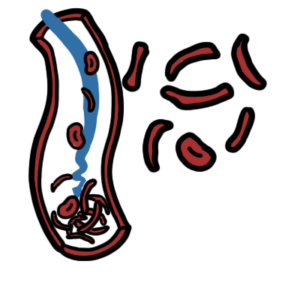
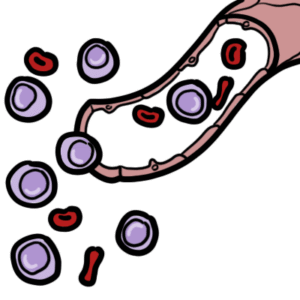
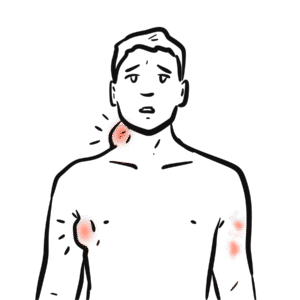
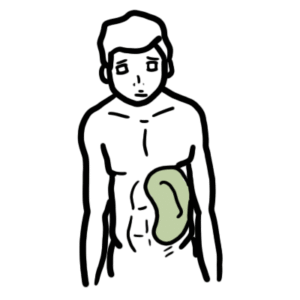
0:00 Hemolytic anemia is defined as anemia due to premature destruction of red blood 0:18 cells. 0:18 Red blood cells also known as erythrocytes are produced in the bone marrow and 0:22 then enter 0:23 circulation to become mature. 0:25 The mechanism of red blood cell hemolysis can be intravascular, which means 0:30 destruction 0:30 of red blood cells within the vasculature, or hemolysis can occur extravascular 0:35 , which 0:35 means hemolysis occurring outside the vasculature, typically in the organs such 0:40 as a spleen 0:41 and liver, where the reticular endothelial system resides. 0:48 Hemolysis stimulates the kidneys to produce erythropoate in a hormone which 0:53 stimulates 0:53 erythropoasis. 0:55 Red blood cells are produced from the myeloid progenitor cell line to become 1:02 reticulocytes 1:04 in the bone marrow. 1:07 As mentioned, erythropoatin, or EPO, stimulates erythropoasis, and the release 1:12 of EPO can 1:14 be due to decreased level of oxygen to tissues. 1:19 Poasis is also stimulated by other hormones, including androgens and thyroid 1:25 hormone. 1:26 Reticulocytes are the premature red blood cells, which are still able to 1:30 synthesize proteins. 1:32 After about three days, the reticulocytes will enter circulation while they 1:36 will mature 1:37 and become erythrocytes, which are a nucleated, so no nucleus cells. 1:44 The typical lifespan of a red blood cell is approximately 120 days, which is 1:50 four months. 1:51 During this time, the red blood cells circulate around the body through the sp 1:56 leen again and 1:57 again where they are subjected to remarkable amounts of mechanical stress. 2:02 Eventually, as they age and/or get injured, they normally get cleared up by the 2:07 body through 2:08 that reticular endothelial system I mentioned earlier. 2:11 I want to take a short time to introduce to you a cool program called PDFE 2:12 lements. 2:16 I'm sure a lot of you guys out there use PDFs for studying. 2:20 PDFElements is an all-in-one PDF editor from which you can get powerful 2:24 features to edit, 2:26 annotate, and convert PDF easily. 2:29 You just open a PDF file. 2:30 For example, here is a PDF file of the red blood cell life cycle. 2:34 If you want to add additional information, you simply get the text box and type 2:37 away, 2:37 change the font, size, and color as you like. 2:40 My PDF is important to remember here that erythrocytes come from the myload 2:44 progenitor line. 2:46 PDFElements also allows you to add images easily. 2:50 It even gives you the option to draw on the PDF file. 2:53 So here is an image of a blood film, and this here represents the erythrocytes 2:57 and 2:57 the bigger cell is the reticular site, the immature red blood cell. 3:02 PDFElements is a robust PDF editor, annotator, and converter on your windows 3:07 and Mac. 3:07 It greatly helps to read, take notes, and convert PDF easily. 3:11 Through this channel, you can save up to 50% off PDFElements by clicking on the 3:15 banner 3:15 in the video or on the description box below. 3:18 I really do recommend this program, especially if you like it in creative with 3:21 your notes. 3:21 Let's continue on with the rest of the video. 3:24 Humolytic anemia is due to premature destruction of the red blood cells and can 3:29 be easily grouped 3:30 into intravascular hemolysis, which is hemolysis occurring in the vasculature, 3:36 and extravascular 3:37 hemolysis, which is hemolysis occurring via the reticular endothelial system, 3:43 which is 3:43 also known as the mononucleophagocyte system situated in Oregon, such as the sp 3:48 leen and 3:48 the liver. 3:50 The reticular endothelial system houses many monocytes and macrophages. 3:55 These monocytes and macrophages normally clear up old and damaged red blood 4:02 cells. 