Authors
- Dr. Armando Faigl
- Areej zeeshan Ahmed
Overview
Liver cysts are fluid filled cavities in the liver that are asymptomatic and usually found incidentally on abdominal imaging. Larger cysts are more commonly associated with symptoms and complications.
Differential diagnosis for all liver cysts
- Liver abscess
- Benign tumors
- Malignant tumors
- Regenerative nodules
- Cholelithiasis
- GERD
- Peptic ulcer disease,
- Gastric dysmotility
- Hemangioma, and/or hamartoma.
Classification
- Simple cysts
- Hydatid cysts
- Congenital polycystic liver
- Biloma
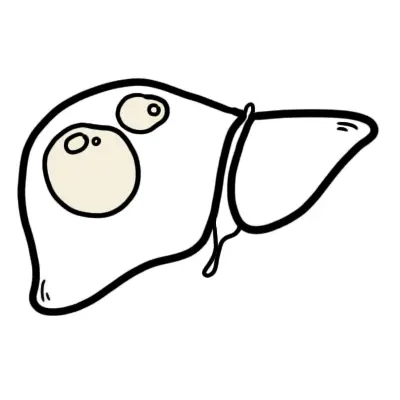
Simple cysts
Are congenital in origin
Risk factors
- Age more than 50 years
- More common in females
Signs and symptoms
Small cysts are asymptomatic but larger ones may present with dull abdominal pain in the right upper quadrant, anorexia and bloating.
| Side note Significantly large cysts may even be palpable on abdominal examination |
Investigations
An ultrasound is performed which shows an anechoic round lesion whilst CT shows a well demarcated lesion.
Management
If symptoms are present laparoscopic surgery is done.
Complications
Larger cysts can
- Compress the biliary tree
- Rupture and cause infection
Hydatid cysts
Fluid filled cavities caused by tapeworm infection of echinococcus genus that are transmitted via faecal contaminated food, water or soil. Most commonly seen in farming or rural communities.
| Remember They can even be transferred from the fur of dogs, cats, foxes! |
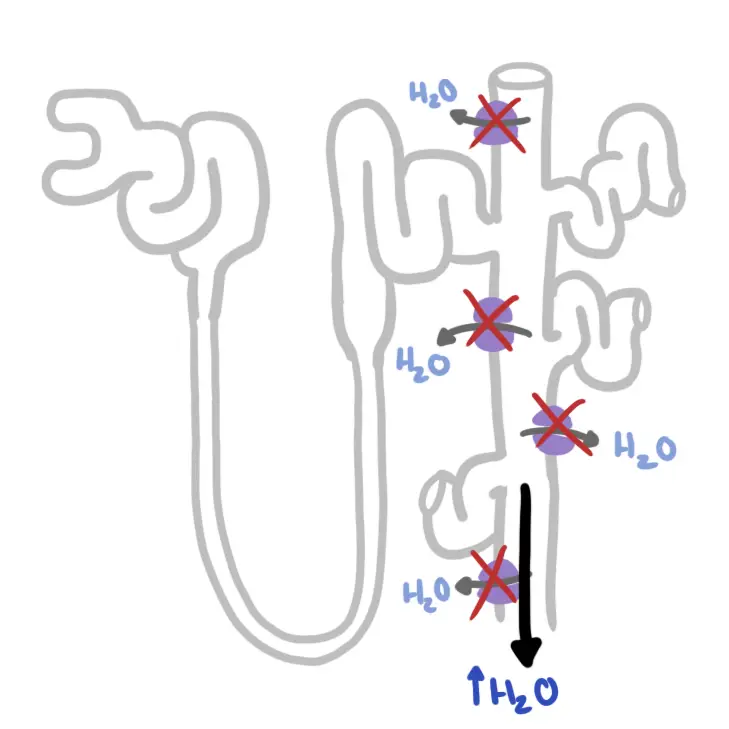
The eggs travel to body organs through the bloodstream after penetrating the intestinal wall -> Cyst formation
Two main types
Cystic echinococcosis
- Infection by E. granulosus
- Usually present as a single liver cyst
- Usually present as a single liver cyst
- Signs and symptoms
- Echinococcal cysts can be asymptomatic or cause increased temperature ,bloody sputum, and pruritus.
- On GPE hepatomegaly and right upper quadrant tenderness is recorded. Patients also complain of non-specific symptoms such as malaise ,nausea and vomiting.
| Remember Hydatid cysts are known to rupture an cause anaphylactic shock which can be fatal! |
- Investigations
- Ultrasound shows anechoic, smooth, well demarcated cyst. When present with daughter cysts, ultrasound can detect characteristic internal septations.
- Eggshell calcifications may be seen in cyst walls.
- CT scan
- Echinococcus ELISA (serology)
- Eosinophilia, low wbcs and low platelets
- Ultrasound shows anechoic, smooth, well demarcated cyst. When present with daughter cysts, ultrasound can detect characteristic internal septations.
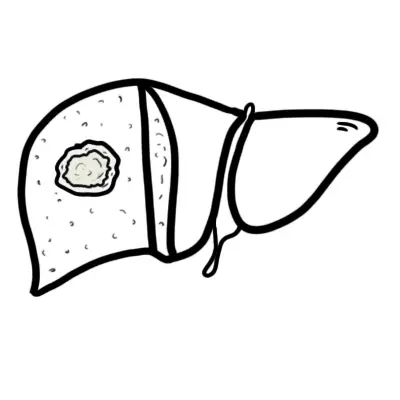
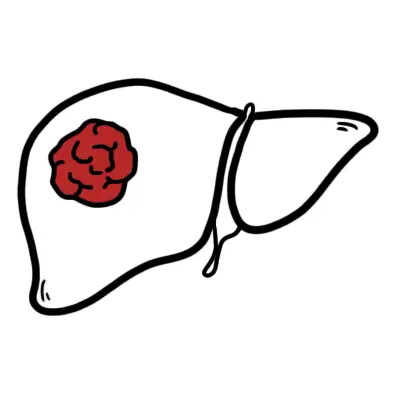
Alveolar echinococcosis
- Infection by E. multilocularis that behaves like hepatocellular carcinoma destroying surrounding structures.
