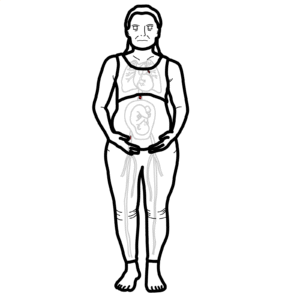
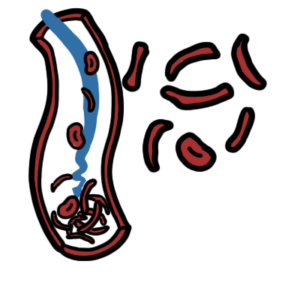
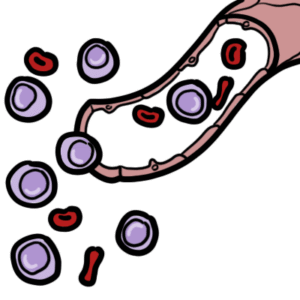
0:00 In this video we're going to talk about deep vein thrombosis, or DVT for short, 0:09 which is 0:09 a big issue, especially amongst patients post-op undergoing surgery, patients 0:15 who are immobile, 0:17 chronic illness, and bed bound. 0:19 DVT can lead to a common complication known called pulmonary embolism, which is 0:26 life-threatening. 0:29 The signs and symptoms of DVT include asymmetrical edema, asymmetrical cough 0:34 swelling, and asymmetrical 0:36 localized pain in the cough. 0:38 There can be signs and symptoms of pulmonary embolism as well, which is again a 0:41 common 0:42 complication of DVT. 0:45 During a normal leg, on the left here we have a leg with DVT. 0:50 The leg with DVT on the left is swollen, has edema with erythema and is warm. 0:57 So deep vein thrombosis, as the name implies, means thrombus forming within the 1:03 deep veins. 1:04 So let's look at a normal vein of the legs here. 1:06 A normal vein of the legs have valves, which assist in the hemodynamics of the 1:11 veins and 1:12 helps return blood back to the heart by preventing back flow. 1:17 In deep vein thrombosis, there is thrombus occurring within these veins of the 1:22 leg, the 1:22 lower legs usually. 1:25 And so clotting is occurring. 1:27 A thrombus is made up of a network of fiber and mesh, platelets and red blood 1:32 cells. 1:32 They all clump together via coagulation cascade and forms what's known as a th 1:38 rombus. 1:38 There are many causes of deep vein thrombosis, or thrombus formation. 1:44 But it can all be condensed to three things. 1:47 And these three things or factors make up what we call virtuos triad. 1:53 And virtuos triad includes vessel injury, number one, venous stasis, number two 1:59 , and 2:00 hyperquagulability, number three. 2:04 Different diseases, condition leads to one or more of these factors, and this 2:10 will predispose 2:11 one to developing deep vein thrombosis. 2:15 And so once a thrombus has occurred, the thrombus itself has a few fates, 2:20 including propagation, 2:22 which means just growing along the vessel. 2:26 Organization, organizing within the vessel layer, re-canulization, forming 2:31 holes within 2:32 the thrombus. 2:35 Embolism, which means dislodgement of the thrombus, allowing the thrombus to 2:39 travel 2:40 around the body via the blood. 2:43 And/or resolution, the thrombus just gets broken down by plasmin, by factors 2:48 that we 2:49 have in our own body. 2:51 But we will mainly focus on embolism, because it is a common fate of thrombus 2:56 in the deep 2:57 veins and can be life-threatening. 3:00 When a thrombus dislodges and becomes an embolus, it can travel up to the heart 3:04 via 3:05 the inferior vena cava. 3:07 The heart will then pump the embolus to the pulmonary circulation. 3:12 The embolus can then lodge into the pulmonary arteries, causing what's known, 3:17 sorry, as 3:18 a pulmonary embolism, and this can subsequently cause pulmonary tissue in fact, 3:23 if it is big. 3:26 And so pulmonary embolism is a big complication of deep vein thrombosis. 3:31 Another big complication is actually the side effects of the medications people 3:36 take 3:36 who have deep vein thrombosis. 3:39 And these medications, they can cause acute GI bleeding because the medications 3:44 are anticoagulants. 3:47 The risk factors for developing deep vein thrombosis essentially will fall into 3:52 one or more of the 3:54 virtuos category, the virtuos triad category. 