4:02 However, in hemolytic anemia, the reticular endothelial system typically works 4:10 in overdrive 4:11 because they are destroying more red blood cells. 4:16 Because there is so much red blood cell destruction, you can find some 4:21 classical laboratory blood 4:22 changes in hemolytic anemia. 4:26 As a result of many premature red blood cell destruction, you get increase in 4:31 lactate dehydrogenase 4:32 and enzyme found in red blood cells. 4:36 One red blood cell contains millions of hemoglobin molecules. 4:41 When there is a lot of hemoglobin being broken down, such as in hemolytic an 4:46 emia, you get 4:47 a lot of globin, which will get recycled. 4:50 You have a lot of heme, which when further broken down, means you have more 4:56 iron and 4:57 unconjugated bilirubin. 5:00 With hemolytic anemia, you classically get hemoglobin molecules floating around 5:05 , which 5:06 have not been fully cleared up by the body. 5:09 Luckily, there are these molecules called haptoglobins, which pick up these 5:15 free hemoglobin 5:16 molecules, and then we'll actually carry them to the reticular endothelial 5:21 system to properly 5:22 remove these hemoglobin molecules. 5:25 So as a result, when you measure haptoglobin levels, they will be reduced in 5:30 hemolytic 5:31 anemia. 5:32 Again, this is because haptoglobin binds onto free hemoglobin and gets cleared 5:38 up. 5:38 In summary, the classic laboratory findings in hemolytic anemia is increased 5:42 lactate 5:43 dehydrogenase, increased bilirubin, and decreased haptoglobin. 5:48 With an increase in the reticulocyte count, because remember, hemolysis 5:52 stimulates erythropoiesis 5:53 and therefore reticulocyte formation production. 5:58 Now let us talk about the different causes of intravascular hemolysis and ext 6:03 ravascular 6:04 hemolysis, beginning with intravascular hemolysis. 6:09 A often forgotten cause of hemolysis is mechanical valve hemolysis, which is 6:13 red blood cell destruction 6:15 due to shear stress trauma to the red blood cell from a mechanical valve in the 6:25 heart. 6:27 During certain conditions when there is a procoagulative state or pro-thromb 6:31 otic state 6:32 such as in micro angiopathic hemolysis, red blood cells can get destroyed 6:38 because as they 6:39 pass through this clot, their cell membranes can get damaged and then they 6:45 burst and die. 6:46 Examples of micro angiopathic hemolysis include thrombotic thrombocytopenic per 6:52 perum, hemolytic 6:54 uremic syndrome, and disseminated intravascular coagulation. 6:59 Remember to note that when you look at the urine in these patients who have 7:03 micro angiopathic 7:04 hemolysis, you can find fragmented red blood cells. 7:10 There are also immune-mediated intravascular hemolysis, such as paroxysmal cold 7:15 hemoglobin 7:16 urea or paroxysmal nocturnal hemoglobin urea, both of which result in red blood 7:22 cell destruction 7:23 through complement activation. 7:29 Cold immune hemolytic anemia is another immune-mediated intravascular hemolysis 7:35 and this is where antibodies 7:37 recognize antigens on red blood cells at temperatures below normal core body 7:43 temperatures 7:44 and they actually induce the red blood cell destruction. 7:48 Cold immune hemolytic anemia are typically extravascular hemolysis due to the 7:53 immunoglobulin 7:55 M, but there are variants that cause intravascular hemolysis. 8:00 Another example of intravascular hemolysis can be seen when giving IV fluids. 8:05 This is osmotic lysis following infusion of hypotonic solutions. 8:10 When giving someone a hypotonic solution, this means water will tend to move 8:16 somewhere 8:16 with more solutes, which is the red blood cells in this case. 8:21 This causes the red blood cells to take in water, they will swell up and burst 8:25 leading 8:25 to intravascular hemolysis. 8:29 Another important cause of hemolysis is acute transfusion reactions. 8:33 Each person has a particular type of red blood cell characterized by an antigen 8:37 on their 8:38 surface. 