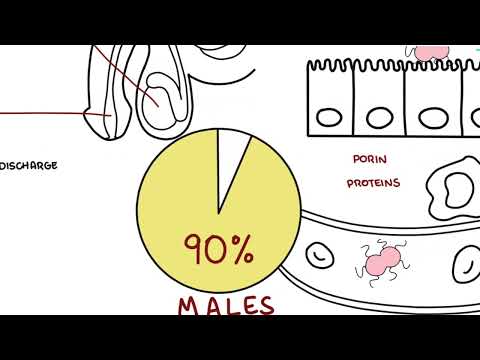
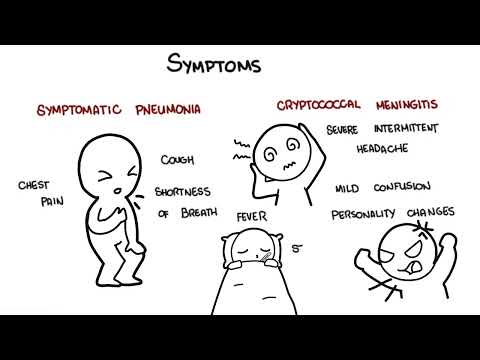
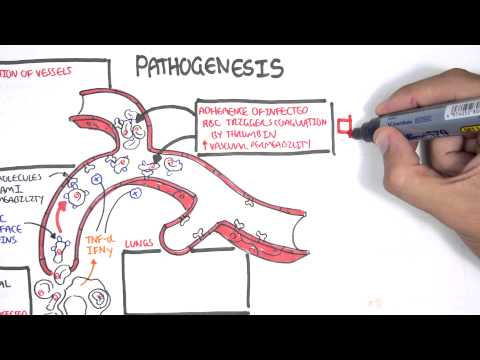
0:00 Hello, in this video, we're going to talk about urinary tract infections. 0:06 This is an overview and introduction. 0:08 It is important to revise the anatomy of the urinary system, specifically the 0:15 urinary tract. 0:17 Let us begin by looking at the male. 0:19 Here we have the kidney. 0:21 Coming off the kidney is the ureter, which carries urine into the bladder. 0:27 Here we have the glands penis, the penis, and the urethra. 0:33 Below the bladder we have the prostate. 0:37 Coming past the prostate and into the urethra is the seminal vesicles, an 0:41 important part 0:42 of semen production. 0:45 Then we have the vas deferens, the actual tube that runs from the testes, and 0:51 the testes 0:51 is where sperm is produced. 0:56 The female anatomy is very similar, except importantly they have a shorter u 1:03 rethra. 1:05 With a shorter urethra means that they are at increased risk of developing UTI. 1:13 Causative agents of UTI are mainly E. coli in 90% of cases. 1:19 Factors include interobacteria, proteas, myrbalis, and Klebsyla pneumonia. 1:26 They essentially enter the urethra and colonize the area, or bladder, because 1:31 of a variety 1:32 of reasons and risk factors, and eventually can cause a urinary tract infection 1:39 , a UTI. 1:40 The bacteria will cause a lower UTI usually. 1:45 And this can be either cystitis, which is infection of the bladder, prostatitis 1:52 , which 1:52 is infection of the prostate gland, and urethritis, which is infection of the u 2:01 rethra. 2:02 Infection of the lower urinary tract can progress and cause an upper urinary 2:08 tract infection. 2:09 This is where infection affects the kidneys. 2:18 Interestingly, as we know, urinary tract infections are more common in women. 2:27 And up to one third of women with symptoms of urinary tract infections have 2:33 actually 2:34 negative midstream urine samples revealing any form of infection. 2:41 That was a side note. 2:43 But anyway, how does a UTI occur? 2:47 Let's look at the pathophysiology. 2:50 Here again is the kidney, the ureter, the bladder, the urethra. 2:56 Here we have the inferior vena cava, and the renal vein comes from the kidney 3:01 and enters 3:02 the inferior vena cava. 3:04 Behind the inferior vena cava we have the descending aorta, which will supply 3:08 the kidneys with 3:09 the branching renal artery. 3:13 So what initially happens, one is contamination. 3:17 Bacteria contaminates the lower urinary tract because of certain risk factors. 3:23 Let's just say the bacteria is E. coli because it is the most common in 80% of 3:29 cases. 3:30 They initially colonize the urethra and the bladder. 3:33 This triggers an inflammatory response in the lower urinary tract. 3:38 Neutrophils are then recruited to this area. 3:42 As you can see in the bladder you have bacteria and you have neutrophils. 3:47 The bacteria multiply and they are able to evade the immune system because of 3:52 certain 3:53 virulent factors. 3:56 Bia for example can bind to cells in the lower urinary tract and hide from 4:01 immune cells. 4:02 The bacteria can form biofilums. 4:06 A biofilum is any group of microorganisms in which they stick to each other and 4:13 often 4:13 these microorganisms adhere to surfaces and it allows them to survive. 4:20 If this urinary tract infection progresses and left untreated or if the patient 4:25 is immunocompromised 4:27 has risk factors, the bacteria can ascend towards the kidneys and then colonize 4:32 the 4:33 kidneys causing an upper urinary tract infection. 4:39 And then from here, if left untreated, the bacteria can spread into circulation 4:44 via the 4:45 renal veins causing worst case septic shock. 4:51 A big risk factor for developing urinary tract infections especially in females 4:56 is urinary 4:57 catheterization. 5:00 Same thing happens, the catheter can introduce infections straight into the 5:04 bladder if not 5:05 done hygienically. 5:07 The bacteria colonizes the bladder initiating an immune response. 5:13 Your fills enter further promoting inflammation. 5:17 Fibrinogen accumulates on the catheter providing an ideal environment for the 5:21 attachment of 5:22 uropathogens that express fibrinogen binding proteins. 5:28 After these bacteria initial attachment to the fibrinogen coated catheters, the 5:33 bacteria 5:33 can multiply and they can again form biofilums, promote epithelial damage and 5:40 can seed infection 5:41 of the kidney. 5:44 And so the same story occurs. 5:47 In pregnancy, urinary tract infections are common. 5:51 Catheterization will almost always result in a urinary tract infection. 