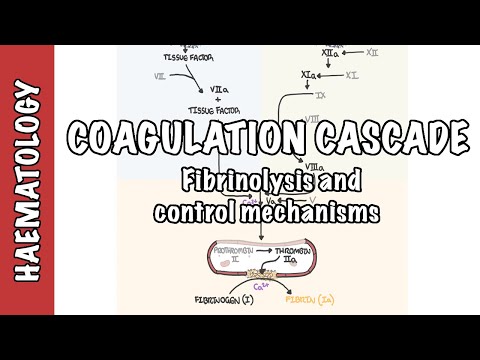
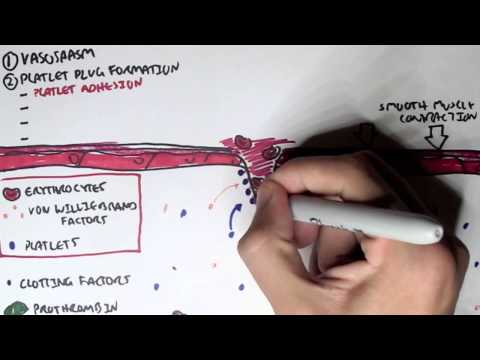
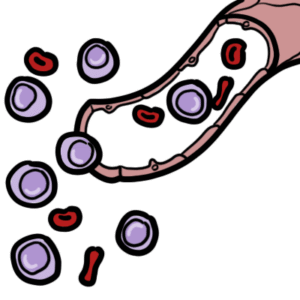
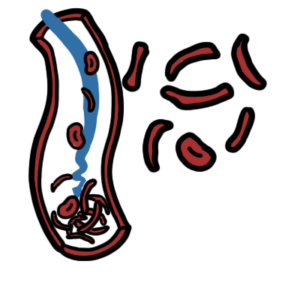
0:00 Hello, in this video, we're going to talk about thrombocyropenia. 0:10 Thrombocyropenia, which means low platelets, is associated with a variety of 0:16 conditions. 0:17 Thrombocyropenia is defined as a platelet count below the lower limit of normal 0:22 , which 0:22 is less than 150,000 microlures, or less than 150,000 cubic millimeters. 0:29 Plates are produced in the bone marrow from mega-cariocyte. 0:33 Each mega-cariocyte produces 1,000 to 5,000 platelets. 0:37 Plates play a key role in hemostasis, forming a temporary plug. 0:42 Therefore, if you have low platelets, you are unable to form a temporary plug 0:47 and tend 0:48 to bleed more easily. 0:50 In order to understand platelet function, we need to revise hemostasis. 0:54 This involves three main phases, phasor constriction, platelet plug formation, 0:59 and coagulation. 1:01 When there's injury to the blood vessel, phasor constriction occurs to reduce 1:04 blood 1:04 flow and therefore reduce blood loss. 1:08 Platelets, red blood cells, and other clotting factors, including von Wille 1:11 brand factors, 1:11 are circulating in the blood. 1:15 The second step in hemostasis is platelet plug formation, where platelets bind 1:19 onto the 1:20 exposed collagen in the injured vessel, with the help of von Willebrand factor. 1:29 Zooming into the area, on the right is the lumen of the blood vessel, the endot 1:34 helial 1:34 lining, collagen layer, smooth muscle cells. 1:39 There are three main steps in the formation of the temporary platelet plug. 1:44 Adhesion, this is where platelets bind onto exposed collagen with the help of 1:48 von Willebrand 1:49 factor and then become activated. 1:52 Here you can see platelet and von Willebrand factor binding onto the exposed 1:58 collagen. 1:59 The second is platelet activation. 2:02 The activated platelets release thromboxin A2 and ADP to recruit more platelets 2:11 . 2:11 So here you can see the platelets releasing ADP and thromboxin A2, which in 2:17 turn will 2:17 activate and recruit more platelets. 2:20 This will lead to platelet aggregation. 2:23 Thromboxin A2 and ADP recruits more platelets, which in turn recruits more and 2:28 more platelets 2:29 forming the temporary platelet plug. 2:35 Platelets do not adhere or agriate to the healthy endothelium, because the 2:39 healthy endothelial 2:39 tissues release nitric oxide and prostacyclins. 2:44 These chemicals prevent platelets to agriate onto these healthy cells. 2:52 After the temporary platelet plug is formed, the last part of hemostasis occurs 2:57 called 2:57 coagulation. 3:00 Coagulation occurs when clotting factors become activated following a series of 3:04 clotting cascades, 3:06 which will eventually activate clotting factor 2, known as prothrombin to throm 3:13 bin. 3:13 The thrombin then activates fibrinogen to form fibrin. 3:18 Fibrin, which is clotting factor 1, will form a fibrin mesh. 3:23 Bazel constriction, platelet plug formation and coagulation completes hemost 3:29 asis. 3:30 After the tissue heals, the fibrin is slowly cleared up, and a new lining of 3:35 endothelial 3:37 tissue is formed. 3:40 It therefore makes sense that if someone has thrombocytopenia, hemostasis is 3:44 disrupted, 3:45 and the formation of the temporary platelet plug is not so good. 3:49 Clinically, features such as easy bruising, TCA, and even bleeding of the gums 3:54 and poor 3:54 wound healing can occur, if platelet levels are low enough. 4:00 Platelets are produced in the bone marrow by megacaryocytes, which are derived 4:04 from 4:05 the multipotent hematopoietic progenitor cells from the Mylar lineage. 4:12 Thrombopoasis is stimulated by thrombopoietin, and inflammation, such as from 4:17 cytokines into 4:18 leukin-6. 4:20 When the megacaryocytes are formed in the bone marrow, eventually they will 4:23 release 4:24 and produce each about 1,000 to 5,000 platelets. 4:29 When platelets are new, they are known to be Cl related. 4:34 They contain Clic acid on their surface. 4:37 Platelets enter circulation. 4:40 At least one third of platelets are actually sequestered in the spleen at any 4:47 one time. 4:48 Platelets actually live for about 7 days before being cleared up by the body. 4:53 When platelets age or become damaged, their morphology changes. 