8:39 This means that we can either be type A, type B, type AB, and type O. 8:45 If a type B recipient, which typically have type A antibodies, receive blood 8:50 from a type 8:51 A donor, the antibodies from the recipient will of course attack the red blood 8:57 cells, 8:58 causing hemolysis because the donor and recipient's blood are not compatible. 9:07 Important to remember that in intravascular hemolysis you see hemocidarin urine 9:11 , whereas 9:12 in extravascular hemolysis you do not see hemocidarin urine. 9:17 Hemocidarin urine is really brown urine, typically because of iron from the he 9:22 me. 9:23 It is usually seen three to four days after the onset of hemolytic conditions. 9:31 Now for causes of extravascular hemolysis, which can be further divided into 9:38 extracurricular 9:39 causes, and this is due to problems not within the red blood cell itself, or 9:45 problems inside 9:47 the red blood cells, such as the enzymes, the morphology, this is intracur 9:52 ricular. 9:53 And intracurricular hemolysis is usually congenital. 9:58 Regardless if it is intracurricular or extracurricular problems, the red blood 10:04 cell is abnormal 10:05 and will be cleared from the circulation via the reticul endothelial system, 10:10 where all 10:11 the monocytes and the macrophages are waiting. 10:14 This is what defines extravascular hemolysis. 10:19 Examples of extracurricular causes include warm autoimmune hemolytic anemia. 10:24 This is where antibodies attack red blood cell membranes when there is an 10:29 increase in 10:30 body temperature. 10:31 The antibody binds onto the cell membrane of red blood cells, bringing them to 10:35 phagocytes 10:36 promoting its clearance. 10:41 Hypersplenism is another cause of hemolytic anemia. 10:45 This is usually due to sequestration of the cells in the area, and an increase 10:50 in the 10:50 activity of the monocytes and macrophages as well. 10:55 Infections of red blood cells, such as malaria and bartonellosis, are important 11:01 causes of 11:02 extravascular hemolysis. 11:04 These parasites invade red blood cells, and because they are now abnormal cells 11:09 , they 11:10 are typically cleared from the body via the reticular endothelial system. 11:17 Intracurricular causes of hemolysis include hemoglobinopathies, problems in the 11:22 hemoglobin 11:23 molecule, its structure basically. 11:26 Remember, each red blood cell contains millions of hemoglobin molecules. 11:31 The structure of the hemoglobin is important for it to function properly in 11:35 order for it 11:36 to carry oxygen around the body. 11:38 Hemoglobinopathies are problems with the hemoglobin, such as encyclic cell an 11:43 emia and thalassemia. 11:45 As a result, these red blood cells are destroyed much quicker. 11:49 Hell membrane defects, such as hereditary spherocytosis, hereditary elliptocyt 11:56 osis, and hereditary 11:57 stomatocytosis, are also destroyed by the reticular endothelial system, because 12:03 the cell 12:04 membrane, the structure, the morphology of the red blood cells are abnormal, 12:08 and they 12:08 are unable to pass through the reticular endothelium successfully during its 12:14 daily circulation. 12:15 Finally, enzyme deficiencies, such as in G6P deficiency, is a cause of intrac 12:21 orposcular 12:22 hemolytic anemia. 12:24 Why is this? 12:25 Well, in red blood cells, anaerobic glycolysis is the main pathway to produce 12:31 energy in the 12:31 form of ATP. 12:34 During its process, free radicals are made. 12:37 G6P is an important enzyme which helps contribute to reducing free radical 12:43 formation, keeping 12:45 the cell healthy. 12:46 Without G6P, you have free radicals building up, causing damage to the cells, 12:52 and so these 12:52 cells will be cleared up by the reticular endothelial system a lot faster. 12:58 In summary, hemolytic anemia can be divided into intravascular causes and ext 13:03 ravascular 13:04 hemolysis. 13:07 Also, hemolysis can be further divided into extracorposcular.