Overview
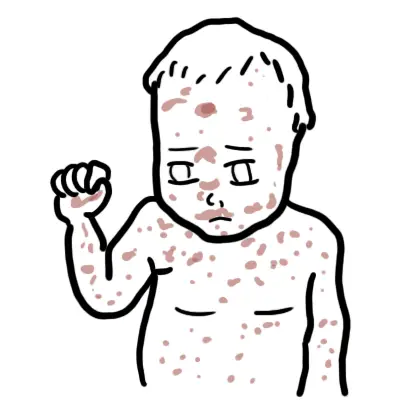
- Atopic dermatitis is a chronic highly pruritic (itchy) inflammatory skin disease.
- Atopic dermatitis and eczema are often used synonymously.
- Atopic dermatitis primarily affect young children and is often associated with other atopic disorders, such as allergic rhinitis and asthma.
- The prevalence of atopic dermatitis has doubled or tripled in industrialised countries during the past three decades.
- Not only are patients affected by the social stigma of a visible skin condition, but the intense itching characteristic of the disease often leads to significant sleep as well.
Atopic dermatitis affects approximately 5 to 20 percent of children worldwide
The incidence of atopic dermatitis appears to be increasing. It may occur in any race or geographic location, although there appears to be a higher incidence in urban areas and developed countries, especially Western societies.
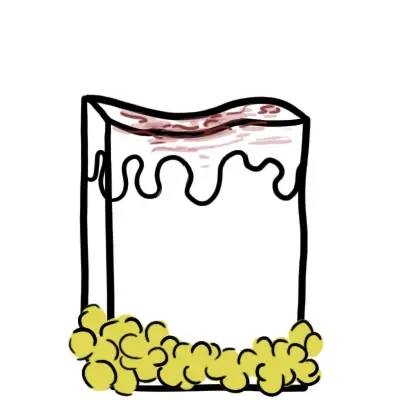
Anatomy
The skin consist of three layers, from superficial to deep:
- Epidermis
- Dermis
- Papillary layer
- Reticular layer
- Hypodermis (some don’t classify it as skin)
The epidermal layer are made up mainly of keratinocytes, which are squamous epithelial cells high in keratin (protein). Other cells residing in the epidermis include:
- Melanocytes – produce melanin
- Langerhan cells – immune cell, basically a dendritic cell of the skin
- Merkel Cells – tactile cells for sensation
| Watch Dermatology Overview |
The epidermis itself can be further divided into 4 or 5 layers, from top to bottom:
- Stratum corneum
- +/- Stratum lucidum
- Stratum granulosum
- Startum spinosum
- Stratum basale
These layers are bound firmly thanks to the Filagrin gene which is responsible for making proteins important for proper skin barrier function, particularly structural proteins in the stratum corneum and granulosum, that help bind keratinocytes together.
Sign and Symptoms
Key clinical features
- Pruritis (itching)
- Xerosis (dry skin)
- Excoriations (scratch marks)
- Hypopigmentation of affected areas
During Flare ups
- Erythema
- Scaling
- Vesicles
- Papules
Chronic
- Lichenification
| Remember Atopic Dermatitis affect mainly flexor surfaces, this differs to psoriasis which classically affect extensor surfaces |
Risk factors
- Age <5 years
- Family History
- Allergic rhinitis
- Asthma
- Antihelminth treatment
Differential Diagnosis
Pruritic (Itchy) skin lesion
- Contact dermatitis
- Scabies
Non pruritic skin lesion
- Seborrhoeic dermatitis
- Psoriasis
| Seborrhoeic dermatitis is a common, chronic or relapsing form of eczema/dermatitisthat mainly affects the scalp and face. It can be associated with psoriasis. Dandruff is an uninflamed form of seborrhoeic dermatitis. |
Investigations
- Clinical Diagnosis of Atopic Dermatitis (See Below)
- Allergy testing (to detect potential triggers and exacerbating facotrs of the dermatitis)
- Serum IgE
- Skin Biopsy (differentiate between contact and allergic dermatitis)
Diagnosis
The diagnosis of atopic dermatitis is clinical, based upon history, morphology and distribution of skin lesions, and associated clinical signs. There is no specific diagnosis and it is controversial but mainly includes:
- Evidence of pruritic skin
- In addition to itchy skin, three or more of the following:
- History of skin creases being involved.
- History of asthma or hay fever
- The presence of generally dry skin within the past year.
- Symptoms beginning <2 years of age.
