| Watch Diverticular Disease |
Overview
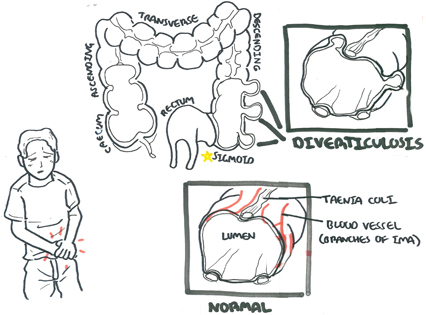
Overview Diverticula of the colon consist of outpouchings of mucous membrane through the muscle wall of the bowel. In the colon, diverticula are found most commonly in the sigmoid and descending colon, and become increasingly rare in passing from the left to the right side of the colon. They are unusual before the age of 40 years, but they are found in about 30% of all autopsies in the elderly.
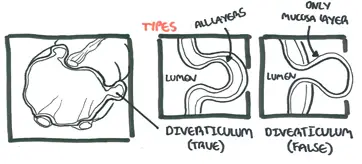
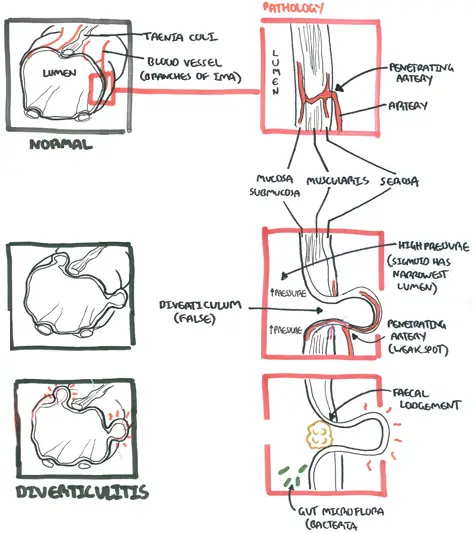
| Definitions Diverticulum: abnormal sac-like protrusion from the wall of a hollow organ Diverticulosis: presence of multiple diverticula, not symptomatic Diverticulitis: inflammation of diverticula Diverticular Disease: Complication of diverticulosis True (congenital) diverticuli: contain all layers of colonic wall, often right-sided (i.e Merkel's Diverticulum) False (acquired) diverticuli: contain mucosa and submucosa, often left-sided (highest pressure) Merkel's Diverticulum: A true diverticulum, it is a reminant of proximal part of the yolk-stalk. May present with symptoms in a small majority of patients. |
Colon Anatomy and Physiology
The colon is divided into:
- Caecum (appendix off this)
- Ascending colon
- Transverse colon
- Descending colon
- Sigmoid colon
- Rectum
The ascending and descending colon are retroperitoneal, these are immobile. The transverse is mobile and lies within the peritoneal cavity. The transverse colon is supported by the greater omentum superiorly and attaches to the posterior abdominal wall (in front of the retroperitoneal cavity) by the transverse mesocolon.
The transverse colon is attached to the greater curvature of the stomach and first part of the duodenum via the greater omentum. The sigmoid colon is also attached
Main features of large intestine structure:
- Complete layer of circular smooth muscle throughout, but incomplete bands of longitudinal muscle (taeniae coli) in colon (stops at the rectum)
- Fatty appendages along taeniae (appendices epiploicae)
- Folded internal mucosal appearances (haustrations)
- ‘Segmented’ external appearances (sacculations)
Blood supply - from superior and inferior mesenteric artery
- Superior mesenteric artery
- Ileocolic artery - last terminal ilealloop, caecum
- Right colic artery - ascending colon
- Middle colic artery - transverse colon up to the splenic flexure
- Inferior mesenteric artery
- Left colic - splenic flexure and descending colon.
- Sigmoid artery - sigmoid colon
- Superior rectal artery - rectum and upper anal canal
Autonomic nerve supply
- Sympathetic, mainly from greater splanchnic nerves via SMA and IMA plexuses.
