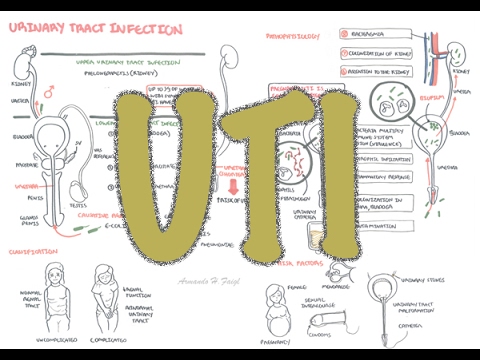
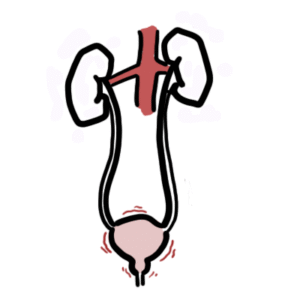
0:00 Hello, in this video we're going to talk about chronic kidney failure. 0:09 It can also be referred to as chronic kidney disease, but failure I guess is 0:13 the end stage. 0:15 And chronic kidney failure is essentially where you have loss, an irreversible 0:19 loss of the 0:20 nephrons, and the nephrons are the functional units of your kidneys, and this 0:24 can result 0:25 in a state, a toxic state, such as uremia, and we'll learn about that in this 0:31 video. 0:31 So here, before we go into chronic kidney failure, let's just recap the anatomy 0:36 slightly. 0:37 So here I'm going to the kidneys, the kidneys connects to the ureter, to the 0:42 bladder, bladder 0:42 stores urine, ready for micturition. 0:47 And here we have the inferior venocovin, the descending aurota, which has 0:50 vessels coming 0:51 in and out from the kidneys. 0:53 Okay, so there are many causes of chronic kidney failure, and these include 0:59 acute kidney 1:00 injury or acute kidney failure, hypertension, diabetes, and other kidney 1:06 diseases. 1:07 Other kidney diseases includes polycystic kidney disease. 1:12 So all of this can lead to an irreversible loss of nephron, which is chronic 1:19 kidney failure 1:20 or disease. 1:22 So let us look at each of these causes of chronic kidney failure in a bit more 1:28 detail. 1:28 Let's begin by looking at acute kidney failure or acute renal failure, it's the 1:34 same thing. 1:35 So acute kidney failure can lead to, you know, chronic kidney failure. 1:40 Acute kidney failure, unlike chronic kidney failure, is reversible. 1:45 And there are many causes of acute renal failure in itself. 1:49 One way to categorize it is into prerenal causes, intrarenal causes and postren 1:57 al causes. 1:58 So a prerenal cause includes renal artery stenosis, heart failure, and hemorrh 2:05 age, all 2:06 which leads to acute kidney failure. 2:10 And then you have intrarenal causes such as glomerular nephritis, tubular nec 2:14 rosis, and 2:15 interstitial nephritis. 2:17 All this can also lead to acute kidney failure. 2:20 Then you have postrenal causes such as benign prosthetic hyperplasia, renal 2:26 stones, and tumours. 2:28 It is also important to note that prerenal causes and postrenal causes often 2:34 lead to 2:35 intrarenal causes essentially. 2:38 And this will all lead to acute kidney failure, acute renal failure. 2:46 So that was, you know, acute renal failure and some causes. 2:51 Again acute renal failure can lead to chronic kidney failure. 2:55 Next, let us talk about hypertension and how this can cause chronic kidney 3:01 failure. 3:01 In order to do so, let us draw this kidney here, which has a renal artery and a 3:06 renal 3:07 vein leaving the kidney. 3:09 The functional unit of the kidney, which actually filters, you know, our blood 3:15 to form 3:15 your own, are the nephrons. 3:17 And here I am drawing one nephron. 3:20 The head of the nephron is the Bowman's capsule and it has capillaries entering 3:24 and exiting. 3:26 This is where blood, you know, is getting filtered through to the nephron. 3:32 Now when there's normal blood pressure, everything is smooth and everything is 3:37 filtered. 3:38 So let us see what happens in hypertension. 3:41 Let us zoom into this area here, the head of the nephron. 3:45 And, you know, this is the Bowman's capsule area. 3:49 So blood vessels will enter this area. 3:52 These blood vessels originate, you know, from the renal artery. 3:57 So here I am drawing part of the renal artery, which enters the kidney. 4:02 When someone has hypertension, it causes thickening of the blood vessels, which 4:08 leads 4:08 to narrowing of the lumen. 4:11 Once we have narrowing of the lumen, there is less blood flow to the kidneys, 4:15 to the nephrons. 4:18 The afferent arterial is a blood vessel which brings blood towards the head of 4:24 the nephron. 4:25 But with less blood flowing through, due to hypertension, there is a decrease 4:30 in filtration, 4:31 thus a decrease in the glomerular filtration rate. 4:36 So the point is, when you have a decrease in blood flow to the nephron, there 4:41 are cells 4:42 in this area that detect this and then start producing renin, which 4:48 subsequently leads 4:48 to the activation of the renin angiotensin-aldosterone system, or RAS, for 4:55 short. 4:56 Now the RAS system is a system which leads to increase in heart rate and 5:03 further hypertension. 