- Visible dermatitis involving flexural surfaces. For children under four years of age, this criterion is met by dermatitis affecting the cheeks or forehead and outer aspects of the extremities.
Aetiology
Atopic dermatitis can be though of a complex genetic disease arising from several gene gene and gene-environment interactions.
Genes
Many genes have been associated with atopic dermatitis, especially what’s known as the filagrin gene on chromosome 1. 50% of people with atopic dermatitis carry a mutated filigrrin gene .The filagren gene encodes a structural protein essential for skin barrier formation.
Environment
There is thought because of a more westernised industrialised lifestyle more people are developing eczema. This compliments the so called hygiene hypothesis which states that the decrease in early childhood exposure to infections, has increased susceptibility to atopy, tendency towards allergy.
Pathophysiology
Two main hypothesis proposed in atopic dermatitis.
Immunological hypothesis (inside out hypothesis)
- T helper cells differentiate into T helper 1 (Th1) or T helper 2 (Th2)
- Th1 promotes cell mediated immunity (Inflammation)
- Th2 promotes humoral immuniy (antibodies)
- Imbalance of T cells. Th2 differentiation predominate
- Th2 produces:
- IL 4 -> positive loop to produce more Th2
- IL 5 -> stimulates B-cell antibody production
- IL 13 -> stimulates B cell class switching to IgE (Elevated IgE are present in only 50% of patients with AD).
- Increase in IgE leads to hypersensitivity -> allergic response
- Cytokine production also down regulates the production of skin antimicrobials cathelicidins and defences -> predisposes patients to infections (S. aureus)
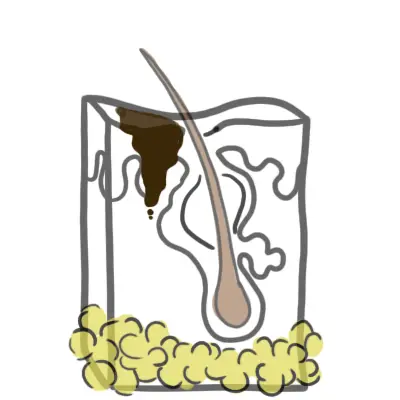
The skin barrier Hypothesis (outside in hypothesis)
- The epidermis is the first line of defence between the body and the environment. The skin barrier keeps environmental irritants, allergens, and microbes from entering the body and prevents excessive water loss.
- Filagrin gene is responsible for making proteins important for proper skin barrier function, particularly structural proteins in the stratum corneum and granulosum that help bind keratinocytes together.
- Mutation in the filagrin gene results in skin barrier dysfunction and water loss which causes eczema.
- Impaired skin barrier also increases penetration of allergens into skin allergic sensitisation to asthma and hay fever.
Histology/Pathology
Pathology
Epidermal intercellular oedema (spongiosis) and a prominent perivascular infiltrate of lymphocytes, monocyte, macrophages, dendritic cells and a few eosinophils in the dermis. In subacute, chronic stages—epidermis is thickened and its upper layer is hypertrophied.
Treatment and Management
Education:
Education on the chronic nature of disease importance of treatment adherence, appropriate use and application of topical therapies.
Skin care:
Use of emolients/moisturizers for hydration of skin.
Topical corticosteroids:
The mainstay first line treatment for Atopic Dermatitis. There are four different classes based on the potency.
Topical calcineurin inhibitors (IL2 Inhibitors):
An alternative to corticosteroids.
Adjuvant therapy:
- Antibiotics and antivirals for infections
- First generation antihistamines for sleep disturbances
| Pharmacology Calcineurin is a IL2 inhibitor, technically it is a Calmodulin inhibitor. Calmodulin is an activator of a powerful transcription factor NFkb, which promotes IL2 production in immune cells. IL2 normally promotes the inflammatory response by recruiting more lymphocytes to the tissue. Inhibiting Calmodulin suppresses IL2 production and so suppresses the inflammatory response. Oral calcineurin is used in Rheumatoid arthritis and other rheumatological conditions. Side effects of topical calcineurin is minimal. |
Complications and Prognosis
Complications
- Psychological stress
- Side effects of Corticosteroids
- Bacterial Infections
Prognosis
- Atopic dermatitis is a chronic disease with a varying course.
- Approximately 60% of children will have symptom resolution as they enter puberty, but relapse may occur in 50%
References
New England Journal of Medicine - Mechanism of Disease Atopic Dermatitis
Best Practice
UpToDate