Notes »
disease
» Obstetrics
Gestational Diabetes
Overview
| Definition Diabetes: A group of metabolic diseases in which there are high blood sugar levels over a prolonged period. Two types Diabetes Mellitus Type I (autoimmune destruction of beta cells in the pancreas) and Type II (insulin resistance followed by beta cell atrohpy) Gestational Diabetes: diabetes diagnosed during the second half of pregnancy with no prior existing diabetes. |
Affects 5-10% of pregnancies. Incidence varies between nutritional and genetic factors. Risk of GDM increases with age. Women born in Southern Asia are at particularly higher risk. 50% change of mother to develop Type II Diabetes later in life.
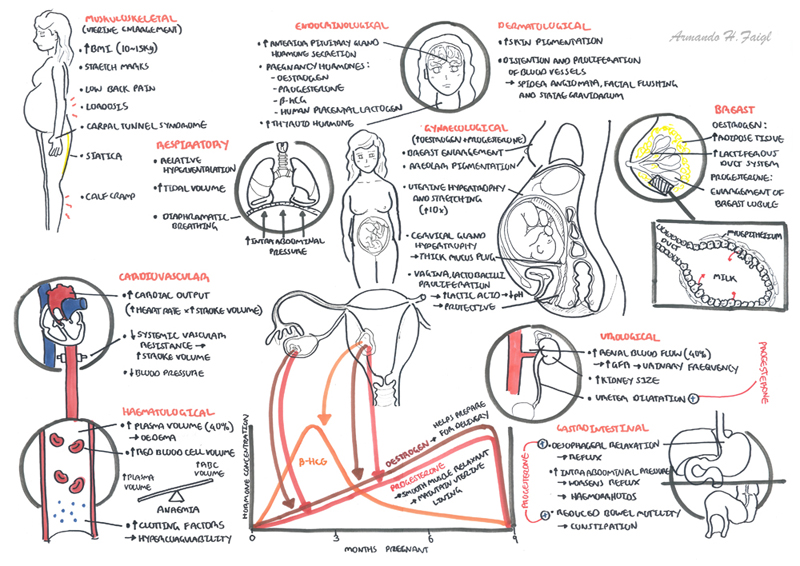
Pregnancy Physiology
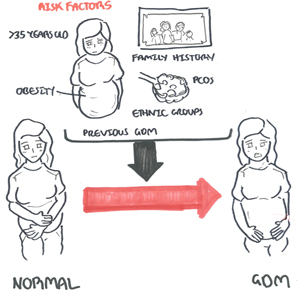
Risk Factors
- Previous GDM
- Increase BMI
- Maternal age >40yo
- Family history
- Polycystic ovarian syndrome
Low fibre diet - Weight gain as young adult
- Current use of glucocorticoids and antipsychotics?
Signs and Symptoms
Clinical Presentation generally asymptomatic
Classic signs of Type II Diabetes (4P's)
- Polyphagia
- Polydipsia
- Parasaethsia
- Polyuria
Investigations
Screening/Diagnosis
In Australia oral glucose tolerance test (75g) at 24 and 28weeks.
- Test at 1 hour >10 or 2 hour >8.5
- Fasting glucose 5.1 hour
| Diagnosing diabetes mellitus in pregnancy: The 7/11 rule. Fasting plasma glucose >7mmol/L and random BGL >11 mmol/L with symptoms of diabetes mellitus |
| Remember it is important to test for gestational diabetes because it can cause congenital abnormalities, miscarriages, organomegaly, hydramnios, pre-eclampsia, maternal and infant birth trauma, perinatal mortality and neonatal metabolic and respiratory problems. |
Pathophysiology
Normal Physiology
- Maternal metabolism switches from carbohydrates to fat utilisation
- Subsequent pancreatic beta cell hyperplasia
- Increased insulin secretion
- Early increase in insulin sensitivity causes progressive insulin resistance.
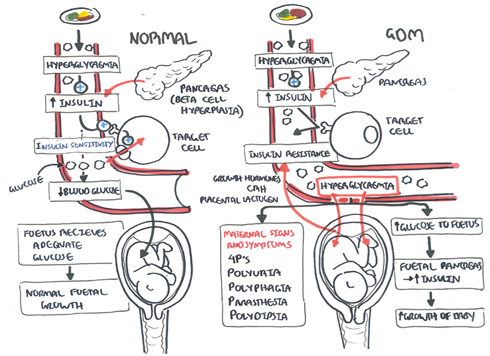
Pathophysiology
- Placenta produces growth hormone, CRH, placental lactinogen and progesterone.
- These hormones promote glucose intake by the fetus by causing insulin resistance in the mother
- Hyperglycaemia in circulation eventually cause the release of fetal insulin causing insulinaemia
Management
Diagnosis GDM then management of a multidisciplinary team (i.e endocrinologist, diabetic educator).
- Monthly ultrasound to check for foetal macrosomia.
- Diet, exercise and blood glucose monitoring.
- If glucose unstable change to insulin.
- Induction of labour if continuously unstable gestational diabetes before term or early at term - to prevent complications
- Postpartum (after delivery) stop insulin and glucose infusions, check blood glucose prior to discharge, follow up 6 weeks for oral glucose tolerance test, educate (as 50% risk of developing diabetes mellitus over the next 25years).
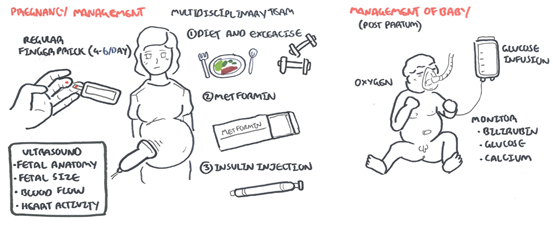
| Remember Why treat GDM? Reduction in composite outcome of death, shoulder dystocia, bone fracture and nerve palsy. Reduction in infants weighing >90th birth-centile. |
Complications and Prognosis
















