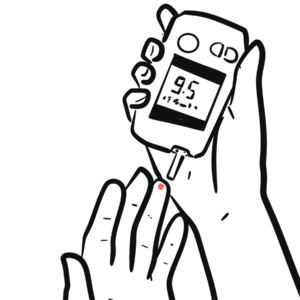
0:00 Hello, in this video, we're going to talk about diabetic ketoacidosis. 0:08 This is an introduction in an overview. 0:10 It is important to know that diabetic ketoacidosis is a medical emergency, 0:15 especially in type 0:17 1 diabetic patients, but it is known that it can also occur in type 2 diabetes. 0:24 As the name suggests, it has to do with acidity, so there's increase in acidity 0:28 in the blood 0:29 essentially. 0:31 The signs and symptoms of diabetic ketoacidosis is nausea, vomiting, polyurea, 0:38 polydipsia, 0:39 weight loss, hyperventilation known as kuzmals breathing. 0:44 Now, diabetic ketoacidosis doesn't occur out of the blue, there's usually some 0:50 triggers, 0:51 and these triggers, these etiologies, it can be remembered as the five eyes. 0:58 The five eyes are infection, intoxication, inappropriate withdrawal of insulin, 1:06 infuction, 1:07 and intercurrent illness. 1:14 And these five triggers, they cause what we know as diabetic ketoacidosis. 1:21 So let's go into the pathophysiology briefly. 1:25 If you want to know more about the functions of insulin, watch a video I have 1:31 on the Fed 1:32 state, which is under biochemistry. 1:34 Anyways, the pancreas normally produces insulin. 1:38 However, in diabetes type 1, there is an autoimmune attack on the B cells, 1:44 which normally 1:45 produce insulin, and therefore insulin is not being produced anymore, so we 1:50 have a decreased 1:52 in insulin. 1:54 Glycone is an important hormone. 1:56 And because we have a decrease in insulin, this causes some problems. 2:01 First, it means that gluconeogenesis is not inhibited. 2:08 And so we get gluconeogenesis, we get more production of glucose. 2:14 We also get increased glycogenolysis, and we get a decrease in glycolysis, all 2:21 of which 2:22 will result in more glucose in the blood. 2:24 So we get hyperglycemia. 2:29 Hyperglycemia results in glucose being peed out. 2:33 So we get glucose urea, glucose draws water, so we get polyuria, and we also 2:39 get dehydration 2:40 as a result. 2:42 Because we lose a lot of water and we are dehydrated, we get polydipsia, we get 2:48 thirsty. 2:50 It's also important to note that the decrease in insulin, the absence of 2:54 insulin, means 2:54 that fat breakdown occurs. 2:59 It's a very important concept to understand fat breakdown occurs, especially if 3:05 the body 3:05 is not receiving enough energy. 3:08 So in periods of infection or feeling ill, the body will start breaking down 3:15 the fat because 3:16 glucose is not present, and because glucose is not being taken up. 3:21 Fats get broken down from adipose tissue to form free fatty acids, which then 3:28 go to 3:28 the liver and undergo ketogenesis to make more ketone bodies. 3:34 It does this because the body needs some form of energy, some form of supply, 3:39 because glucose 3:40 is not working, or because glucose is not present. 3:45 With so much ketones being made, we get ketoneemia, we get high ketones in the 3:51 blood. 3:51 And then subsequently, this means that we get ketone urea, we are peeing out 3:57 ketones. 3:58 And it's also important to note that ketones are acidic, ketones are acids, and 4:06 so they 4:07 reduce the pH in the blood, but also they will reduce the pH in urine. 4:13 This is the main pathophys we see in DKA. 4:18 So if a person presents with the signs and symptoms we spoke of, a thorough 4:22 history and 4:23 examination needs to be done, and appropriate management needs to be performed, 4:29 which includes 4:30 checking the airways, checking breathing, and circulation. 4:36 In circulation, IV access is important for a few reasons, first, to get bloods 4:43 for investigation. 4:45 It's also important here to get a base serum potassium level. 4:52 After getting the bloods for investigation, administering IV fluids, saline, 4:58 and also administration 5:00 of insulin slowly is very important. 5:04 And if insulin is important because we want the cells in the body to take up 5:10 the glucose 5:11 that is in the blood. 5:14 While this is going on, investigations have to be performed. 5:19 So ABG, which is arterial blood gas, is very important to measure the pH in the 5:25 blood. 5:26 And this needs to be done regularly. 5:30 Once as we mentioned, full blood count, EUCs for infections and also electroly 5:36 te abnormalities 5:37 and dehydration, urine analysis is important to check and monitor if there's 5:44 glucose, ketones, 5:46 and infections. 5:48 ECG is performed to check for arrhythmias in case of potassium, hyperkalemia, 5:56 or hypokalemia. 5:58 So again, monitoring pH by doing regular arterial blood gas is important. 6:03 And also it is important to monitor serum potassium levels. 6:07 The reason it is important to measure serum potassium levels is insulin is 6:12 being administered. 6:14 Because insulin will actually cause hypokalemia. 6:19 If you get hypokalemia, you can actually trigger an arrhythmia. 6:25 Sometimes calcium gluconeate can be administered to protect the heart from 6:30 these hypokalemia-induced 6:32 arrhythmias. 6:34 Anyways, monitoring is continuous. 6:38 Check pH and check bloods. 6:42 After a while, you can switch the fluids to 0.5% saline and 5% dextrose. 6:49 This is done when blood glucose goes down at least about 14mm per liter, let's 6:55 just say. 6:57 Again, for diabetic ketoacidosis, monitoring is essential. 7:02 Monitor bloods, EUCs, perform ABGs to check for pH, and monitor urine output, 7:08 and also 7:09 the changes in urine pH, glucose, and ketones.