute Appendicitis
Acute appendicitis is an acute inflammation of the vermiform (worm-like) appendix. It is mainly caused by obstruction of the lumen of the appendix by stool, infective agents or lymphoid hyperplasia. Acute appendicits is the most common abdominal surgical emergency in the world, with a lifetime risk of 6.9% in females and 8.6% in males. If left untreated, the appendix can perforate resulting in sepsis and even death.1,2,3,4
Uncomplicated appendicitis is a condition where the appendix is inflamed, in the absence of gangrene, perforation or abscess.
Complicated appendicitis is a condtion where the appendix is inflamed in the presence of perforation, gangrene or periappendicular abscess.
Appendectomy (appendicectomy) is a surgical removal of the appendix. It can be done open or laparoscopic.
Appendicolith is a calcified mass formed by faeces and inorganic salts. It is associated with more severe appendicitis and higher risk of complication, making it an indication for surgical treatment.
When the appendix is posterior to another structure (eg. caecum – in retrocaecal appendix) it may not be visualised on imaging (especially on ultrasound), making it difficult to definitively make a diagnosis of appendicitis.
Retrocecal appendix: Less peritonism, pain more in the flank.
Arterial supply
Venous drainage
Nervous supply
Luminal obstruction (primary cause)
Other emerging mechanisms
Luminal obstruction ➔ Inflammation➔ Enlargement ➔ Obstruction of vessels ➔ Hypoxia ➔ Mucosal ulceration➔ Bacterial invasion ➔ Perforation and sepsis
Appendicitis pain
In early appendicitis, pain is periumbilical because the appendix receives afferent innervation from T10, which innervates the dermatome around the umbilicus. As inflammation progresses, it irritates the parietal peritoneum in the RIF. This causes the pain to migrate to the RIF, since the parietal peritoneum has somatic innervation that is well localised.
Triad Periumbilical pain → migration to right iliac fossa (RIF) + anorexia + nausea/vomiting
Alvarado score – for risk stratification
Alvarado score (TRAMLINE)
Laboratory findings
Imaging
IF imaging is inconclusive: monitor WCC and CRP for 48 hours after admission, without giving antibiotics – if levels come down chances of appendicitis are low.3
For female patients, rule out ectopic pregnancy and ectopic rupture.
Differential diagnosis
Mesenteric adenitis is a common presentation in children that can be difficult to differentiate from appendicitis due to similar findings on imaging – enlarged lymph nodes and free fluid (signs of inflammation).
Uncomplicated appendicitis
Complicated appendicitis
Acute appendicitis is essentially a clinical diagnosis; if there is high degree of suspicion, an appendicectomy can be performed without imaging.
Appendiceal carcinoid
Mainly found incidentally in appendix post appendicectomy. Comprises 85% of all appendiceal tumours. If <1cm in diameter it is considered cured by appendicectomy. If >2cm in diameter (rare), investigate for spread to sentinel lymph nodes. Managed by hemicolectomy.
Complications
Prognosis
In the elderly they have less classic features, higher risk of perforation.
1. BMJ Best Practice. Acute appendicitis 2025 [Available from: https://bestpractice-bmj-com.ezproxy.newcastle.edu.au/topics/en-gb/290.]
2. Petroianu A, Barroso TVV. Pathophysiology of Acute Appendicitis 2016 [Available from: https://www.jscimedcentral.com/public/assets/articles/article-pdf-1635934050-7440.pdf.]
3. Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World Journal of Emergency Surgery. 2020;15(1):27.
4. Körner H, Söndenaa K, Söreide JA, Andersen E, Nysted A, Lende TH, et al. Incidence of acute nonperforated and perforated appendicitis: age-specific and sex-specific analysis. World J Surg. 1997;21(3):313-7. https://doi.org/10.1007/s002689900235
5. New England Journal of Medicine. Antibiotics versus Appendectomy for Acute Appendicitis — Longer-Term Outcomes. 2021;385(25):2395-7. https://www.nejm.org/doi/full/10.1056/NEJMc2116018?query=recirc_Semantic#ap2
6. Ansari P. Appendicitis 2024 [Available from: https://www.msdmanuals.com/professional/gastrointestinal-disorders/acute-abdomen-and-surgical-gastroenterology/appendicitis.]

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion