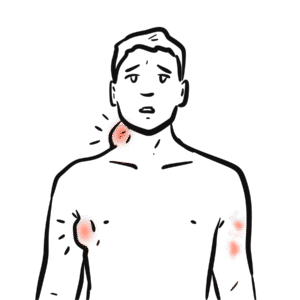
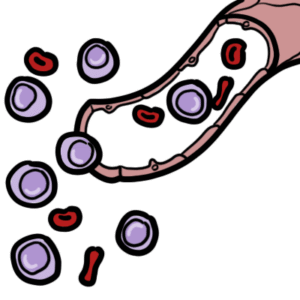
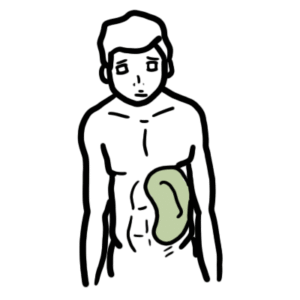
0:00 Hello, in this video we're going to look at the B cell and the T cell story, so 0:12 the story 0:12 of the B and T cells, as well as we will introduce lymphoma, particularly the B 0:18 cell lymphoma. 0:20 So I'll just introducing the organs here that are associated with the B and T 0:26 cells. 0:27 We have the bone marrow, the thymus, and the lymph node. 0:34 Now in the bone marrow there are lymphoid progenitor cells which can either 0:39 become a precursor 0:41 T cell or a precursor B cell. 0:45 Let us follow the precursor T cells. 0:48 The precursor T cells will move into the thymus where they become thymocytes, 0:54 double negative. 0:57 They are double negative because they are negative for both CD4 and CD8 1:04 receptors. 1:05 In the thymus, however, the double negative thymocytes will develop to become 1:10 either 1:10 a CD8 naive T cell which will have the CD8 receptor or a CD4 naive T cell with 1:19 a CD4 1:20 receptor. 1:22 The naive CD4 and CD8 T cells will also have a T cell receptor on them. 1:29 And the naive CD4 naive T cells will then move into the lymph node ready to 1:34 become activated. 1:37 Now let us look to the bone marrow and follow the precursor B cell. 1:42 With the help of the enzyme RAG1 and 2, the precursor B cell in the bone marrow 1:48 will 1:49 undergo VDJ recombination of light and heavy chains to form a naive B cell with 1:56 a membrane 1:57 bound IgM antibody. 2:00 So the naive B cell actually will have a unique, you can say, a specific type 2:07 of antibody 2:08 on its surface for a specific type of antigen. 2:13 So the naive B cell will leave the bone marrow and proceed to the lymph node. 2:19 During circulation or within the lymph node, the naive B cell, if the naive B 2:26 cells IgM 2:27 surface-bound IgM recognizes an antigen, it will phagocytize it and then 2:33 present the 2:34 antigen on an MHC class II molecule on its cell surface. 2:40 Now the experienced naive B cell now waits for either co-stimulation or 2:47 stimulation by 2:48 a activated CD4 T cell. 2:54 So we're going to look at what happens in co-stimulation. 2:58 So let us just say this naive CD4 T cell can recognize the antigen being 3:03 presented by the 3:04 B cell. 3:06 What happens next is called co-stimulation. 3:10 The naive CD4 T cell stimulates the naive B cell and the naive B cell 3:14 stimulates the 3:15 CD4 T cell. 3:19 Alternatively, alternatively, what could have happened is that a fully 3:24 activated CD4 T cell 3:26 could have activated the naive B cell. 3:29 But anyways, what we end up with is an activated CD4 T cell and an activated B 3:36 cell. 3:37 When the B cell is activated by the T cell, something big happens. 3:42 There are cytokines that the T cell will secrete, that trigger the naive B cell 3:47 to proliferate 3:48 into central blasts. 3:52 During the proliferation process, each individual B cell undergoes what is 3:57 known as somatic hypermutation 4:00 by the AID enzyme. 4:05 Scic hypermutation introduces point mutation in the variable region of the 4:12 antibody gene. 4:13 Thus what we end up with are we end up with many central blasts, each with 4:20 different surface 4:23 IgM antibodies, because their variable regions have slightly changed thanks to 4:31 the mutations. 4:33 So these central blasts can have antibodies with either an increased or 4:37 decreased affinity 4:39 to that antigen. 4:45 The central blasts then move through the germinal center to where there are 4:49 many follicular 4:50 dendritic cells presenting many antigens on its surface. 4:54 There are also follicular T helper cells in this area. 5:03 When the central blasts move from one part of the germinal center to the other, 5:09 they 5:09 become centrocytes. 5:12 And these centrocytes need cytokines in order to survive and mature. 5:18 So they sample these antigens presented by the gendritic cells using their 5:23 newly acquired 5:24 specific surface IgM antibody. 5:29 Unfortunately some centrocytes will have decreased affinity to these antigens 5:34 after undergoing 5:36 somatic hypermutation. 