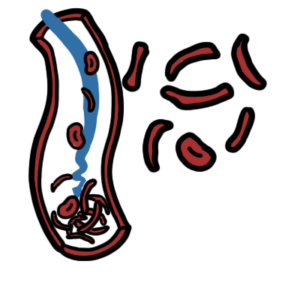
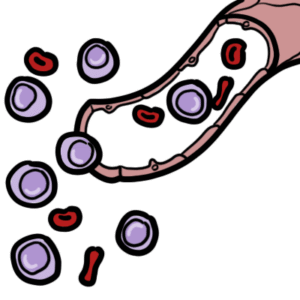
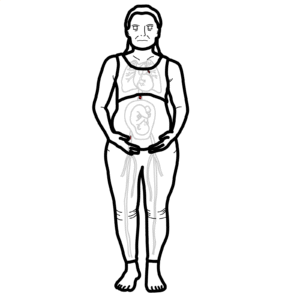
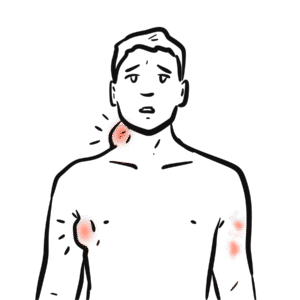
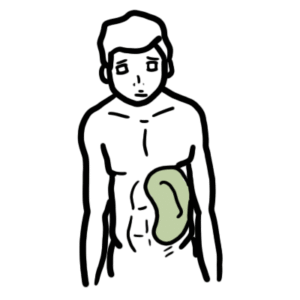
0:00 Hello, in this video, we're going to talk about primary myelofibrosis. 0:09 This is an overview and introduction. 0:12 Primary myelofibrosis is a type of myeloproliferative disorder. 0:19 Remember that there are three classic myeloproliferative disorders, and these 0:25 include polycythemia 0:27 rubrovera, essential thrombocythemia and primary myelofibrosis. 0:35 So with primary myelofibrosis in particular, it is characterized by clinical 0:41 proliferation 0:42 of myeloid cells with variable morphological maturity and hematopoietic 0:52 efficiency. 0:54 Let's look at the normal and compare it to primary myelofibrosis. 1:00 So normal, we have bones that contain bone marrow. 1:05 This bone marrow mostly are found in flat bones, in adults, and contain hematop 1:11 oietic stem cells. 1:14 These stem cells have the potential to become any blood cell type in our body. 1:20 For example, the hematopoietic stem cells can become white blood cells, red 1:25 blood cells 1:26 or mega carrier sites, which subsequently become platelets. 1:33 These three cells are very different in function and serve completely different 1:38 purposes in 1:39 our body. 1:40 The bone marrow and cell differentiation has to work properly in order to 1:46 produce these 1:47 red blood cells, white blood cells and mega carriers. 1:52 Some people can develop primary myelofibrosis due to some factors, but mainly 1:57 the exact 1:58 cause is unknown. 2:01 Primary myelofibrosis is myelofibrosis that is not secondary to another disease 2:08 . 2:08 Primary myelofibrosis is a myeloproliferative disorder on its own. 2:16 A lot of people with primary myelofibrosis are asymptomatic, about 30%, but the 2:22 majority 2:23 of these people who are asymptomatic have spleenomegalae in large spleen or he 2:31 patomegalae 2:32 in large liver. 2:35 And we will see why this happens as we go along in the video. 2:41 In myelofibrosis, what we see is fibrosis occurring in the bone marrow, the 2:47 area where 2:48 hematopoietic stem cells usually differentiates and become our blood cells. 2:55 Within the fibrotic bone marrow, there is an increase in fibroblasts, which 3:00 means that 3:01 there is an increase in collagen formation and deposition, and also a type 3 3:05 collagen 3:06 also known as reticulum. 3:09 The proliferation of fibroblasts and the deposition of collagen is actually a 3:16 result of hyperplasia 3:18 of mega-cariocytes in the area. 3:22 Remember that mega-cariocytes are the cells that produce and eventually release 3:29 platelets. 3:30 There is also proliferation of blood vessels, angiogenesis, and also osteos 3:36 clerosis, which 3:37 is because of the increase in activity of osteoblasts, the bone-building cells 3:43 in the 3:43 area. 3:46 What is not shown here is also the proliferation of neutrophils that also 3:50 contribute to the 3:50 fibrotic transformation of the bone marrow. 3:55 Keeping these bone marrow fibrotic changes in mind, let us focus now on the 4:00 pathophysiology 4:01 of myelofibrosis, and it is quite an amazing story. 4:05 So here is the same person who has primary myelofibrosis. 4:11 Here is his liver and spleen on the left, below the diaphragm. 4:16 In primary myelofibrosis, there is bone marrow fibrosis with cellular 4:21 abnormalities within 4:23 the bone marrow. 4:26 The etiology or cause of these changes is not exactly known, but however, there 4:34 are several 4:35 factors that have been identified. 4:38 For example, there are chromosomal abnormalities that are found up to 60 4:43 percent of cases. 