- Parasympathetic, from vagus via SMA and IMA plexus from caecum to splenic flexure and from pelvic parasympathetics (S2, 3, 4) via hypogastric plexuses and retroperitoneal nerves from splenic flexure to upper anal canal
The colon is about 1.5 metres long, transverse being the longest and most mobile. The ascending and descending colon are fixed by the mesentery and do not move.
| Watch The Colon (and Colon Cancer) |
Risk Factors
| Risk Factors |
| Age >50 |
| Low fiber diet |
| Western diet |
| Obesity |
| NSAIDs |
Signs and Symptoms
Differential Diagnosis
- Ectopic Pregnancy
- Colorectal Cancer
- Meckel’s diverticulum
- Appendicitis
- Inflammatory Bowel Disease
- Mesenteric Ischaemia
- Pyelonephritis
- Urinary Tract infection
- Pelvic Inflammatory Disease
- Irritable Bowel Syndrome
Investigation
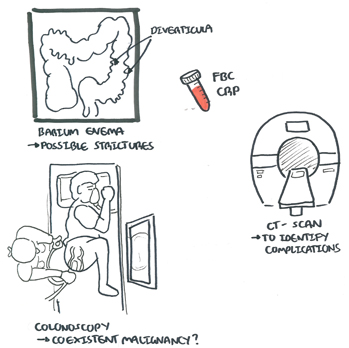
Investigations depend on suspected complication and for diagnosis of diverticular disease. Diverticulosis may be an incidental finding on colonoscopy. Laboratory tests include FBC and CRP to check for bleeding and signs of inflammation/infection/malignancy. CT scan can help identify complications. A Chest x-ray can also be used which may reveal free air under the diaphragm (sign of perforation)
| Remember On CT scan diverticulitis will have wall thickening (4mm) and surrounding oedema (inflammation) and signs of fat stranding. |
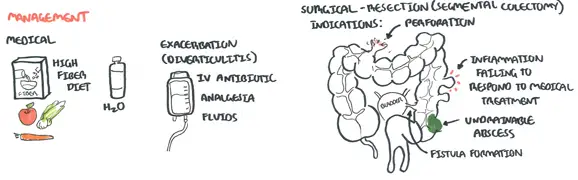
Management
Diverticulitis - Conservative therapy
- NBM
- Fluids
- IV Antibiotics
- IV analgesia
| Indications for surgery |
| Failure of medical therapy |
| Wide-spread inflammation |
| Bowel obstruction |
| Abscess and fistula formation |
| Stenosis |
| Recurrent bleeding |
| Unacceptable symptoms for patients |
| Hinchey Staging and Treatment of Diverticulitis | ||
| Stage | Feature | Treatment |
| I | Phlegmon/small pericolic abscess (Localized) | Medical |
| II | Large abscess/fistula | Abscess drainage, resection +/- anastomsosis |
| III | Purulent peritonitis (ruptured abscess) | Hartmann procedure |
| IV | Feculent peritonitis | Hartmann procedure |
Complications
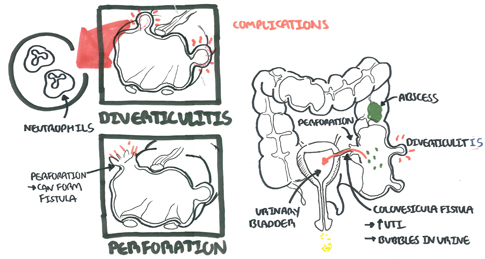
An inflamed diverticulum (diverticulitis) may do one of three things.
- Perforation
- Into peritoneal cavity to causing peritonitis
- Into the pericolic tissues with formation of a pericolic abscess
- Into adjacent structures (e.g. bladder, small bowel, vagina), forming a fistula.
- Produce chronic infection with inflammatory fibrosis, resulting in obstructive symptoms
- Haemorrhage, as a result of erosion of a vessel in the bowel wall. The bleeding varies from acute and profuse to a chronic occult loss.
Merkel's Diverticulum
Meckel’s diverticulum is the remnant of the vitellointestinal duct of the embryo. It lies on the antimesenteric border of the ileum and, as an approximation, occurs in 2% of the population, arises 55cm (2 feet) from the caecum, and averages 5 cm (2 inches) in length.
| Remember Merkel's Diverticulum is a true diverticulum |