5:57 The reason being is not only is the urethra shorter in women but during 6:03 pregnancy, progesterone 6:05 relaxes smooth muscle causing stasis of urine which allows for colonization, 6:12 especially 6:13 up to the kidneys. 6:15 During pregnancy it is important to perform urine analysis because not only are 6:20 urinary 6:21 tract infections more common but are also asymptomatic. 6:26 Untreated urinary tract infections during pregnancy can have consequences for 6:30 the growing 6:31 infant in utero. 6:35 So now let's talk about risk factors for UTIs. 6:39 These include pregnancy, being female, menopause because it's dry in the vagina 6:44 and the urethra, 6:46 sexual intercourse, condoms, catheterization, urinary tract malformation and 6:54 urinary stones 6:55 are also risk factors. 6:59 The signs and symptoms of UTI depend on where the infection is, if it is lower 7:05 urinary tract 7:06 infection or if it's an upper urinary tract infection, upper being the more 7:11 severe. 7:12 Lower urinary tract infections cause dysuria, pain upon urination, frequency, 7:18 hematuria, 7:19 blood in urine, super pubic discomfort and a burning urgency sensation with ur 7:26 ination. 7:27 The urine is often described as being cloudy and having an offensive smell. 7:33 Upper urinary tract infections can have the same types of symptoms but class 7:38 ically, malase, 7:40 fever, rycles, vomiting and loin-flank pain radiating to the back. 7:47 There can be signs of shock if the infection is more severe. 7:52 The classic triad for upper urinary tract infections or hyalonephritis is 7:58 vomiting, flank loin 7:59 pain and fever. 8:04 Another way to categorize UTI is either being complicated or uncomplicated. 8:11 To put it simply uncomplicated UTI, the renal tract and function are normal. 8:18 With complicated, there is decreased renal function based on investigations and 8:22 symptoms 8:22 and potentially is accompanied by an abnormal urinary tract. 8:31 Let's go through an algorithm of managing urinary tract infection. 8:37 It is important to remember that if there is discharge or itch with signs of UT 8:44 I, perform 8:45 a genital examination with swab to check for a sexual transmitted infection, ST 8:52 I. 8:52 A characteristic of STI is having discharge and a fishy smell within the mucus. 9:01 Other investigations that are performed, importantly a urine dipstick which 9:05 will show 9:06 hematuria, proteinuria, positive nitrates and the presence of urine microscopy 9:13 can be 9:13 performed as well as a urine microscopy culture sensitivity. 9:18 Bloods include full blood count to check for infections, CRP, eta HCG serum to 9:25 check for 9:26 ectopic as a differential diagnosis especially in a young female adult. 9:34 For UTI, if the urinary dipstick is positive, treat with empirical antibiotics. 9:41 If the dipstick is negative, but you still suspect UTI, send for microscopy 9:47 culture sensitivity 9:49 using the urine sample. 9:52 The diagnosis of a UTI is having a bacterial growth on a culture plate of more 9:58 than 10,000 9:59 colony forming units per mil. 10:04 As mentioned, urinary tract infections are common in females. 10:09 And so if a female patient presents with an uncomplicated UTI, she is most 10:14 likely able 10:15 to go home discharged with oral antibiotics. 10:21 The treatment of UTI is essentially empirical antibiotics. 10:26 For lower urinary tract infections, it's typically oral antibiotics, a 3-7 day 10:31 course consisting 10:32 of either trimethoprine, nitro forentroin or amoxicillin. 10:39 Upper UTI are generally more serious and require IV antibiotics initially until 10:45 the fever has 10:46 settled and then moving on to oral antibiotics. 10:50 The course of antibiotics are generally longer with upper urinary tract 10:56 infections. 10:57 Finally, it is important to know when to refer to a renal specialist or urolog 11:05 ist. 11:06 Refer to a urologist if there is failure of the patient to respond to 11:12 antibiotic treatment. 11:14 If there is recurrent UTI, which is defined as having three or more in one year 11:21 . 11:21 Refer to a urologist if a man, a man, have symptoms of an upper urinary tract 11:27 infections. 11:29 And this is because it is very uncommon for men to develop upper UTI and 11:34 potentially could 11:36 be a result of a more sinister anatomical abnormality. 11:42 Finally, refer to urologists also if there is significant hematuria. 11:47 Only preventive measures for UTI include drinking more water, antibiotic proph 11:52 ylaxis, especially 11:53 for females with recurrent UTIs, and cranberry juice, although there are 11:58 arguments for an 12:00 against this. 12:17 for the patient. 12:47 the patient. 13:17 the patient.