4:45 A common example is a mutation of the retinoblastoma gene, for example. 4:52 Another common finding is a JAC2 mutation, with or without the STAT mutation. 4:58 Now the JAC2 STAT mutation is a signaling pathway within cells that essentially 5:06 allows the cells 5:07 to proliferate and to survive. 5:12 A common feature of primary myelofibrosis found in the bone marrow is mega-car 5:17 ioside 5:18 growth and abnormal hyperplasia of these cells. 5:22 And there are many causes of this. 5:25 Some ideas include thrombopoietin receptor mutation or overexpression of thromb 5:31 opoietin 5:31 itself. 5:33 Thrombopoietin is a hormone, a factor which stimulates mega-carioside 5:38 development and 5:39 therefore stimulates platelet production. 5:43 Platelets are also known as thrombocytes. 5:48 Finally these abnormal mega-cariosides and the other cells within the bone 5:53 marrow with 5:54 the JAC2 mutation can begin releasing cytokines abnormally. 6:00 And this is unnecessary. 6:03 These cytokines can include growth factors which recruit things such as fibrobl 6:09 asts and 6:10 stimulate fibroblasts to proliferate and thus cause deposition or formation of 6:17 collagen 6:18 turning the area into a fibrotic tissue causing the whole mox of primary myelof 6:23 ibrosis that 6:24 is bone marrow fibrosis. 6:28 Because the bone marrow becomes fibrotic and because of the abnormal cells in 6:32 the area, 6:33 the bone marrow is unable to keep up with the production of red blood cells, 6:37 white blood 6:38 cells and platelets. 6:40 As a result, the hematopoietic cells migrate to other organs. 6:45 The liver and the spleen take over the role of hematopoiesis. 6:49 When hematopoiesis occurs outside the bone marrow, this is called extra-mod 6:56 illary hematopoiesis. 6:58 As a result of hepatic hematopoiesis, you get hepatomegaly. 7:04 Similarly, as a result of splenic hematopoiesis, you get splenomegaly. 7:10 The liver and spleen are essentially compensating for the fibrotic bone marrow. 7:16 Again, as a consequence of myelofibrosis, hematopoietic stem cells may migrate 7:22 to the 7:23 liver and spleen. 7:25 A note about the spleen, the spleen can grow so big it extends to the left-cost 7:32 al margin 7:33 of the ribs and even further and extend towards the pelvic rim. 7:40 The spleen enlarges and it can actually compress the structures nearby, such as 7:46 the stomach, 7:47 which is right next to it. 7:49 Because the spleen compresses the stomach, it can cause early satiety. 7:57 Splenomegaly can undergo small infarctions and irritate the surrounding tissue, 8:02 causing 8:02 left upper quadrant pain. 8:07 Splenomegaly may also cause abdominal discomfort and a dragging sensation. 8:14 Splenomegaly can cause thrombocytopenia in later stages of the disease and also 8:19 sequestration 8:21 and destruction of red blood cells. 8:24 This is one of the contributors of anemia, seen in people with myelofibrosis. 8:32 But there are actually many other causes of anemia in myelofibrosis. 8:38 For example, the bone marrow fibrosis and cellular abnormality can lead to 8:43 reduction 8:44 in medullary erythropoasis, which can contribute to anemia. 8:49 Further, the extra medullary hematopoasis can be ineffective and not produce 8:56 enough 8:56 red blood cells, or what not, and this will subsequently contribute to anemia. 9:05 Going back to the bone marrow fibrosis, as mentioned, you get abnormal medull 9:10 ary hematopoasis, 9:12 which contributes to anemia. 9:15 But this abnormal medullary hematopoasis can also lead to leucocytosis or leuc 9:23 openia, 9:24 so increase in leucocytes or decrease in leucosites. 9:29 It can also cause thrombocytosis or thrombocytopenia, so a lot of platelets or 9:35 reduced number 9:36 of platelets. 