Overview
Overview Transient ischemic attack is defined as transient neurologic symptoms without evidence of acute infarction. It is a common and important risk factor for future stroke. TIAs are produced by temporary ischemia to a vascular territory, usually caused by thrombosis or embolism and less commonly by vasculitis, hematologic disorders such as sickle cell disease or vasospasm.
| Remember The stroke risk after a TIA is around 10% at 2 weeks, with half of these events occurring within 48 hours. This emphasises the need for rapid clinical assessment and investigations in patients with TIA. |
| Defintion Stroke: Acute onset of a focal neurologic deficit due to a cerebral infarction or hemorrhage. Transient Ischaemic Attack (TIA): TIA is a transient episode of neurological dysfunction caused by focal brain or retinal ischaemia, without infarction. When there is evidence of brain infarction, the episode is considered to be a mild stroke (if symptoms are minor or disappear). Amaurosis Fugax: Transient monocular blindness that often is described as a gray shade being pulled down over the eye caused by ischemia to the retinal artery. |
Anatomy and Physiology
Cerebral Anatomy and Blood supply
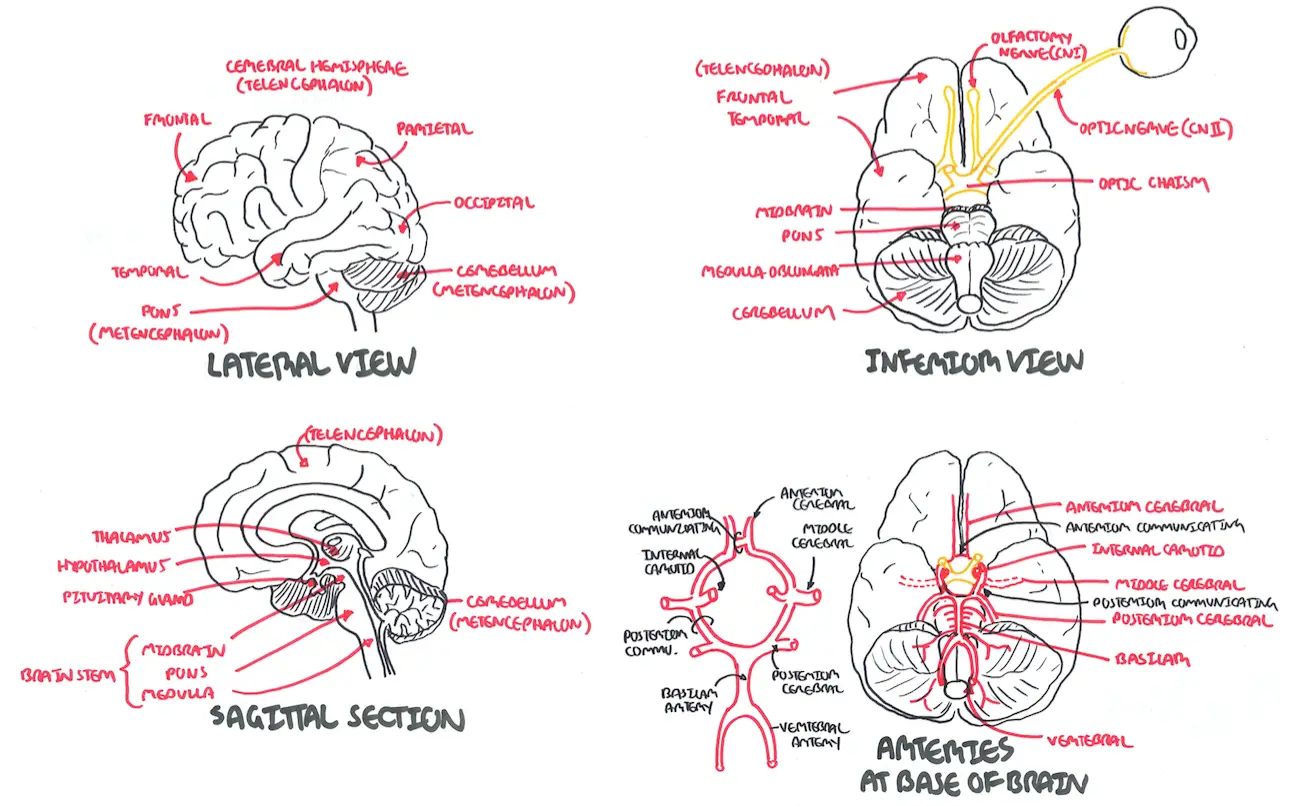
| Watch Anatomy - Cerebral anatomy and blood supply (Circle of Willis) |
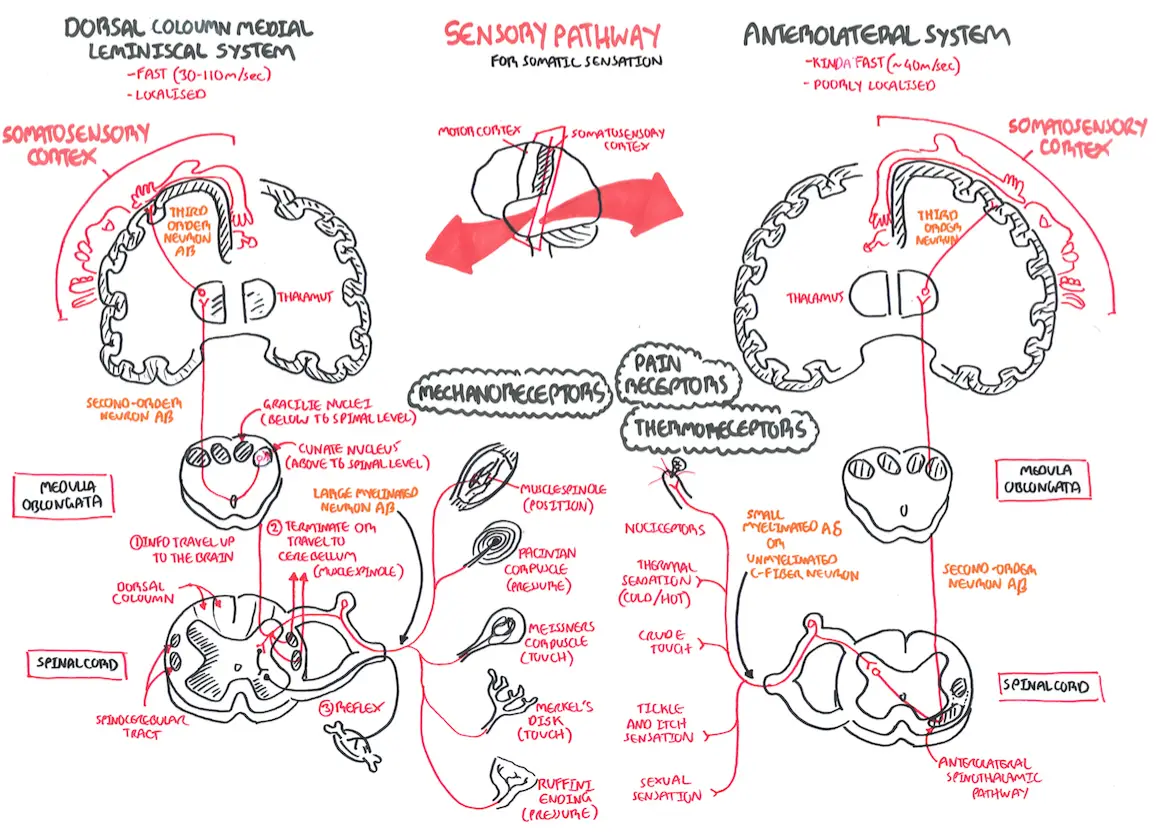
Sensory Pathways
Motor Pathways
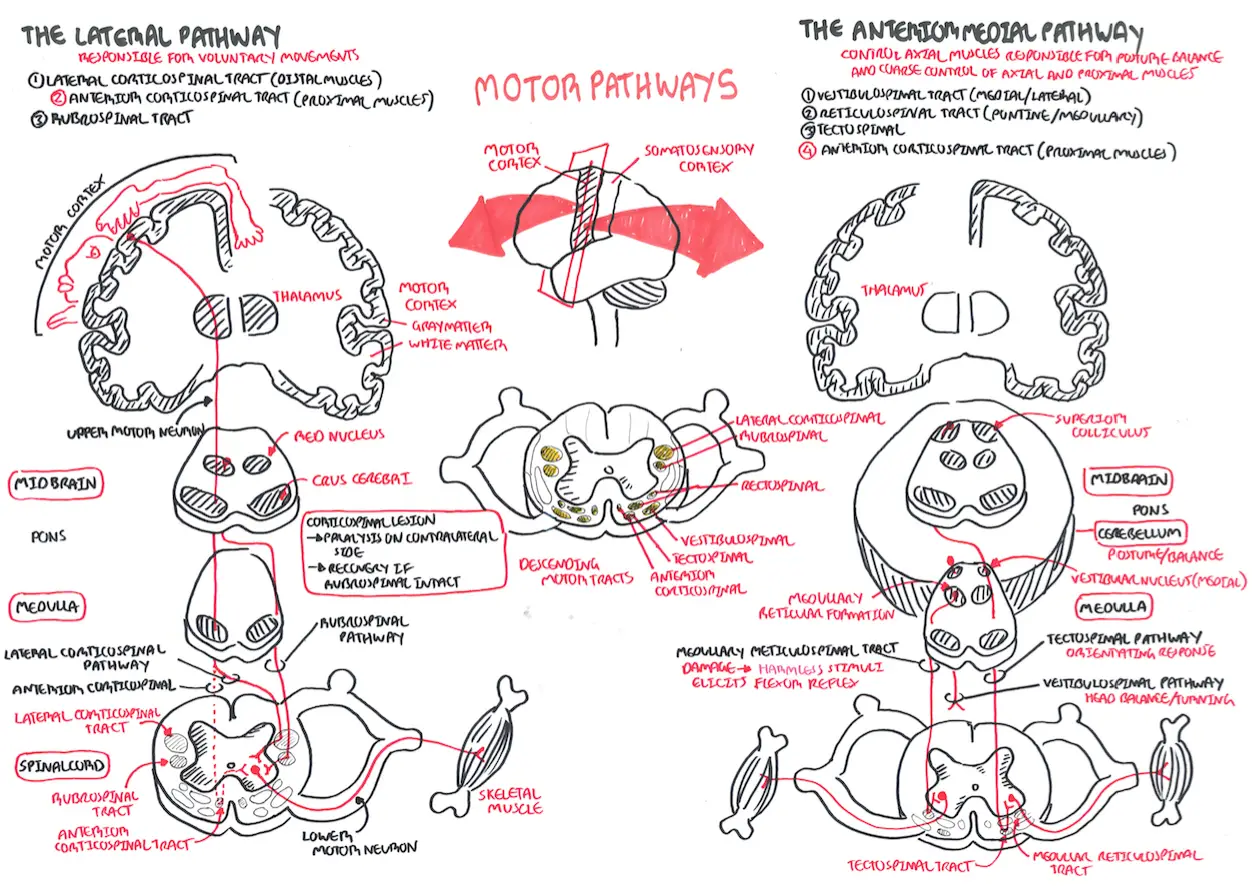
| Watch Motor Pathway |
Risk Factors
- Hypertension
- Smoker
- Large waist-to-hip ratio
- High alcohol intake
- Diabetes mellitus
- Unhealthy diet
- Psychosocial stress
- Regular physical activity
| Remember The highest- risk patients for stroke are those with previous ischemic events such as TIA |
Signs and Symptoms
The focal neurologic symptoms produced by ischemia depend on the area of the cerebral circulation involved
Common Presentation (Sudden onset)
- Memory loss
- Headache
- Blurred vission
- Unilateral paresis
- Transient monoocular blindness
- Diplopia
Cranial Nerve Examination
- Diplopia
- Hemianopia
- Monocular blindness
- Disconjugate gaze
- Facial drooping
- Lateral tongue movement
- Dysphagia
- Vestibular dysfunction
Cerebellar Examination
- Nystagmus
- Past-pointing
- Dystaxia
- Ataxia
| Side note Many patients with suspected TIA turn out to have a different diagnosis (eg migraine, hypoglycaemia, seizure). |