4:57 For example, they become decelerated and need to be cleared up by the body. 5:03 The clearance of platelets occur in the reticular endothelial system, such as 5:07 in the liver 5:08 and the spleen. 5:10 Platelets are removed by monocytes of the reticular endothelial system, also 5:14 known as 5:14 a mononucleophagocyte system. 5:17 Using this simple diagram of the platelet's life cycle, we can categorize and 5:21 understand 5:22 how thrombocytopenia occur. 5:25 Any conditions can cause thrombocytopenia. 5:28 Let's look at some of these. 5:31 One possible mechanism is through reduced production of platelets, such as in 5:35 bone marrow disorders, 5:37 such as bone marrow failure and acute leukemia. 5:41 Malignancy through bone marrow infiltration. 5:44 Alcohol can actually directly induce bone marrow toxicity, reducing production 5:49 of mega 5:49 carrier sites and hence platelets. 5:55 All of these causes essentially will lead to disruption in thrombopoasis. 6:02 Another cause of thrombocytopenia is where the platelets are all used up. 6:06 This is called platelet consumption. 6:09 This occurs in conditions such as disseminated intravascular quagulopathy, th 6:14 rombotic micro 6:15 angiopathy, such as in thrombotic thrombocytopenia perpura and hemolytic urimic 6:21 syndrome, which 6:21 are also important causes of hemolytic anemia. 6:25 Another cause of platelet consumption is heparin-induced thrombocytopenia. 6:31 Heparin-induced thrombocytopenia occurs when the anticoagulant heparin is 6:37 administered. 6:38 Heparin binds with a platelet factor, which is produced by the platelets, 6:42 forming a heparin 6:43 platelet factor complex. 6:46 This triggers the immune system to make antibodies against the heparin platelet 6:50 factor complex. 6:52 When the antibodies binds onto this complex, it stimulates platelet activation 6:58 and aggregation. 7:00 This means increased platelet consumption resulting in thrombocytopenia. 7:06 Heparin-induced thrombocytopenia requires administration of heparin, and the 7:09 effects 7:10 typically occur four to five days after the administration of heparin. 7:15 Splenomegli is another cause of thrombocytopenia. 7:18 Approximately one-third of platelets are sequestered in the spleen, or reciting 7:22 the spleen, to 7:23 maintain normal circulating platelet numbers. 7:26 Conditions that increase the spleen size, therefore, can reduce platelets' 7:30 number 7:30 in circulation. 7:33 Causes of splenomegli include portal hypertension, secondary to liver disease, 7:37 and felty syndromes, 7:38 such as seen in rheumatoid arthritis. 7:42 Another cause of thrombocytopenia is dilutional causes from massive fluid 7:47 resuscitation, which 7:48 can reduce the number of platelets in circulation temporarily. 7:53 Another category of thrombocytopenia can be due to increase in platelet 7:58 destruction. 7:59 Platelets survive in circulation for about seven days after which they are 8:02 removed by 8:03 monocytes and macrophages of the reticular endothelial system, such as the 8:07 liver and 8:08 the spleen. 8:09 Some conditions accelerate platelet destruction, as well as mega-cariocyte 8:13 destruction, including 8:15 idiopathic thrombocytopenic perpera, or ITP. 8:19 ITP can be primary or secondary to rheumatological conditions, such as SLE. 8:26 ITP occurs when antibodies attack platelets, increasing the clearance rates. 8:32 Drug-induced ITP is also important to remember. 8:36 Important to note that a variant of ITP can include the antibodies attacking 8:42 the mega-cariocytes 8:44 in the bone marrow, which means less platelet production. 8:49 Finally, infection is another very important cause of thrombocytopenia, which 8:55 occurs through 8:56 a number of mechanisms, via ITP, so immune mediated, bone marrow suppression, 9:02 as well 9:03 as platelet consumption. 9:08 Clinical features of thrombocytopenia include skin changes, which are probably 9:12 the most 9:13 important finding. 9:14 These include perpera and petique, mucosal bleeding. 9:19 Depending on the cause of the thrombocytopenia, you can have lymphadenopathy if 9:24 the cause is 9:25 infective, splenomegli, and hepatomegli if there is portal hypertension or even 9:32 malignancy. 9:33 But you know that the difference in presentation between someone also you have 9:38 the constitutional 9:40 symptoms, of course, such as fever, loss of appetite, which could mean infect 9:45 ive or 9:45 it could mean malignant. 9:48 I hope you enjoyed this video on thrombocytopenia. 9:50 Thank you.