9:38 Thrombocytopenia is more of a common feature in the late stage of the disease. 9:45 The abnormal medullary hematopoasis means that there will be more abnormal 9:50 cells being 9:51 produced. 9:52 And this means that more cells will be destroyed and so there will be an 9:58 increase in cell turnover. 10:00 This increase in cell turnover means that there will be an increase in things 10:04 such as 10:04 uric acid from DNA, which can lead to gout and urinary stone formation. 10:12 As well, the increase in cell turnover means an increase in lactate dehydrogen 10:18 ase. 10:19 Thus, these findings uric acid and lactate dehydrogenase are markers in myelof 10:28 ibrosis. 10:30 The ineffective extra medullary hematopoasis, together with this sequestration 10:35 of red blood 10:36 cells, white blood cells and platelets in the spleen, contribute to splenomegal 10:43 ae, but 10:43 also lead to lecopenia, thrombocytopenia and an increase in overall cell 10:52 turnover, leading 10:53 again to mention earlier an increase in metabolites such as lactate dehydrogen 11:01 ase and uric acid. 11:03 Bone marrow fibrosis and cellular abnormality can cause pain once it involves 11:09 the periosteum, 11:11 which contains pain-nerve fibres. 11:16 Let's go to the other side now and talk about the liver, hepatomegalae. 11:22 Remember, hepatomegalae is a common feature in myelofibrosis, a result of extra 11:27 medullary 11:28 hematopoasis. 11:30 With an enlarged liver, there can be portal hypertension. 11:35 Portal hypertension leads to a few things, it causes esophageal and gastric var 11:41 ices, 11:41 which can lead to gastric bleeding, and thus contribute to anemia when you lose 11:49 blood. 11:50 Portal hypertension can also lead to hepaticing and cathalopathy in later 11:57 stages. 11:57 Portal hypertension can also cause ascites, which can predispose one to 12:02 spontaneous bacterial 12:03 infection of the peritoneum. 12:07 When the bone marrow cannot perform hematopoasis properly, extra medullary 12:13 organs take over 12:15 the job, as mentioned. 12:17 Now, extra medullary hematopoasis is very interesting. 12:23 The spleen and the liver are usually responsible for the majority of extra med 12:29 ullary hematopoasis 12:30 when the bone marrow fails. 12:35 But the lymph nodes can also do this, leading to lymphadenopathy. 12:41 What's crazy is that the lungs and pleura can also perform hematopoasis, which 12:48 may lead 12:48 to pleural fusion and pulmonary hypertension. 12:53 Lots of the gastrointestinal tract and the genital urinary tract can also do 13:00 this. 13:01 What's mind-blowing is that the thalamus, the brain area, and other parts of 13:06 the brain 13:06 can also perform hematopoasis if it needs to. 13:14 Knowing the pathophysiology of primary myelofibrosis, the clinical presentation 13:21 therefore can include 13:22 fatigue, which is seen in a majority of cases, 60%, and this is due to anemia. 13:30 The signs and symptoms can also include spleenomegaly, seen in up to 50% of 13:36 patients. 13:37 Hepatomegaly, pruritis, pulmonary hypertension, it's also important to note 13:45 that hypermetabolic 13:46 state or constitutional signs can also be seen, including fever, bone pain, 13:53 night sweats, 13:55 and weight loss. 13:59 The risk factors for primary myelofibrosis is radiation exposure, industrial 14:07 solvent 14:08 exposure, including benzene and toluene, also age greater than 65 is a risk 14:18 factor. 14:20 Primary myelofibrosis is a disorder on its own, however there is also secondary 14:27 myelofibrosis 14:28 and secondary myelofibrosis is caused by another disease or disorder. 14:35 A common cause for secondary myelofibrosis is the other myeloproliferative 14:42 disorders. 