| Remember The ABCD (Age, Blood pressure, Clinical presentation, Diabetes mellitus, Duration of symptoms) score should be determined during the initial evaluation and can help assess the immediate risk of repeat ischemia and stroke. |
Differential Diagnosis
| CONDITION | CLINICAL MANIFESTATION |
| Brain tumor | Severe unilateral headache with nausea and vomiting |
| Central nervous system infection (e.g., meningitis, encephalitis) | Fever, headache, confusion, neck stiffness, nausea, vomiting, photophobia, change in mental status |
| Falls/trauma | Headache, confusion, bruising |
| Hypoglycemia | Confusion, weakness, diaphoresis |
| Migraines | Severe headaches with or without photophobia, younger age |
| Multiple sclerosis | Diplopia, limb weakness, paresthesia, urinary retention, optic neuritis |
| Seizure | Confusion with or without loss of consciousness, urinary incontinence, tongue biting, tonic-clonic movements |
| Subarachnoid hemorrhage | Severe headache with sudden onset and photophobia |
| Vertigo (central or peripheral) | Generalized dizziness and diaphoresis with or without hearing loss |
| Remember TIA is more likely with sudden onset, unilateral paresis, speech disturbance, or transient monocular blindness. |
Investigations
TIA and Stroke is a medical emergency!
