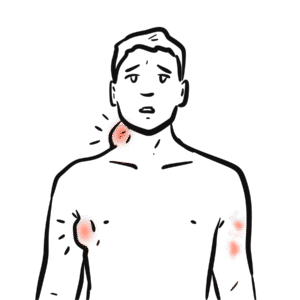
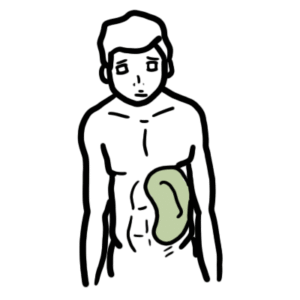
0:00 In this video we will talk about multiple myeloma, the signs, the symptoms, 0:09 pathogenesis, diagnosis, 0:10 and treatment of multiple myeloma. 0:14 Multiple myeloma is a malignant disease of plasma cells in the bone marrow. 0:19 It is the second most common hematological cancer, generally affecting older 0:24 people. 0:25 There is no known genetic component, hereditary genetic component, or 0:31 definitive environmental 0:32 risk factors. 0:34 Let us see what some common signs and symptoms of multiple myeloma are. 0:40 So many patients present with back pain, infections of the respiratory tract, 0:46 anemia, which will 0:47 result in tightness and fatigue, renal failure, and protein urea. 0:55 People, patients with multiple myeloma, also suffer from fractures and 1:03 dehydration. 1:05 And finally investigations, including scans, will show litic bone lesions. 1:11 Looking at vertebrae and bone marrow, we find that bone will suffer from litic 1:21 bone lesions. 1:24 The vertebrae is also a site for hematopoiesis, the production of cells for the 1:31 blood, which 1:32 arises from hemopoietic stem cells. 1:36 So if we were to zoom into the bone marrow, here we have a hemopoietic stem 1:41 cell within 1:41 the bone marrow. 1:43 Normally the hemotopoietic stem cell will eventually make B cells and then 1:49 plasma cells, 1:50 which will event where the plasma cells will eventually reside in the bone 1:57 marrow. 1:58 Normally the bone marrow contains less than 5% plasma cells, which are the long 2:03 -lived plasma 2:04 cells and they, and these guys, they secrete antibodies, remember, plasma cells 2:09 secrete 2:09 antibodies to help fight against infection. 2:13 The antibodies, secreated, are normal, consisting of a light and heavy chains. 2:20 Now in multiple myeloma, the hemopoietic stem cell shifts production mainly to 2:25 produce 2:26 more B cells and then finally plasma cells. 2:29 Thus, in the bone marrow, we end up with more than 10% plasma cells occupying 2:36 the bone marrow. 2:37 And now these plasma cells, they secrete abnormal antibodies. 2:41 75% of multiple myeloma cases, the antibodies are abnormally produced in high 2:48 amounts. 2:50 And plasma cells also produce just light chains. 2:53 So they produce abnormal antibodies and they produce light chains only. 2:58 And these light chains only that are being produced are called the para 3:04 proteins. 3:05 The main antibodies produced, or that are found associated with multiple myel 3:10 oma, are 3:10 high amounts of IgG and IgA. 3:15 Let us now look at the pathophysiology and the interaction that occurs between 3:23 these 3:24 abnormally high amounts of plasma cells with other cells in the bone. 3:29 Firstly, we just need to recap some cells found in the bone and bone marrow. 3:35 So the bone contains a number of cells. 3:38 Osteoblasts are cells that build bone, osteoclasts are the cells that break 3:43 down bone. 3:44 And then we have things called bone marrow stromal cells which regulate a hemat 3:53 opoiesis. 3:54 So looking at this diagrammatically, here we have osteoblast and osteoblast, 4:00 which 4:01 will secrete osteoids. 4:03 And which together with minerals, calcium and phosphate, they will form strong 4:11 bones. 4:12 Osteoclasts on the other hand break down bone by secreting hydrochloric acid. 4:17 The breakdown of bone results in the release of calcium and the phosphate. 4:23 And the calcium here will enter the plasma, the blood. 4:27 The interesting thing is that osteoclasts activation, so the bone breaking 4:33 cells, the 4:33 bone breaking cells activation is regulated by osteoblasts, which express Rank 4:40 L. When 4:40 Rank L binds to Rank on osteoclasts, this will stimulate osteoclastic activity. 4:49 But osteoblasts also secrete another molecule called OPG, which inhibit this 4:54 interaction, 4:55 thus inhibits or decreases osteoclastic activity. 5:01 Now let me introduce the bone marrow cells and the pathophysiology of multiple 5:06 myeloma. 5:07 The bone marrow stromal cells normally regulate a hematopoiesis, right? 5:12 But in multiple myeloma, these bone marrow stromal cells will interact with 5:17 these cancer 5:18 cells through receptors and cytokines. 5:21 Adhesion of multiple myeloma cells to the bone marrow stromal cells results in 5:28 cytokine-mediated 5:29 cell growth, survival, drug resistance, and migration. 5:38 So essentially, the bone marrow stromal cells helps the multiple myeloma cells 5:42 survive and 5:43 grow. 5:44 So let's look, so when the multiple myeloma cells survive and grow, they then 5:49 do other 5:49 things that help, that help themselves. 