14:43 30% of polycythemia rubra vera can lead to secondary myelofibrosis, as well as 14:51 a high 14:52 percentage of essential thrombocythemia can also lead to secondary myelofib 15:02 rosis. 15:03 Blood presents with signs and symptoms suggestive of primary myelofibrosis and 15:08 other hematological 15:09 diseases. 15:10 A full blood count needs to be performed, which will reveal anemia, hemoglobin, 15:17 less 15:17 than 10 grams per deciliter, it can go as low as 8. 15:22 A blood smear is performed, a peripheral blood smear, and in myelofibrosis will 15:29 show 15:30 nucleated red blood cells, which is abnormal, as well as tear drop shaped red 15:35 blood cells, 15:36 also known as dachrosites. 15:39 A side note, dachro comes from the Greek word which relates to tears or the lac 15:44 rimal ducts. 15:47 Anisocytosis means red blood cells of unequal size, which is also a feature 15:56 seen in myelofibrosis. 16:00 Thrombocytosis, including full blood count, may show luchocytosis, or thrombocy 16:04 tosis, 16:05 or luchopenia, and thrombocytopenia. 16:10 Thrombocytopenia, or low levels of platelets in the blood, is usually signs of 16:15 later stage 16:16 of the disease. 16:19 Other blood investigations look for nonspecific abnormalities. 16:24 These include liver function tests, which show an increase in alkaline phosphat 16:30 ase. 16:31 There can also be an increase in lactate dehydrogenase because of the increase 16:34 in cell turnover. 16:37 Electrolyte urea creatinine can show increase in uric acid because of the 16:41 increase in cell 16:42 turnover. 16:43 There can also be an increase in vitamin B12 levels, which reflects the 16:47 increase in 16:47 neutrophil mass. 16:51 Another investigation in primary myelofibrosis is checking for CD34. 16:56 CD34 cell count is increased in some primary myeloproliferative patients. 17:04 Also, the JAC2 mutation is found in about 50% of primary myelofibrosis. 17:11 Important note to make here is that JAC2 mutation is a common feature of most 17:18 of the 17:18 classic myeloproliferative disorders. 17:24 Bone marrow examination is very important, part of investigating, and helps in 17:29 diagnosing 17:30 myelofibrosis. 17:32 There are three bone marrow investigations. 17:36 Bone marrow aspiration, bone marrow biopsy, and bone marrow imaging using MRI. 17:44 Bone marrow aspiration can be initially performed. 17:47 Bone marrow aspiration essentially is aspirating things from the bone marrow, 17:52 typically done 17:53 on the pelvic bone. 17:56 However, bone marrow aspiration is not diagnostic, and performing the bone 18:01 marrow aspiration results 18:03 in a dry tap. 18:05 It's a dry tap because of the fibrotic tissue in the bone marrow, which leads 18:09 to nothing 18:10 coming out. 18:13 Bone marrow biopsy, on the other hand, helps in diagnosing myelofibrosis. 18:19 The bone marrow biopsy is necessary to demonstrate fibrosis. 18:27 Here is a biopsy needle which is being drilled into through the bone and into 18:32 the bone marrow. 18:34 It is then used to obtain bone marrow tissue for histological examination. 18:42 The final bone marrow investigation includes imaging, for example using an MRI. 18:49 The diagnosis of myelofibrosis is based on the World Health Organization Crit 18:55 eria in 2008, 18:58 and need to include most of the following listed. 19:03 One, a bone marrow biopsy which shows mega-cariocyte proliferation, as well as 19:10 collagen and 19:11 reticulum deposition throughout, jack 2 or MPL mutation. 19:25 There can be leukoerythroblastosis, signs of anemia, or an increase in lactate 19:33 dehydrogenase, 19:37 a palpable splenomegaly, and other differential diagnosis has to be ruled out. 19:47 Not all of this have to be met in order to diagnose primary myelofibrosis, but 19:52 the majority 19:52 needs to be met.