- Signs and symptoms
- Hepatic cyst causing hepatomegaly and right upper quadrant pain as well as the non specific symptoms.
- Cyst invades and destroys liver parenchyma causing
- Portal hypertension
- Liver cirrhosis
- Cholangitis
- Jaundice
- Budd-chiari syndrome
| Remember E. multilocularis has potential of malignancy thus higher mortality than E. granulosus |
- Investigations
- Ultrasound Liver - Irregular lesions with poor margins with central necrosis as well as cyst wall calcifications
- CT scan
- Echinococcus ELISA (serology)
- Eosinophilia, low wbcs and low platelets
Management
Asymptomatic simple hepatics cysts do not require any treatment but cysts larger than 4cm are monitored.
Cysts less than 5 cm are treated with antihelminthic agents such as albendazole or mebendazole.
The three operations performed that remove the cyst or reduce its size are
- Percutaneous aspiration
- Done in combination with albendazole
- Cysts more than 5cm
- Laparoscopic deroofing
- If aspiration not successful or viable
- Much lower recurrence rate for this method
- Downside of higher morbidity.
- Complete cyst excision
- Cysts more than 10cm
- To avoid any spillage of contents
| Remember hydatid cysts cause fatal anaphylactic reactions on rupture! |
Prognosis
- 90% of untreated Alveolar echinococcosis patients die within 10 years, while treated have a far better prognosis.
- Prognosis of Cystic echinococcosis depends on other organ involvement.
Congenital polycystic liver
These cysts are extrarenal manifestations of polycystic renal disease.
It is an inherited disorder caused by a defect in
- PKD1 or PKD2 gene leading to dominant type which manifests in adulthood
- PKHD1 leading to recessive type which manifests in infancy
| Side note Cysts are more common in dominant type |
Risk factors for progression to liver
- Genetics
- Age older than 35
- Female sex
| Side note Cysts volume is larger in women than men |
- Contraceptive drugs
- Multiple pregnancies
| Side note Hepatic cysts epithelial lining is very reactive to estrogen induced growth as they express receptors for it |
Signs and symptoms
Like many other cysts classifications, polycystic liver cysts are usually asymptomatic and incidental findings that begin to show symptoms once enlarged.
Big cysts can compress intrahepatic structures along with hepatomegaly inducing
- Shortness of breath
- Esophageal reflux
- Postprandial fullness
- Back pain
- Increased abdominal girth
- Budd-Chiari-like syndrome
Compression of Portal vein can lead to portal hypertension
- Varices
- Ascites
- Jaundice
- Encephalopathy
Investigations
- Diagnosis is made with imaging studies.
- Ultrasound is performed which shows hyperechoic areas in the subscapular regions of the liver while on CT they appear hypodense and well delimited.
- Liver function is typically normal.
Management
Three main types of interventions are made for symptomatic patients
- Medical therapy
- Octreotide
- Estrogen receptor antagonists
- Surgical
- Laparoscopy- the cyst is deroofed and aspirated
- Segmental hepatic resection
- Only for patients with extreme hepatomegaly and symptoms
- Liver transplant
- Gives patients a good prognosis
Prognosis and complications
Invasive procedures carry their risk of complications as venous bleeding, bile leaks and sometimes adhesions thus need to carefully be weighed with benefits for a good prognosis.
Other complications
- Cyst haemorrhage
- Cyst infection
- Cyst rupture
- Portal hypertension
- Jaundice
Biloma
A biloma is defined as an abnormal, well-circumscribed, extra-biliary collection of bile that typically forms following traumatic or iatrogenic procedures of the biliary tree causing bile leakage and subsequent encapsulation and biloma formation.
Encapsulation of the bile leak is thought to be mediate through inflammation in the surrounding abdominal tissues or liver parenchyma, resulting in fibrosis and encapsulation.
Risk factors
Bilomas are most commonly secondary to disruption of the biliary tree by either an iatrogenic or traumatic cause.
- laparoscopic cholecystectomy
- endoscopic retrograde cholangiopancreatography (ERCP)
- radiofrequency ablation (RFA)
- transcatheter arterial chemoembolization (TACE)
- liver transplant
- Resection
- Biopsy.
Signs and symptoms
- Upper abdominal fullness and right upper quadrant discomfort following iatrogenic or traumatic disruption to the biliary tree.
- Nausea, vomiting, and fever are recognized symptoms
- If infected biloma - septic
Investigations
- Neutrophilia, raised CRP
- LFT may be deranged in compressed biliary tree
- If febrile - Blood cultures (mostly gram negative organisms grown)
- Imaging for diagnosis
- US
- CT
- MR imaging
- HIDA
Management
- Percuteanous drainage of biloma
- Ongoing bile leaks may require surgical fixation or endoscopic stent placement.
Complication
- If bile leakage rapid and large - Biliary peritonitis
- If biloma is infected - systemic inflammatory response, sepsis, and abscess formation.
- Cholestasis from obstruction of biliary tree
- Rare: pancreatitis, respiratory failure, and trans-diaphragmatic bile fistulation in patients with abdominal bile collections
References
- AMBOSS
- BMJ
- NCBI