Imaging
- CT or MRI
- ECG
- Carotid imaging within 24 hours
| Remember Urgent brain imaging is required. Computerised tomography (CT) can help to exclude a stroke mimic and to differentiate haemorrhagic to ichaemic stroke |
Laboratory investigation
- FBC
- EUC
- Blood glucose
- LFT
- Lipid studies
- Cardiac markers?
Other (for differentials)
- Rapid plasma reagin testing
- Cerebrospinal fluid analysis
- Urine drug screening
- Coagulation profile
| Remember All patients with suspected TIA should get FBC, EUC erythrocyte sedimentation rate (ESR), lipid profile, glucose level, ECG and brain (CT/MRI) and carotid imaging. |
Pathophysiology
NOT UP YET
Management
| INDICATION FOR CT/MRI |
| Patient on anticoagulants or with abnormal coagulation |
| Plan to give thrombolysis or immediate anticoagulants |
| Deteriorating conscious level or rapidly progressing deficits |
| Suspected cerebellar haematoma, to exclude hydrocephalus |
Medical Management
- Urgent brain CT or MRI (within 24hours)
- Antiplatelet - Aspirin (within 24-48 hours) if CT/MRI scans excludes haemorrhage
- The first dose should be at least 150 to 300 mg
- Dosage thereafter can be reduced (e.g. 100 mg daily)
- Long-term antiplatelet therapy: aspirin +/- dipyridamole or clopidogrel should be prescribed to all people with ischaemic stroke or TIA
| Remember Anticogulant is preferred for cardioembolic events (Ischaemic heart disease) if CT/MRI scans excludes haemorrhage |
Aggressive risk factor modification Interventions following a stroke or TIA are aimed at preventing future episodes
- Treat hypertension
- Smoking cessation
- Lose weight if obese
- Increase physical activity
- Treat Diabetes mellitus
- Treat dyslipidaemia with statin
- Hormone Replacement Therapy should be stopped
- Carotid endarterectomy or stenting
| Side note In patients found to have a high-grade ipsilateral carotid stenosis, carotid endarterectomy should be performed urgently. The benefit of surgery is greatest within 2 weeks of the TIA or mild stroke as this is the period of greatest risk of recurrent stroke. |
Dont Forget Primary Survey when someone presents to ED
Airway
- Is the patient able to protect his/her airway?
- Can the patient swallow without evidence of aspiration?
- Perform a swallow screen and keep patient nil by mouth if swallowing unsafe
Breathing
- Is the patient breathing adequately?
- Check oxygen saturation and give supplementary oxygen if oxygen saturation < 95%
Circulation
- Are peripheral perfusion, pulse and blood pressure adequate?
- Treat with fluid replacement, anti-arrhythmics and inotropic drugs as appropriate
Hydration
- Is the patient dehydrated or unable to swallow?
- Give fluids parenterally or by nasogastric tube if swallow is unsafe
Nutrition
- Assess nutritional status
- Consider nutritional supplements
- If dysphagia persists for a day or two, start feeding via a nasogastric tube
Medication
- If the patient is dysphagic, consider alternative routes for essential medications
Blood pressure
- Unless there is heart failure or renal failure, evidence of hypertensive encephalopathy or aortic dissection, do not lower the blood pressure in the first week since it will often return towards the patient's normal level within the first few days
- Early blood pressure reduction may decrease cerebral perfusion and increase infarction to offset potential benefits. Trials of early blood pressure lowering are ongoing
Blood glucose
- Is the blood glucose ≥11.1 mmol/l
- Hyperglycaemia may increase infarct volume, therefore use insulin (via infusion or glucose/potassium/insulin (GKI)) to normalise levels but monitor closely to avoid hypoglycaemia
Temperature
- Is the patient febrile?
- Raised brain temperature may increase infarct volume
- Investigate and treat any cause but give antipyretics early
Pressure areas
- These should be formally assessed and measures taken to reduce the risk
- Treat infection, maintain nutrition, provide a pressure-relieving mattress and turn immobile patients regularly
Incontinence
- Ensure the patient is not constipated or in urinary retention
- Avoid urinary catheterisation unless the patient is in acute urinary retention or incontinence is threatening pressure areas
Complication and Prognosis
Complications
- Stroke
- Myocardial infarction
- Depression
- Anxiety
- Unable to drive
Prognosis By definition, a patient with a TIA has no residual symptoms from the primary event.The highest- risk patients for stroke are those with previous ischemic events such as TIA, >10% of TIA patients seen in the emergency department will have a stroke within 3 months