5:53 So the multiple myeloma cells secrete many cytokines and they have some bad 5:59 consequences 6:00 for the body. 6:02 So for example, the multiple myeloma cells can secrete interleukin-3, which 6:06 actually 6:06 decreases osteoblastic activity by inhibiting osteoblasts, progenitor cells to 6:12 become osteoblasts. 6:14 So basically it just decreases the production of osteoblasts. 6:20 The multiple myeloma cells also secrete DKK1, which inhibit OPG production by 6:26 osteoblasts, 6:28 thus resulting in an increase in osteoclastic activity. 6:33 Multiple myeloma cells also stimulate osteoclastic activity through MIP1 alpha 6:39 and through expression 6:40 of rank ligand. 6:44 The osteoclasts can self-stimulate itself and the multiple myeloma and bone 6:51 marrow stromal 6:52 cells through interleukin-6. 6:54 So this whole picture shows an amplification of multiple myeloma cells, osteocl 7:02 astic activity 7:04 and a decrease in osteoblastic activity. 7:08 So osteoclastic activity is basically promoted and osteoblastic activity is 7:16 reduced. 7:17 When osteoclastic activity is stimulated, this will result in bone marrow 7:22 breaking down. 7:24 An increase in osteoclastic activity will lead to fractures and littic lesions. 7:30 And also will result in more calcium entering the body. 7:34 So in the blood again here we have hypercalcemia, which can cause nerve 7:40 problems and dehydration. 7:42 In the blood there is also paraproteinemia with bits of light chains floating 7:48 around. 7:49 The paraproteinemia has some bad effects and remember the light proteins, these 7:53 paraproteins 7:54 are being produced by the multiple myeloma cells. 7:57 So these light chains, these paraproteins are small enough to get filtered 8:01 through the glomerulus 8:02 of the kidneys and it can lead to renal failure in 20% to 30% of cases. 8:11 The light chains are also urinated out, they're peed out, which is a clinical 8:15 feature of multiple 8:16 myeloma. 8:17 When light chains are urinated, it is known as Ben's Jones proteins. 8:24 Multiple myeloma as I mentioned at the start also leads to anemia and this is 8:27 through several 8:28 mechanisms. 8:29 Three, the first is that there is a shift of hematopoietic stem cells from myel 8:35 oid progenitor 8:36 to lymphoid progenitor to make more plasma cells. 8:40 Two, overproduction of plasma cells clog up the bone marrow, stopping red blood 8:46 cells 8:47 being formed and entering the plasma. 8:49 Three, there is also the kidney failure, failing kidney, which results in 8:55 decreased erythropoiesis, 8:57 ethropoietin production, and so decrease in red blood cell production. 9:03 There are many investigations that can be performed in multiple myeloma to sort 9:07 of rule out other 9:08 problems and to confirm that it's multiple myeloma. 9:12 And these investigations include blood and urine tests. 9:15 In the blood tests, we can detect anemia as a result of abnormal red blood cell 9:21 level. 9:22 We can see an increase in paraproteins, a decrease in normal antibodies. 9:28 We see hypercalcemia as a result of increased breakdown of bone. 9:33 We see increase in urea and nitrogenous basis as a result of renal failure as 9:39 well as an 9:40 increase in creatinine, which is a measure of renal competency, I guess. 9:49 Parent tests show urinary Benz-Jones proteins, which are the light chains that 9:53 are peed out, 9:55 remember. 9:56 And then bone investigations include bone aspiration, bone marrow biopsy, which 10:00 can show more than 10:01 10% plasma proteins in the bone marrow. 10:06 X-rays can show osteoporosis, and CT scans can show lesions of the bone and 10:16 soft tissue. 10:18 So those are the investigations we can perform in multiple myeloma. 10:22 The actual diagnosis of multiple myeloma is one, the presence of monoclonal 10:29 plasma cells 10:30 in the bone marrow, 10% or greater. 10:33 So this is through bone biopsy. 10:37 Two, the presence of monoclonal antibodies, or the paraproteins in serum, or in 10:46 urine. 10:47 And three, one or more of the following. 10:51 So I have an acronym hral, or some people use crab, same thing. 10:57 So I use hral, H is for hypercalcemia, R is for renal failure, A is for anemia, 11:04 and L is 11:05 for lytic bone lesions. 11:07 So that's how you diagnose it. 11:09 And to treat multiple myeloma, chemotherapy and radiotherapy of the vertebrae, 11:15 vertebral 11:16 bodies, or whichever, wherever the plasma cells are located, the neuroplastic 11:25 plasma cells 11:26 are located. 11:27 So chemotherapy and radiotherapy. 11:31 And I won't go into more detail than that. 11:34 Hope you enjoyed this video on multiple myeloma. 11:36 Thanks for watching. 11:37 Bye.