Normal Labour
| Definition Labour: Cervical change accompanied by regular uterine contractions Abnormal Labour (Dystocia or arrest): Any deviation from the definition of normal labour "Show": As a result of the dilatation of the cervix, the operculum, which formed the cervical plug during pregnancy is lost. The women may see a blood stained mucoid discharge hours before, or within a few hour after labour starts. |
Overview
Labour is the period from the onset of regular uterine contractions until expulsion of the placenta. Labour can be either:
- Spontaneous labour
- Induced labour (Discussed at the end)
Labour can be a "true" labour or a "false" labour. Braxton Hicks contractions are mild, often irregular contraction that may occur from 30weeks gestation and often confused as true labour. True labour is characterised by:
- Painful uterine contractions at REGULAR intervals
- Contraction with increasing intensiry and duration
- The show occuring
- Progressive effacement and dilatation of the cervix
- Formation of the bag of waters
Labor is determined by assessing the cervical change versus time. Labour is initiated by the stretching of the cervix causing the release of oxytocin from the posterior pituitary gland
Stages of Labour - three stages
- 1st Stage
- Latent phase (cervical effacement and dilatation up to 3/4cm)
- Active phase (3/4cm to full dilatation)
- 2nd Stage - Full cervix dilatation until baby is born
- 3rd Stage - Placental delivery
| Watch Video: Stage I of Labour |
The foetus ready for a normal labour
- The foetal lie is longitudinal
- The presentation is cephalic
- The position is right or left occipitoanterior
Mechanism of normal labour - Movement of baby through the pelvis during labour
- Engagement
- Descent
- Internal Rotation
- Crowning and extension
- Restitution
- External Rotation
- Delivery of anterior shoulder
- Delivery of posterior shoulder
| Side note Shoulder dystocia is a complication of labour and is where the anterior shoulder is stuck at the pubic symphysis (more discussed in the shoulder dystocia section). |
Monitoring during labour
- CTG throughout - assessed every 30min
- Contraction - assessed every 30min
- Maternal pulse - assessed every 30min
- Maternal Blood pressure and Temperature - assessed 4 hourly (or hourly if complicated)
- Maternal urine - assessed 4 hourly
- Vaginal Examination - offered 4 hourly to see progress of cervical dilatation.
| NORMAL LABOUR PARAMETERS | ||
| Nulliparatous | Multiparatous | |
| First Stage - Latent Phase | <20hr | <14hr |
| First Stage - Active Phase | >1.2cm/hr | >1.5cm/hr |
| Second Stage | <2hr (<3hr if epidural) | <1hr (<2hr if epidural) |
| Third Stage | <30min | <30min |
| Remember During 1st stage, 1-1.5cm cervical dilatation should take ~1hour for nulliparous women. This is quicker for multiparous women. |
| Remember During 2nd stage labour, birth should take place within 3hr for nulliparous women and within 2hr for multiparous women (on epidural). |
Labour can be either:
- Spontaneous labour
- Induced labour - medical intervention helps induce labour
Induction of Labour As a general principle, induction of labour is undertaken when continuing a pregnancy is associated with greater level of maternal or foetal risk than delivery. 20% of all pregnancies are induced. The Bishops score helps assess the favourability for induction of labour.
| MODIFIED BISHOP'S SCORING SYSTEM (A total score >8 indicates a favourable cervix) | |||
| Cervix | SCORE | ||
| 0 | 1 | 2 | |
| Position | Posterior | Axial | Anterior |
| Length | 2cm | 1cm | <0.5cm |
| Consistency | Firm | Soft | Soft amd Stretchy |
| Dilatation | 0 | 1cm | >2cm |
| Station of the presenting part | -2 | -1 | 0 |
Indications for Labour Induction (IOL)
- Obstetric indication
- Uteroplacental insufficiency (most common)
- Prologed pregnancy (>40weeks)
- Interuterine Growth Restriction
- Non-reassuring CTG
- Severe Pre-eclampsia
- Medical Indication
- Gestational Diabetes (If on insulin and poorly controlled)
- Pre-eclampsia and eclampsia
Methods of labour induction
- Prostaglandins (dinoprostone) → causes uterine contraction (can be either administered via vaginal gel/orally)
- Oxytocin infusion → causes uterine contraction
- Cervical ripening. Either:
- Stretch and sweep
- Artificial rupture of membranes (Amniotomy)
- Transcervical Foley catheter
When labour has progressed to full dilatation and concerns exist regarding wellbeing of the fetus, mother, or both, three options exist
- Allow the labour to proceed as normal aiming for spontaneous vaginal birth
- Proceed to instrumental vaginal birth also known as operative
- Perform a caesarean section
Normal Labour - Instrumental Vaginal Delivery
Instrumental Vaginal Delivery Labour is divided into 3 stages. Stage 2 of labour (the stage from full cervical dilatation to the expulsion of the baby from the uterus) sometimes can be difficult and prolonged. Instrumental vaginal delivery helps with this stage and reduced need for caesarean section which is associated with more complications.