3:58 And these risk factors include pregnancy. 4:01 Now, pregnancy can cause or as a risk factor to do Vt because when the uterus 4:07 enlarges, 4:08 it can press against the inferior vena cava causing stasis below. 4:13 Also in pregnancy, there is a rise in clotting factors. 4:17 Other risk factors for developing deep vein thrombosis include increased age, 4:23 obesity, 4:24 malignancy, having had a major surgery for the past three months, having 4:29 medical comorbidities, 4:31 being hospitalized in the past two weeks. 4:35 And for patients who are hospitalized, 25 to 50% of actually surgical patients 4:42 can develop 4:42 DVT and also many non-surgical patients. 4:47 Other risk factors for DVT include being on certain medications such as oral 4:51 contraceptives, 4:53 tamoxifen, being on long-distance flights. 4:58 Genetics also plays a role in increasing the risk of DVT. 5:03 Genetics including anti-thrombin gene mutation, protein C and S deficiency, and 5:11 also anti-thrombin 5:12 deficiency. 5:16 Investigations for deep vein thrombosis include a full blood count, liver 5:20 function test, 5:21 electroideuria creatinine, INA, APTT, which are both clotting studies. 5:30 Imaging including venous duplex ultrasound. 5:33 And imaging can also include imaging for the chest in suspicion of pulmonary 5:39 embolism. 5:40 There's another investigation that can be done based on the coagulation cascade 5:45 . 5:45 Let us briefly go through the coagulation cascade. 5:49 There are two pathways in the clotting cascade or coagulation cascade, which is 5:54 the extrinsic 5:55 pathway and the intrinsic pathway. 5:58 Both the extrinsic pathway and the intrinsic pathway will lead to a common 6:03 pathway, which 6:04 is activation of factor 10 to factor 10A. 6:10 10A in turn activates factor 2 or prothrombin to factor 2A, which is known as 6:17 thrombin. 6:18 Thrombin then activates fibrinogen to fibrin. 6:22 Fibrin forms the basis of the fibrin mesh and is the last step in the formation 6:26 of the thrombus. 6:28 So now the thrombus is formed. 6:30 However, things can also break down the thrombus. 6:35 These things is plasminogen or plasmin and a plasmin cleaves the fibrin, 6:40 creating what 6:41 is now called a d-dimer. 6:45 During active thrombosis, there is elevated d-dimer. 6:49 And so the measurement of a d-dimer can give some indication of coagulation 6:54 activity that 6:55 is occurring in the body. 6:57 However, saying this, testing for d-dimer is not very specific for deep vein th 7:02 rombosis. 7:03 As elevated d-dimer also occur in a number of other conditions, including 7:10 pregnancy as 7:11 well as post-surgery. 7:13 And so measuring d-dimer is often not useful, but sometimes it is useful in 7:20 ruling out pulmonary 7:21 embolism or deep vein thrombosis. 7:25 Let's move on to management, which is mainly anticoagulants. 7:29 And essentially, the anticoagulants include heparin, and there are two types of 7:35 heparin 7:35 that can be given. 7:37 Low molecular weight heparin, which is given IV or subcutaneous unfraction he 7:44 parin. 7:45 Warfarin is given orally and needs maintenance through iron arm measurement. 7:51 Probably heparin and warfarin target some pathways within the cotton cascade, 7:56 mainly 7:57 the common pathway. 8:01 Another important management is actually prophylaxis, preventing PE from 8:07 occurring. 8:08 And this is especially important for patients who are undergoing surgery. 8:13 And these prophylaxis interventions include compression stockings, as well as 8:18 physical 8:18 activity for the people that sit down a lot to keep the blood flowing.