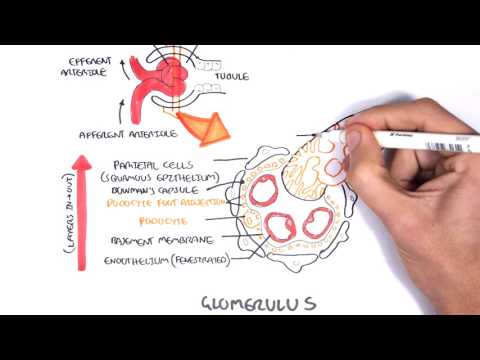
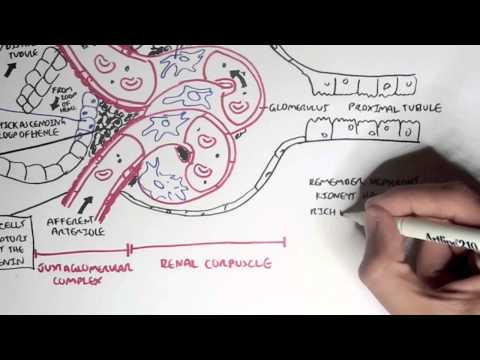
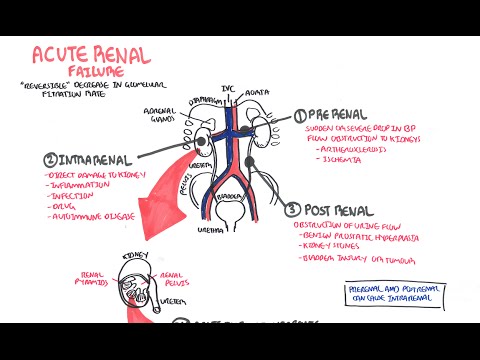
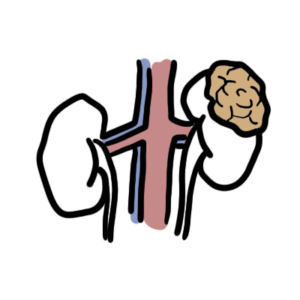
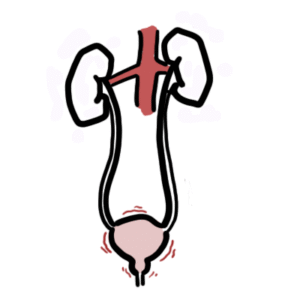
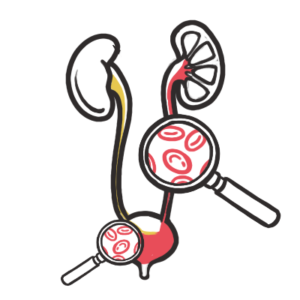
0:00 Hello, in this video we're going to talk about nephrotic syndrome and focused 0:08 on the pathophysiology. 0:11 So nephrotic syndrome presents as a tetrad of manifestations and this tetrad is 0:19 protein 0:19 urea, greater than 3.5 grams in 24 hours. This lipidemia, more specifically 0:27 hypercholesterolemia, 0:30 the third is hypo albuminemia and the last is peripheral edema or edema. So let 0:40 us look 0:41 at the pathophysiology and see how this tetrad occurs. So here is a nephron, 0:48 the functional 0:49 unit of the kidney. Here is the afferent arterial coming into the head of the 0:55 nephron and forms 0:56 the glomerulus within the head of the nephron. Coming out is the efferent arter 1:02 ial which 1:03 eventually joins with other efferent arterials to form the renal vein and then 1:09 the renal vein 1:10 will enter circulation once again. In nephrotic syndrome for many reasons which 1:18 won't be 1:19 discussed in detail here, there is inflammation and damage to the glomerulus. 1:26 This inflammation 1:27 and damage can be from immune cells, antibodies, component proteins, immune 1:33 complexes, hypertension 1:35 and sclerosis. Whatever the cause, it results in damage and inflammation 1:42 specifically to 1:43 cells called podocytes which normally help prevent protein loss. So podocytes 1:51 are damaged 1:52 within the glomerulus and this damage will allow proteins to pass through into 1:58 the nephron's 1:59 tubule and remember this usually should not happen. And so the protein travels 2:07 through 2:07 the nephron's tubule and will be part of urine and nephrotic syndrome is 2:12 characterized 2:14 by protein loss of more than 3.5 grams in 24 hours. This loss of protein 2:23 results in mass 2:24 protein urea with or without hematuria which is blood in urine and this hematur 2:32 ia will 2:33 essentially depend on how much damage occurs to the glomerulus. The protein 2:40 loss can also 2:41 be antibodies that is lost because antibodies are proteins as well. So if there 2:47 is loss 2:48 of antibodies, the person doesn't have their normal antibody defense mechanism 2:54 and so 2:54 this means that they are at increased risk of infection. The mass loss of 3:01 protein such 3:02 as albumin from the circulation results in hypoprotonemia, more specifically 3:12 hypo albuminemia. 3:14 So less protein, less albumin in the blood. And this will tell the liver to 3:22 produce more 3:24 proteins to compensate and so the liver works on overdrive producing not only 3:30 proteins such 3:32 as albumin but the liver will also produce cholesterol. The cholesterol is not 3:38 necessary 3:39 but because anyway resulting in hypercholesterolemia. Now the hypoprotonemia or 3:48 the hypo albuminemia 3:51 also results in a reduced plasma oncotic pressure. A reduced oncotic pressure 3:58 means that water 4:00 and the electrolytes will actually move into the interstitium so they will move 4:06 from circulation 4:07 into the interstitium. This occurs because of oncotic pressure. There are no 4:14 solutes. 4:15 There are no proteins in the vascular compartment to hold the water and the 4:20 electrolytes and 4:22 so the water and the electrolytes will move to the interstitium and this will 4:26 result in 4:27 peripheral edema which causes swelling of the feet for example. 4:34 Now the movement of water and electrolytes means that there will be a decrease 4:39 in volume 4:40 in the vascular compartment. There will be decrease of volume in the 4:45 circulation. This 4:47 decrease in volume means that there will be a decrease in volume returning to 4:51 the heart 4:52 so there will be a decrease in venous return to the heart. With a decrease in 4:57 blood volume 4:57 returning to the heart this means that the heart will also be pumping less 5:02 volume to 5:02 the rest of the body. What does this mean? Well, this means that there will be 5:09 a decrease 5:10 in renal blood flow which means a decrease in GFR. The GFR stands for the gl 5:18 omerular filtration 5:19 rate and it's essentially the rate at which the kidneys, the nephrons filter 5:25 circulation. 