Indications for instrumental vaginal delivery
- Suspected or anticipated fetal compromise
- Maternal Exhaustion
- Prolonged 2nd stage (>1hr of active pushing in multiparous women or >2hr in primiparous women
- Medical intervention to avoid Valsalva (cardiac disease, hypertensive crisis, spinal injury)
| Remember to discuss the need for instumental delivery, process and alternative options (caesarean section). Consent must be obtained. |
Criteria for Intrumental vaginal delivery - FORCEPS
- Fully dilated cervix
- Obstruction should be excluded
- Ruptured membranes
- Consent, Catheterized bladder, Check instruments prior to application
- Epidural anaesthesia, Explained the procedure, Examine the vagina area for signs of trauma
- Presentation and postiion of fetal head, Power of uterine contraction, Placement of forceps bladers or venouse cup
- Station of the presenting part, Senior help if needed
| Remember Postnatal care following instrumental vaginal birth requires attention to analgesia, voiding function, thromboembolic prophylaxis, rehabilitation of the pelvic floor, and counselling regarding the index birth and future births. |
Instruments used for Vaginal Delivery
- Forceps
- Ventouse (vacuum)
| Side note Ventous appears safe for mother but forceps may be safer for baby. |
Complications of instrumental vaginal delivery
- Maternal trauma
- Vaginal trauma
- Postpartum haemorrhage
- Urinary tract injury
- Damage to pelvic floor and anal sphincter
- Fetal complication (rare)
- Shoulder dystocia and its consequences
- Subaponeurotic/subgaleal haemorrhage
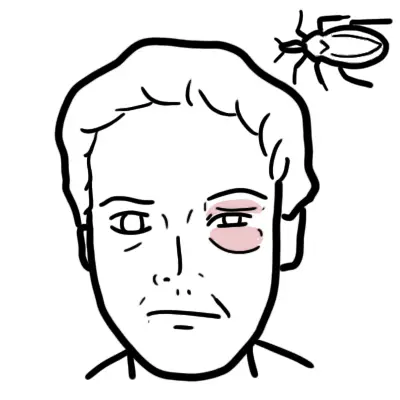
- Facial nerve palsy, corneal abrasion, retinal haemorrhage
- Skull fracture and/or intracranial haemorrhage
- Cervical spine injury
Risk Factors for failed instrumental vaginal delivery
- Obese women (BMI >30)
- Macrosomia
- Occiptoposterior position
- Mid-cavity, or when 1/5 of the fetal head is palpable abdominally
Normal Labour - Episiotomy
Episiotomy is a surgically planed cut to enlarge the vaginal introitus so as to facilitate easy and safe delivery of the foetus.
| Definition Episiotomy: is a surgically planned incision on the perineum and the posterior vaginal wall during te second stage of labour Perineal tears: Laceration of the perineum are the result of overstretching or too rapid stretching of the tissues, especially if they are poorly extensile and rigid. |
Consider episiotomy in the following circumstances:
- High likelihood of severe laceration
- Soft tissue dystocia
- Requirement to accelerate the birth delivery of a compromised foetus
- Need to facilitate operative (instrumental) vaginal delivery
- History of female genital mutilation
| Remember Bulging thinned perineum during contraction just prior to crowning is the ideal time for performing a episiotomy. |
Type of episiotomy
- Mediolateral episiotomy
- Midline episiotomy
Complications of episiotomy
- Extension of the incision to involve th rectum
- Vulval haematoma
- Infection
- Wound dehiscence
- Injury to anal sphincter causing incontinence of flatus or faeces
- Rectovaginal fistula (rare)
- Necrotising fascitis
- Dysparenuia
- Chance of perineal lacerations
- Scar endometriosis (rare)
| Remember Episiotomy should be restricted to use in situations in which it is clearly indicated, and should not be routinely used during normal vaginal delivery. |
Perineal tears
- There are four classes
Repair of perineal tears
- Done as soon as possible
- Examine the rectum to make sure no trauma to anal sphincter complex
Failure To Progress (Labour Arrest)
Failure to progress also known as labour arrest, labour dystocia or abnormal labour is used to describe a labour pattern deviating from the observed (normal) in the majority of women who have a spontaneous vaginal delivery. About 20% of all labors ending in a live birth involve failure to progress.