5:06 This is unfortunate, because less blood is flowing to the kidneys. 5:12 The kidney thinks by increasing blood pressure it will receive more blood. 5:17 It might work for some time, but eventually this cycle will continue. 5:21 There is further vessel thickening and vessel narrowing. 5:26 So it's a vicious cycle. 5:28 Now this all eventually will lead to glomerular sclerosis, which is thickening 5:32 and hardening 5:33 of the vessels in the Bowman's capsule in the glomerulus itself. 5:40 Glomerular sclerosis inevitably leads to ischemic injury and so loss of the ne 5:45 phron itself. 5:48 Next let us look at the most common cause of chronic kidney failure, which is 5:53 diabetes. 5:54 A massive complication in diabetes is diabetic nephropathy. 5:58 Now diabetic nephropathy eventually will lead to chronic kidney failure. 6:03 To learn about diabetic nephropathy, let us cut a section of the Bowman's 6:07 capsule and 6:08 the glomerulus and see what changes occur. 6:13 The four main changes we see in diabetic nephropathy are mesangial expansion 6:19 and proliferation. 6:21 We see podocytopathy, which includes podocytopathy and eventually atrophy. 6:28 We see glomerular basement membrane thickening and sclerosis. 6:35 And sclerosis is essentially what we see in hypertension as well. 6:40 So how do all these changes occur? 6:43 Well, people develop diabetes because of risk factors, which include 6:51 hypertension. 6:53 Diabetes is a condition where you have high blood glucose. 6:56 High blood glucose leads to overproduction of reactive oxygen species. 7:02 Now these reactive oxygen species, or ROS, leads to a cascade of events. 7:08 But in summary, this will lead to activation and production of unnecessary 7:14 growth factors, 7:15 pro-inflammatory cytokines, and producing essentially oxidative stress. 7:22 All this leads to the four diabetic nephropathy changes we just talked about. 7:32 So going back to where we initially started, chronic kidney failure, again, is 7:37 where you 7:37 have irreversible loss of nephrons. 7:40 And this can be caused, as we have learned, by acute renal failure or acute 7:47 kidney failure, 7:48 hypertension, diabetes, and other kidney diseases, such as polycystic kidney 7:54 disease. 7:55 So when you have loss of nephrons in the area, the blood flow will shift to ne 8:02 phrons that 8:03 are still alive and working. 8:06 This leads to glomerular hyperfiltration. 8:11 So let me draw it out. 8:13 For example, here is a loss of nephron, and here is a functional nephron. 8:20 The blood flow will shift to the functional nephron, leading to glomerular 8:24 hyperfiltration. 8:25 There will be more blood flow. 8:28 Now during the early stages, glomerular hyperfiltration is tolerated. 8:34 We get a big increase in GFR in the functional nephron. 8:40 After a while, this hyperfiltration results in sclerosis because there's so 8:46 much pressure. 8:47 And eventually, glomerular sclerosis will eventually lead to loss of that neph 8:53 ron as 8:53 well. 8:54 And the cycle will continue. 9:01 In the late stage, you lose so much of your kidney's function that your GFR 9:10 decreases, 9:11 your urine output decreases, and you begin to retain waste resulting in euremia 9:19 . 9:20 All this leads to the clinical manifestations of chronic kidney failure. 9:25 And this will bring us to the next topic, which is the clinical presentation, 9:29 or clinical 9:30 manifestation of chronic kidney failure. 9:34 So here, in this part, we will talk about disruption that occurs with sodium 9:42 and water 9:43 balance, disruption that occurs with potassium balance. 9:47 We talk about metabolic acidosis, mineral balance, and osteodystrophy, and 9:51 other manifestations 9:53 of euremia. 9:55 So let's begin by looking at sodium and water balance. 9:59 A decrease in GFR leads to increase in sodium and water retention, which leads 10:05 to an increase 10:06 in blood pressure and peripheral edema. 10:09 It is important to restrict fluid intake for these patients. 10:17 And when vomiting and diarrhea occurs in patients with chronic kidney failure, 10:23 this is very 10:24 dangerous, because of the already restricted fluid intake, further loss from 10:29 vomiting 10:29 and diarrhea can be very, very dangerous. 10:35 Next, potassium balance. 10:36 So again, a decrease in GFR leads to an increase in potassium retention. 