5:28 Now the inflammation that is occurring in the kidneys already will also 5:33 contribute to a 5:34 decrease in GFR. So when you have a decrease in GFR, when you have a decrease 5:41 in the glomerular 5:42 filtration rate and the blood flow, this will actually stimulate some cells 5:48 ahead of the 5:49 nephron to produce a molecule called renin. Renin is important and it will 5:57 activate what 5:58 is known as the renin angiotensin aldosterone system. The function of the renin 6:05 angiotensin 6:06 aldosterone system is to essentially increase blood pressure to compensate for 6:11 the decrease 6:12 in vascular volume and the decrease in GFR. One way the renin angiotensin ald 6:19 osterone 6:19 system does increase blood pressure is by retaining sodium and thus retaining 6:28 water 6:29 from the kidneys to maintain it in the vascular space. However, this will 6:37 eventually result 6:38 in further edema because of the hypoprotonemia that is already occurring, 6:47 remember. So in 6:49 summary, we just saw how proteinuria occurs due to inflammation in the glomer 6:55 ulus and 6:56 this will eventually lead to hypo albuminemia, hypercholesterolemia and 7:02 peripheral edema and 7:04 this is a tetrad seen in nephrotic syndrome. Based on this tetrad, we can 7:10 expect to possibly 7:12 see some signs and symptoms. So for the dyslipidemia, the hypercholesterolemia, 7:19 we can see xantholezma 7:22 which is deposits of cholesterol around the eye and xanthomata. Hypo albuminem 7:29 ia will result 7:30 in tiredness and leukonichia striata which is essentially the changes occurring 7:37 along 7:38 the nail bed. Hypo albuminemia also results in edema because of the reduced onc 7:46 otic pressure. 7:47 Edema can be periorbital edema which is fluid around the eye, it can be acites, 7:55 fluid in 7:56 the abdomen and also peripheral edema of the lower limb. Patients with nephrot 8:03 ic syndrome 8:03 can be breathless because of fluid edema, because of the fluid overload or ple 8:08 ural effusion. 8:11 Urine in nephrotic syndrome is often described as being frothy in appearance. 8:18 So next is 8:19 investigations. Now there are many many causes of nephrotic syndrome and these 8:24 causes will 8:25 be discussed on a separate video which will look at the different types of neph 8:29 rotic syndrome. 8:31 But some common causes of nephrotic syndrome include diabetic nephropathy, 8:36 there are certain 8:37 connective tissue diseases and some autoimmune immunological problems that 8:44 attack the kidneys. 8:45 So the investigations that are performed is to assess severity, is to diagnose 8:52 nephrotic 8:53 syndrome and to differentiate the different types of nephrotic syndrome. So 9:00 investigations 9:00 can include urine dipstick, MSU, full blood count, EUCs, liver function test, L 9:10 FTs, calcium 9:11 levels, CRP and glucose. Serum and urine immunoglobulins is important to screen 9:20 for autoimmune diseases 9:23 and also to check for presence of immune response to hepatitis B, hepatitis C 9:30 and HIV which 9:31 are also some causes of nephrotic syndrome. Chest x-rays can be performed and 9:38 may show 9:39 pleural effusion or edema. Other important investigations include ultrasound of 9:47 the kidneys. 9:49 Rinal biopsy is important to look at the macro and micro changes seed in glomer 9:55 ular nephritis 9:56 and to distinguish between the different types of nephrotic syndrome. In renal 10:02 biopsy you 10:03 take a sample of the kidney tissue, usually ultrasound guided. After renal bi 10:10 opsy is 10:11 taken three things are checked. First, light microscopy which looks at the 10:19 general change 10:21 in the kidney tissue, particularly the head of the nephron where the glomerulus 10:28 is. 10:28 Two, immunofluorescence. Here, they expose the kidney tissue with specific 10:35 things that 10:36 will bind to antigens, immune complexes and immunoglobulins in that tissue. 10:44 Once they 10:45 expose the biopsy with these tags, it will light up with immunofluorescence. 10:52 This will 10:52 tell the person if there is or there isn't presence of those things they were 10:57 looking 10:57 for. 10:59 Number three, finally there is electron microscopy, which looks at the detailed 11:04 architecture of 11:05 the glomerulus, specifically the membrane of the glomerulus where the problems 11:10 might be 11:10 occurring. 11:13 The management of nephrotic syndrome depends on what the type is and it won't 11:18 be discussed 11:19 in this video. Thank you for watching.