Risk Factors
- Hypocontractile uterine activity
- Older maternal age
- Nulliparous women
- Short stature
- Maternal obesity
- Macrosomia
- Cephalopelvic disproportion
- Non- occiput anterior position
- Bandl's ring
- Uterine abnormality
- Postterm pregnancy
| Bandl's Ring An hourglass constriction ring of the uterus. Complication associated with obstructed labor in the second stage. The constriction forms between the upper contractile portion of the uterus and the lower uterine segment. |
| Remember Occipito-anterior position is the most common position (either left or right). |
Diagnosis
| NORMAL LABOUR PARAMETERS | ||
| Nulliparatous | Multiparatous | |
| First Stage - Latent Phase | <20hr | <14hr |
| First Stage - Active Phase | >1.2cm/hr | >1.5cm/hr |
| Second Stage | <2hr (<3hr if epidural) | <1hr (<2hr if epidural) |
| Third Stage | <30min | <30min |
Labour pattern deviating from the above normal labour parameters is considered abnormal labour or failure to progress. Other interventions are indicated such as instrumental delivery or most often caesarean section.
Caesarean Section
Overview Caesarian delivery is the surgical removal of the infant from the uterus through an incision made in the abdominal wall and an incision made in the uterus. Incidence is 15-30%. Caesarean sections can be done as a planned procedure (elective) or as an emergency.
| Definition Vaginal Delivery: Vaginal delivery is a natural process that usually does not require significant medical intervention Caesarean Delivery: Operation performed to deliver a viable fetus through an abdominal incision and is used as an alternative route to the natural vaginal birth Instrument Caesarean Delivery: |
Types of Caesarean Delivery
- Low segment transverse - incision made transversely in lower segment of uterus (most common)
- Classic - vertical incision is made directly into the wall of the body of the uterus (not common)
Indications
- Previous caesarean section
- Dystocia or dysfunctional labour
- Fetal distress
- Breech presentation
- Antepartum haemorrhage
- Maternal problems
- Caesarean section on demand
Anaesthesia
- Spinal Anaesthesia
- Epidural Anaesthesia
- General Anaesthesia
Intrapartum Complications
- Primary haemorrhage
- Injury to internal organs
- Injury to the baby
- Difficulty in delivery of the head
- Anaesthetic complications
Postoperative Complications
- Paralytic ileus
- Respiratory complications
- Infections
- Peritonitis
- Pelvic abscess
- Pelvic thrombophlebitis
- Deep vein thrombosis and pulmonary embolism
- Wound dehiscence
Occipitoposterior Position
Occipitoposterior Position (OP) is the most common foetal malposition. Before labour, 15-20% of term foetuses in cephalic presentation are OP, but only 5% at vaginal delivery remain OP because most spontaneously rotate to Occipitoanterior position during labour.
| Remember The most common foetal position is left or right anteriorposterior position, cephalic presentation. |
Occipitoposterior Position (OP) and consequences on labour
- OP position can cause protraction of the 1st or 2nd stages of labour, or even arrest the second stage
- Women with an OP foetus are more likely to undergo interventions to hasten labour progress
- Other delivery complications: ↑risks of anal sphincter injuries, failed forceps or vacuum delivery, and inadvertent extension of the hysterotomy at caesarean
- ↑Neonatal adverse outcomes - Low APGAR, birth trauma
| Risk Factors |
| Nulliparity |
| Maternal age >35 years |
| Obesity |
| Previous OP delivery |
| Decreased pelvic outlet capacity |
| Gestational age ≥ 41 weeks |
| Birth weight ≥ 4000g |
| Anterior placenta |
| Epidural anaesthesia |
Treatment OP position antepartum is not predictive of foetal position at delivery or adverse outcome, as 95% rotate to OA by delivery. Intrapartum management occur in second stage of labour and include:
- Digital manual rotation (to rotate to OA prior to vaginal delivery)
- Operative vaginal delivery from OP position
- Caesarean delivery
| Remember Manual rotation in first stage has no benefits and may lead to cord prolapse. |
| Side note Doctor can attempt manual rotate OP at 36 weeks or 37-38 weeks to a AP. |
Breech Presentation
Breech presentation is normal in preterm pregnancy (<37 weeks gestation) and should not be considered abnormal, requiring intervention, until 37 weeks pregnancy is reached (at term). Breech presentation incidence of 40% at 20 wks gestation but incidence decreases with gestational.
| Definition Breech Presentation: When the buttocks, foot or feet are presenting instead of the head in a longitudinal lie. |
Breech Classification:
- Frank breech: where the hips are flexed and legs extended (65-70%)
- Complete breech: hips & knees are flexed + feet not below the level of the fetal buttocks (30%)
- Footling breech (incomplete): where hips are not completely flexed and one or both feet are presenting as the lowest part of the fetus
| RISK FACTORS | |
| Maternal Factors | Foetal Factors |
| Polyhydramnios | Prematurity |
| Uterine anomalies e.g. bicornuate, septate | Foetal anomalies e.g. neurological, hydrocephalus, anencephaly |
| Space occupying lesions e.g. fibroids | Multiple pregnancy |
| Placental abnormalities e.g. placenta praevia | Foetal death |
| Contracted maternal pelvis | