Overview
Overview
| Definition Ankle-Brachial Index (ABI): Ratio of ankle to brachial systolic blood pressure, determined using Doppler ultrasound flow. Claudication: Pain, ache, or cramp in muscles that increases with walking or leg exertion in a predictable manner and resolves with rest. Peripheral arterial disease: Atherosclerosis leading to narrowing of the major arteries distal to the aortic arch. It can involve both the upper and lower extremities Acute Limb ischemia: Sudden decrease in the blood flow to a limb, resulting in a potential threat to the viability of the extremity Chronic Limb ischaemia: Peripheral vascular disease Critical Limb ischaemia: severe obstruction of the arteries which markedly reduces blood flow to the extremities (hands, feet and legs) and has progressed to the point of severe pain and even skin ulcers, sores, or gangrene. T |
Classification
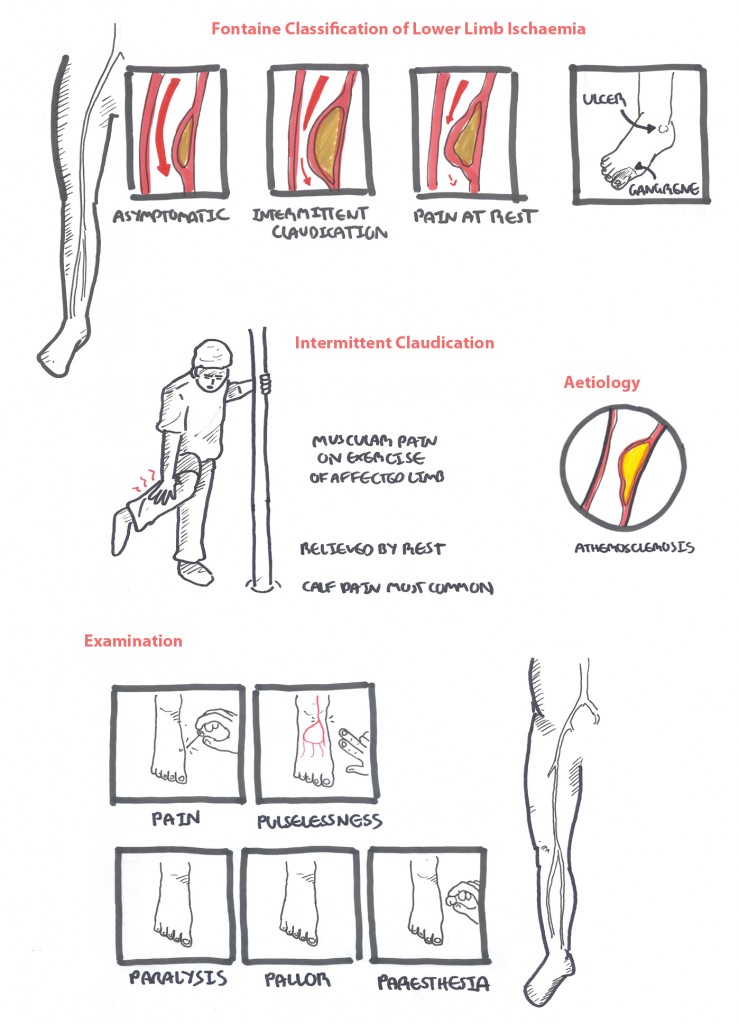
| FONTAINE STAGE CLASSIFICATION OF PVD | |
| Stage I | Asymptomatic, decreased pulses, ABI <0.9 |
| Stage II | Intermittend claudication |
| Stage III | Daily rest pain |
| Stage IV | Focal tissue necrosis |
Risk Factors
| Risk Factors |
| Cardiovascular risk factors |
| Atrial fibrillation |
| Recent MI |
| Aortic athersclerosis |
| Aneurysm |
| Prior vascular surgery |
| Deep vein thrombosis (paradoxical embolism) |
Risk Factors The most important risk factors for PAD are cigarette smoking and diabetes mellitus. Hypertension, dyslipidemia, and elevated homocysteine levels also play significant roles.
Clinical Manifestation
Peripheral arterial disease is atherosclerosis leading to narrowing of the major arteries distal to the aortic arch. Progressive occlusion results in arterial stenosis, reduced blood flow, and claudication, the most common presenting symptom
Examination - The 6 P's
- Pain (absent in 20% of cases)
- Pulse
- Pallor (within a few hours becomes mottled cyanosis)
- Pressure (pain on stretch, firm, tense)
- Paresthesia
- Paralysis
Physical examination findings may include cool skin; nonpalpable distal pulses; auscultation of bruits over the iliac, femoral, or popliteal arteries; abnormal capillary refill time; nonhealing wounds; shiny skin; absence of hair in the affected area; and distal extremity pallor on elevation
Differential Diagnosis
Differential diagnosis of Claudication
- Arthritis
- Chronic compartment syndrome
- Muscle strain
- Baker's cyst
- Nerve entrapment
- Nerve root compression
- Spinal stenosis
- DVT
- Vasculitis
| DIFFERENCES BETWEEN TYPES OF CLAUDICATION | |||
| Arterial - Intermittent (atherosclerosis) | Neurogenic (Lumbar spinal stenosis) | Venous (Deep vein thrombosis) | |
| Pain | Pain is in the muscle of the calf, thigh or buttock | Pain is in whole leg ca be associated with tingling and numbness | Involvement of whole leg. Patients may describe feeling their leg is going burst |
| Unilateral or Bilateral | Unilateral in femoropoliteal disease. Bilateral in aortic-iliac disease | Bilateral | Most commonly unilateral |
| Provoking facotrs | Gradual onset after walking "claudication distance" | Comes on suddenly on standing or walking | Gradual onset after beginning to walk |
| Relieving factors | Pain is relieved by rest | Relieved by sitting down, bending over and stopping walking | Relief on elevating the leg |
| Unable to straighten legs | |||
| Pulses/ABIs | Absent/reduced pulses | Absent/reduced pulses | Normal |
| Skin and tissue changes | Mottled skin, Gangere | Absent | Cyanosed, Oedematous |
Investigations
- FBC
- Serum glucose
- β-hCG
- Coagulation profile
- Lipid profile
- Ultrasound (Colour-duplex ultrasound)
- CT - needs to be done before surgery
- Surgery
When peripheral artery disease is suspected, the test most commonly used to evaluate for arterial insufficiency is the ankle-brachial index (ABI). Normally, blood pressures in the large arteries of the legs and arms are similar. In PVD this is different.
| Reference Values of ABI | |
| Ankle pressure is somewhat high | ≥1.30 |
| Normal | 1.00 - 1.29 |
| Borderline normal | 0.91-0.99 |
| Mild peripheral vascular disease | 0.41-0.90 |
| Severe peripheral vascular disease | ≤0.40 |
| Think In diabetic vessels there are calcification of arteries. This means it can give false ABI readings. Thus different sites of compression (toes) are used. |
| Ankle-brachial index is the ratio of the ankle blood pressure to the highest brachial systolic pressure. Ankle blood pressure is obtained by inflating a blood pressure cuff above the ankle and detecting the return of the dorsalis pedis or posterior tibial artery pulse by Doppler ultrasonography as the cuff is slowly deflated |
Diagnosis clinical history and physical examination findings may suggest a diagnosis of PAD, especially in patients with multiple risk factors or classic claudication + Ankle-brachial index.
Management
Management of Chronic Limb Ischaemia
- Lifestyle Modification
- Control Blood Pressure
- Analgesia
- Statin
- Antiplatelet therapy (to reduce risk of cardiovascular events)
- Surgery
- Angioplasty +/- Stenting
- Endarterectomy
- Bypass
Prognosis
- 70% to 80% had stable claudication
- 10% to 20% had worsening claudication
- 1% to 2% progressed to critical limb ischemia over five years.
- The rate of limb amputation at five years is estimated to be 1% to 4%
Acute Limb Ischaemia
Overview This section will mainly focus on acute limb ischemia, which is any sudden decrease in limb perfusion that causes a potential threat to viability. Patients who present later than two weeks after the onset of the acute event are considered to have chronic limb ischemia. Surgical thromboembolectomy and bypass grafting were the mainstays of therapy for many years. Subsequently, thrombolytic therapy and percutaneous transluminal angioplasty (PTA) have become treatment options for selected patients. Despite these advances, the morbidity, mortality, and limb loss rates from acute lower extremity ischemia remain high
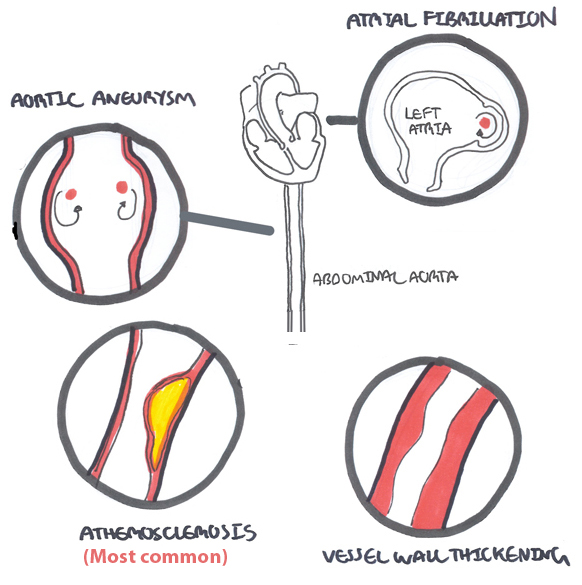
Aetiology
Acute thrombosis in a vessel with existing atherosclerosis (60%)
Emboli (30%)
- Cardiac cause (ie. Atrial fibrillation) (80%)
- Aortic Aneurysm
Rare causes
- Aortic dissection
- Trauma
Examination - The 6 P's
- Pain (absent in 20% of cases)
- Pulse
- Pallor (within a few hours becomes mottled cyanosis)
- Pressure (pain on stretch, firm, tense)
- Paresthesia
- Paralysis
| ASSESSING SEVERITY BASED ON EXAMINATION | |||||
| Pain/Pressure | Pulse | Pallor | Parasthesia | Paralysis | |
| Non-viable | Variable/ Woody hard muscle | Absent | Fixed mottling of skin | Complete deficit | Profound/ Complete |
| Threatened | Severe/ Tender to touch (swollen) | Absent | Blue - Pale | Partial deficit | Partial |
| Viable | Mild | Present | Pale | No sensory deficit | None |
Management
| Remember Patients will usually have co-excisting coronary, cerebral, or renal disease |
Resuscitation Acute Limb Ischaemia- Emergency
- Oxygen
- Fluids IV
- Analgesia IV
- Call for senior help
- Assess severity (6 P's)
- IV Heparin (check APTT every 4-6 hrs), aim for target time of 2-2.5x normal range
| Remember Acute arterial occlusion that threatens limb viability is a medical emergency and requires immediate anticoagulation and investigation with conventional arteriography. |
Definitive Management (Depending on severity)
- Nonviable - amputation
- Threatened - manage sign/symptoms of muscle necrosis (hyperkalaemia, acidosis, ARF and cardiac arrest). Identify cause (ie. atherosclerosis). Surgery to revascularise and perform fasciotomy if need to prevent compartment syndrome. Consider amputation if ischaemic changes advanced and life-threatening.
- Non- threatened - Initiate thrombolytic treatment. Surgery and revascularisation will most likely be required.
| Remember Smoking cessation is the single most important intervention for atherosclerotic peripheral vascular disease. Other treatments include pentoxifylline or cilostazol, regular exercise, and cardiovascular risk factor modification. |
Acute vs. Chronic limb Ischaemia (PVD)
| Acute | Chronic | |
| Aetiology | Sudden obstruction of an artery due to an embolus or thrombosis. | Slowly progressing disease process that is usually due to atherosclerosis causing obstruction |
| Claudication | No history | Usually Present |
| Site | Lower extremity | Lower extremity |
| Management | Urgent as limb can progress to irreversible ischaemia and myonecrosis within 6 hours. | Conservative and surgery if severe lifestyle impairment, vocational impairment, critical ischemia |
| Prognosis | ~15% mortality and up to 40% morbidity (amputation | Claudication therapy (60-80% improve, 20-30% stay the same, 5-10% deteriorate, 5% amputation). For patients with critical ischemia high risk of amputation (carries 25% risk of death at 1 year) |
References
Oxford Handbook of Clinical Surgery
Oxford Handbook of Clinical Medicine
Toronto Essential Notes
Hennion, D. & Siano, KA. (2013). Diagnosis and Treatment of Peripheral Arterial Disease. American Family Physician. 88(5). 306-310.
This section focuses on Limb Ischaemia as a result of peripheral vascular disease (chronic limb ischaemia)