5:38 The ones that have decreased affinity will die through apoptosis. 5:43 Fortunately however, there are centrocytes that will have an increased affinity 5:47 following 5:48 hypermutation. 5:49 And so will easily recognize the antigen presented by the follicular dendritic 5:55 cell. 5:55 So if these centrocytes recognize the antigen, it will again engulf it and 5:59 present it to the 6:00 T helper follicular cell nearby. 6:04 The T helper follicular cell will now help the B cell, help the centrocyte 6:09 which is the 6:10 B cell, help the centrocyte to proliferate and then to differentiate. 6:15 The centrocyte can differentiate into memory B cell or into a plasma blast 6:21 which will then 6:22 become a plasma cell. 6:26 Plasma cell are the type of B cells that secrete antibodies. 6:31 When the centrocyte receives signals from the T cells to differentiate, the 6:37 centrocytes 6:38 actually undergo class switching. 6:40 Which is basically where the constant region of the antibody can become a 6:49 specific class. 6:51 So it can change into an IgE, IgA or IgG for example. 7:01 Now I hope that made sense. 7:05 I also, we also have to introduce the thymic B cells which are B cells that 7:09 reside in the 7:10 thymus but we will not go into the functions of the thymic B cells here. 7:15 Ok so what you have watched till now was an overview, overall picture sorry of 7:19 the T cell 7:21 and particularly the B cell story. 7:25 Now we will start looking at lymphoma which as the name suggests is tumor of 7:30 the lymph. 7:31 Alpha involves cancer cells coming from mainly T or B cell development. 7:37 So using this diagram we can see in which steps of the T and B cell development 7:42 these 7:42 cancers these cancer cells may arise from and what type of lymphoma can result. 7:49 So lymphoma, lymphoma is a heterogeneous group of malignancies characterized by 7:55 proliferation 7:56 of lymphoid tissue, diverse and they are diverse in cellular origin, morphology 8:02 , immunofinotype, 8:04 cytogenetic and molecular abnormalities and they are different in response to 8:10 treatment 8:11 and prognosis. 8:14 So they are big deal. 8:15 Lymphoma can be categorized into two broad categories. 8:18 These are Hodgkin's and non-Hodgkin's lymphoma. 8:22 In this video we will focus on non-Hodgkin's lymphoma which is the sixth most 8:27 frequent 8:27 cancer and it is increased and it is increasing in prevalence. 8:33 Risk factors for non-Hodgkin lymphoma include immunological disturbances, viral 8:39 , genetic 8:39 and environmental. 8:42 So immunological can be HIV or autoimmune diseases which predisposes one to 8:47 lymphoma. 8:49 Scientists such as HIV, epsilon bar virus and HCV are risk factors also for 8:55 lymphoma. 8:56 Genetics as in climb filters and SCID increases the risk of non-Hodgkin lymph 9:02 oma and environmental 9:04 risk factors include pesticides, herbicides and smoking. 9:10 Okay now let us look at the different types of non-Hodgkin's lymphoma and where 9:14 they can 9:15 arise from. 9:16 So non-Hodgkin's lymphoma can either be B cell or T cell in origin. 9:25 We will first look at the T cell non-Hodgkin's lymphoma. 9:29 So T cells in the thymus during its development can give rise to precursor T 9:34 cell lymphomas 9:35 which we won't go into. 9:38 Similarly T cells that have moved into the lymph node can give rise to what's 9:41 called 9:41 the peripheral T cell lymphomas, the neoplasmum. 9:47 Now T cell lymphomas can arise during genetic rearrangement of the T cell 9:51 receptor and during 9:53 positive and negative selection in the thymus which will lead to either 9:58 precursor or peripheral 9:59 T cell lymphomas. 10:01 Of course that's like that was just super basic overview. 10:06 Now what is important to know is that T cell lymphomas are less common than B 10:11 cell lymphomas. 10:13 So we just looked at two types, two classes you can say of T cell lymphomas. 10:20 Now let us focus on B cell lymphomas and we'll go into more detail. 10:25 We will focus more on the B cell lymphomas because as I mentioned just then the 10:29 prevalence 10:30 of the B cell lymphoma is much higher than the T cell and this is because B 10:36 cells undergo 10:37 so many genetic changes during its development. 