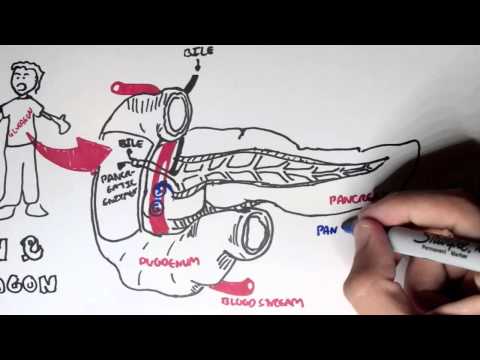
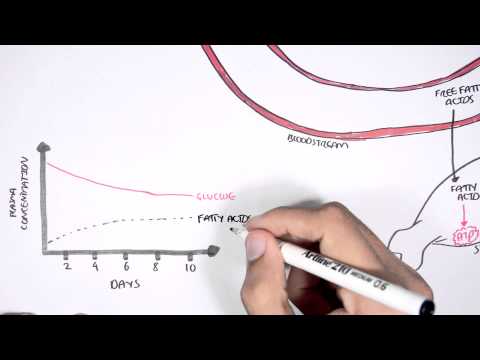
0:00 Hello, in this video, we're going to talk about diabetes pathophysiology. 0:09 This is an overview specifically focusing on diabetes type 2. 0:14 Diabetes type 2 is a problem where the hormone insulin, which is normally 0:19 secreted by the 0:20 pancreas, does not actually work properly. 0:24 The pancreas is an organ sitting behind the stomach, and secretes many things 0:29 for digestion, 0:30 but also it produces and secretes hormones, which are very important for 0:37 metabolism. 0:38 One of these hormones is insulin, which is produced in response to high blood 0:44 glucose. 0:45 An example is after we eat, glucose enters our blood, and then here it will 0:51 stimulate 0:52 the pancreas to produce insulin. 0:56 Before continuing on with the pathophysiology of diabetes, we actually need to 1:02 understand 1:03 what normally happens and how insulin works in a normal scenario. 1:09 So again, here is the circulation, here is the liver, and here is the pancreas. 1:15 The pancreas is the organ that produces insulin, and here is the adipose tissue 1:20 , fat, basically, 1:22 and here is the muscle cells, skeletal muscles. 1:26 And on these organs, on these cells of these organs, there are receptors for 1:31 insulin. 1:32 So again, high blood glucose will stimulate insulin production and insulin 1:37 release from 1:38 the pancreas. 1:40 The insulin will then target these different organs by binding onto insulin 1:45 receptors or 1:47 insulin sensitive proteins, with the sole purpose of decreasing blood glucose 1:55 levels. 1:56 The binding of insulin to its receptor or protein triggers a cascade of events 2:03 within 2:04 a cell, leading to the increased uptake of glucose from circulation into the 2:10 organs. 2:10 This is done, for example, by producing more glucose channels or transporters 2:16 on the 2:16 surface of cells, allowing glucose to move from the blood into the cells of the 2:25 organs. 2:26 Insulin also promotes glucose storage. 2:32 In the liver, insulin stimulates glycolysis and glycogenesis to store glucose 2:41 as glycogen. 2:43 But also stimulates glucose to be stored as fat, which will be subsequently 2:47 transported 2:48 to adipose tissue. 2:51 So going back to our first diagram, remember, high blood glucose stimulates 2:58 insulin release. 2:59 In type 2 diabetes, there is insulin resistance, which means that the receptor 3:05 's insulin works 3:07 on usually does not actually work properly or as effectively, and so insulin 3:15 essentially 3:16 does not work properly on liver adipose tissue and skeletal muscle. 3:24 And as a result, there will be high blood glucose levels for longer periods of 3:30 time. 3:31 Now insulin resistance occurs because of a number of variety of factors, 3:37 including genetics, 3:39 family predisposition, bad eating habits, and also obesity. 3:47 So because of insulin resistance, glucose cannot be taken up by all these 3:52 different organs, 3:55 and so you have high blood glucose. 3:59 Because there is high blood glucose, the pancreas is told to secrete more 4:06 insulin, despite 4:07 not changing the fact that insulin sensitivity is present. 4:13 With persistent high blood glucose, the glucose will travel to the kidneys and 4:18 be secreted 4:19 out. 4:20 This is called glucosuria. 4:24 Glucosuria will result in osmotic diuresis. 4:27 What does that mean? 4:29 The glucose will essentially drag water with it because it is a solute, and so 4:34 the person 4:35 will start peeing more polyurea. 4:40 With constant polyurea, you get loss of water and you get loss of electrolytes. 4:46 The loss of water and the loss of electrolyte leads to two main things. 4:52 One, dehydration because of the loss of water, and two, hyperosmolar state. 5:00 Hyperosmolar state is a medical emergency, which will not be really discussed 5:06 here. 5:06 The dehydration will stimulate the brain to drink more water, so we get polyd 5:14 ipsia. 5:15 Modern resistance can actually lead to polyfasia, which means the urge to eat 5:23 more, or the feeling 5:25 of hunger. 5:26 And how does this happen? 5:27 Well, if there is high blood glucose and it doesn't go into the tissues that 5:32 need it, 5:33 the organ will say, "Hey, I'm not receiving enough food, feed me," and so you 5:39 get polyfasia. 5:41 And dehydration in serious cases can lead to renal failure because of the 5:46 decrease of 5:46 blood flow going to the kidneys. 5:50 Remember that insulin has many functions in the liver, and because of insulin 5:55 resistance, 5:56 glucose is not stored properly. 5:59 Instead, you can get the opposite. 6:02 You can get the liver actually releasing more glucose in the attempt to supply 6:09 the organs 6:10 that need it. 6:13 It is important to know that with prolonged insulin resistance, eventually the 6:18 cells in 6:18 the pancreas that produces insulin, called the beta cells, these beta cells 6:24 will atrophy 6:25 because the body is not responding to the insulin properly. 6:30 And so this will further cause problems, and the person, the person who has 6:35 diabetes will 6:35 eventually need to be on insulin injections to compensate.