10:43 This causes hyperkalemia, which can result in muscle weakness. 10:47 It can result in ECG changes and cause fibrillations. 10:53 It is important to note that the loss of nephrons leads to a decrease in rinden 10:58 production as 10:59 well, eventually, which leads to a decrease in aldosterone. 11:03 When you have a decrease in aldosterone, the distal sodium-potassium pump does 11:07 not work, 11:09 which leads to potassium retention. 11:12 Therefore, using potassium-sparing diuretics and ACE inhibitors can further 11:19 aggravate a 11:20 problem because you are, essentially, promoting more potassium. 11:26 And remember, if I draw it in this nephron, the sodium-potassium pump, the 11:30 sodium-potassium 11:32 ATPase is at the distal part of the nephron and is responsible for the exchange 11:37 between 11:37 sodium and potassium. 11:40 So if aldosterone is not being produced, this transporter does not work, and so 11:49 we are 11:49 retaining potassium. 11:54 Metabolic acidosis. 11:55 Now, metabolic acidosis, we get diminished capacity in chronic kidney failure 12:00 to excrete 12:01 hydrogen and to generate bicarbonate, which leads to the acidosis. 12:06 Acidosis can lead to bone decalcification amongst many other things. 12:11 So normally, the nephron is responsible for maintaining the pH of our body, the 12:17 blood. 12:18 It does this by producing bicarbonate, if necessary, or to secrete hydrogen 12:25 ions, if 12:26 necessary. 12:28 Next let's talk about mineral and osteodystrophy. 12:31 Now when you have loss of nephrons, the kidneys cannot produce the hormone it 12:37 normally produces, 12:37 which is calcitrile. 12:40 Now with no calcitrile, you have a decrease in calcium reabsorption from the G 12:46 IT and the 12:47 kidneys. 12:49 And this will lead to hypocalcemia. 12:53 Hypocalcemia and a decrease in calcitrile will stimulate the parathyroid glands 13:00 always 13:01 continuously, and this will lead to secondary hyperparathyroidism. 13:06 The hyperparathyroidism state leads to osteodystrophy because of the hormone 13:12 parathyroid hormone, 13:14 which actually stimulates bone breakdown and, yeah, bone breakdown essentially. 13:21 The loss of nephrons eventually also lead to a decrease in GFR. 13:26 And so, you know, when you have a decrease in GFR, you have a decrease in filt 13:31 ration. 13:31 And so this will lead to hyperphosphatemia because the body cannot secrete 13:36 phosphate. 13:37 Yeah. 13:38 Now let's talk about uremia, which is essentially a lot of urea in the blood. 13:44 Urea is normally excreted by the kidneys in urine. 13:49 Let's see what normally happens to urea. 13:53 So the vasorecta, the blood vessels responsible for secretion of substances 14:01 into the nephron, 14:03 and the reabsorption of substances from the nephron. 14:07 In the last part of the nephron, the urea is actually reabsorbed into the vas 14:12 orecta, which 14:13 helps drag water into these vessels. 14:16 Urea then gets secreted back into the nephron because we don't want to keep it. 14:21 And the water just remains. 14:23 Water remains in the vessels because here the sodium is also reabsorbed, 14:29 allowing for, 14:31 you know, equilibrium. 14:34 And so if this whole process does not work, if the kidneys don't work at all, 14:39 you actually 14:39 retain urea and so you get urea. 14:44 And urea is bad because it results in urological signs and symptoms such as h 14:49 iccups, cramps, 14:50 gastro problems, anorexia and vomiting, reproductive changes, including 14:54 decrease in 14:55 estrogen and testosterone, resulting in amenorrhea and impotence. 15:00 And this urea may also result in some skin changes. 15:04 And so that was most of the clinical manifestations in chronic kidney failure. 15:10 Finally, as we have mentioned briefly, in late chronic kidney failure or 15:14 chronic kidney 15:15 disease, when a lot of nephrons are lost, this will eventually result in a 15:19 decrease in 15:20 renin production, resulting in a decrease in blood pressure, a decrease in ery 15:25 thropoietin, 15:26 which results in anemia, and also, as I mentioned earlier, a decrease in the 15:31 production of the 15:32 hormone calcitrile, which causes renal osteodystrophy, as I mentioned earlier. 15:39 So I hope you enjoyed this video. 15:41 We essentially talked about chronic kidney failure, some of the causes, and 15:45 some of the 15:46 clinical manifestations that results. 15:49 Thank you for watching.