Meningitis
5 year old presents with non-blanching rash, fever, headache, photophobia and neck stiffness.
Aetiology
- Up to three months of age
- Group B streptococcus
- E-coli
- Listeria
- Three to 12 years of age
Clinical presentation
- Fever
- Lethargy
- Irritability
- Anorexia
- Nausea/vomiting
- Photophobia
- Neck and back pain/rigidity
- Kernig sign
- Brudzinski sign
Investigations
Treatment
- Resuscitation
- IV dexamethasone
- IV empirical antibiotics – vancomycin and ceftriaxone
- Once organism is identified switch to targeted antibiotic therapy
Complications
- Increase intracranial pressure
- Seizures
- Hearing loss (pneumococcus associated)
- Developmental delay
Pertussis
8 month old presents with paroxysmal cough and fever. Parents states the baby coughs all night and has episodes of post-tussive emesis (vomiting). The baby is not up to date with their vaccination.
Aetiology
Clinical presentation
Differential Diagnosis
Investigations
Treatment
- Prevent with immunisation
- Supportive care
- Antibiotics – macrolide
- Treat other people who lives at home
Scarlet Fever
Overview
Caused by certain strains of group A beta-hemolytic streptococci that release a streptococcal pyrogenic exotoxin.
Clinical Finding
- Fever and sore throat few days before rash
- Strawberry tongue
- Rash
- Erythematous, blanching, fine macules, resembling a sunburn
- Sandpaper-like papules
- Spares the palms
- Sore throat (pharyngitis)
Treatment
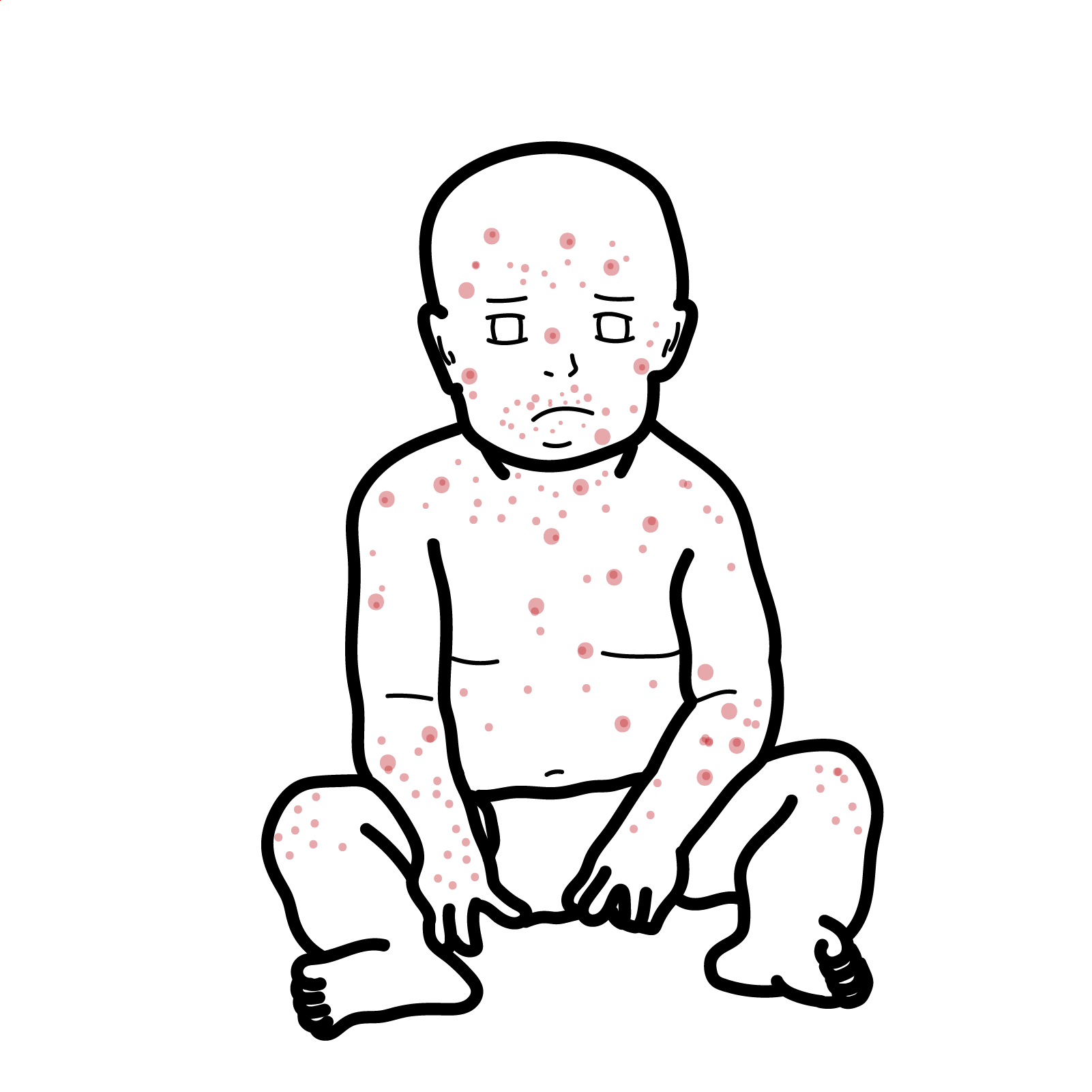
Impetigo
Overview
Contagious local superficial bacterial infection involving the epidermis.
Aetiology
- Staphylococcus aureus
- Group A streptococcus
- Pseudomonas aeruginosa
Risk Factors
- Contaminant skin disease
- Children
- Poor hygiene
- Overcrowding
Classification and features
- Non Bullous Impetigo
- Honey comb crusts
- No blisters (bullous)
- Not Painful
- Bullous Impetigo
Treatment
- Hand hygiene
- Stay home (not school)
- Usually self-resolving if not (or concerned) pharmacological treatment
Complications
Cellulitis
Cellulitis is an acute local inflammatory condition of deep skin layers involving the dermis and subcutaneous fat.
Causative agents – normal skin flora or other bacteria niche to a area.
- S. Pyogenes
- S. Aureus
- Pseudomonas Aeruginosa
- Penetrating injury cellulitis
P. Aeruginosa causes three skin infections cellulitis, ecythma gangrenosum (neutropenic patients) and folliculitis (hot tub).
Classic Clinical feature
- Localised pain
- Erythema
- Swelling
- Heat
Diagnosis
- Wound swab of portal of entry, wound
Management
- Oral Antibiotics
- IV Antibiotics – for severe and at risk patients such as diabetes and immunocompromised

Discussion