10:42 Many B cells can give rise to mantle cell lymphoma. 10:47 B cells that have experienced an antigen encountered can become a chronic lymph 10:52 ocytic leukemia 10:53 or small lymphocytic lymphoma. 10:59 Lymphoma and leukemia can often be confusing, they are different yet related. 11:04 The main difference is that leukemia involves the blood. 11:08 Anyways, we won't really talk about leukemia and lymphoma in this video but it 11:12 's just good 11:13 to know that this particular part of the B cell development can lead to the 11:20 chronic lymphocytic 11:21 leukemia or the small lymphocytic lymphoma. 11:25 The central blasts in the germanol center can give rise to bercus lymphoma and 11:30 germanol 11:31 center be like diffuse large B cell lymphoma or dlbcl which has interestingly 11:41 60% five 11:43 years survival. 11:45 Both bercus lymphoma and germ cell be like diffuse large B cell lymphoma are 11:53 some of the 11:54 common types of B cell lymphomas because possibly because of the genetic 11:59 mutation that occurs 12:01 following somatic hyper mutation in the germanol center. 12:08 What I mean is that following hyper mutation in the germanol center which is a 12:12 normal process 12:14 it can lead to mutations leading to cancer which is the bercus lymphoma or the 12:21 large 12:22 diffuse B cell lymphoma. 12:26 The central sites can give rise to follicular lymphoma. 12:30 Memory B cells following class switching which is another genetic rearrangement 12:34 can give rise 12:34 to chronic lymphocytic leukemia or the small lymphocytic lymphoma as we've 12:40 already introduced 12:42 earlier. 12:45 Plasma blasts can give rise to activated B cell like diffuse large B cell lymph 12:50 oma which 12:51 has a 35% five year survival. 12:55 So now we've actually talked about two types of diffuse large B cell lymphoma. 13:01 Well we actually have three and the third one arises from the thymic B cells. 13:06 So here the thymic B cells can give rise to what is called the primary mediast 13:11 inal B cell 13:11 like diffuse large B cell lymphoma. 13:15 So we have one, two, three types of diffuse large B cell lymphoma. 13:22 Anyways the reason it is important to know this is because the most common non- 13:29 hudgkins 13:30 B cell lymphoma are the diffuse large B cell lymphomas as well as the foll 13:36 icular lymphomas. 13:38 So that is why it's important to know these. 13:42 So those were the major types of lymphomas I wanted to talk about. 13:45 But using this diagram it is also important to introduce a common type of 13:49 cancer which 13:49 arises from one particular cell which are the plasma cells. 13:55 Plasma cells can give rise to multiple myeloma in which there are so much 14:02 plasma cells being 14:03 produced and moving into the bone marrow that it causes big problems. 14:08 And I will have a video on that hopefully, a link to the video hopefully. 14:17 So so far we have talked about the B and T cell story and we have introduced 14:21 the different 14:22 types of lymphomas. 14:26 Now let us look at the reason why they arise. 14:30 So I guess the molecular aspect of lymphoma which is important. 14:38 So we just looked at the T and the B cell story as well as the different types 14:43 of non-hudgkins 14:45 lymphoma that can arise during different periods of the development of the B 14:52 and T cells. 14:53 Now let us look at the pathophysiology basically how do these lymphomas arise 15:00 and they basically 15:01 arise mainly through genetics, genetic changes such as one translocation and 15:08 two mutations 15:10 during development during like somatic hyper mutation for example or class 15:17 switching. 15:18 So the translocations of chromosomes are seen in many of the lymphomas. 15:26 And of for example the BCL2 and BCL6 genes are seen in a lot of lymphomas. 15:37 And also we can see mutations and amplifications of certain genes such as 15:43 mutations in the 15:45 P53 gene, the BCL2, the BCL6 and the MYC genes. 15:53 So we just overall know that lymphomas arise from genetic changes such as 15:58 translocations 15:59 and mutations during the development of the cells. 16:04 Thank you for watching. 16:05 I hope you enjoyed this video.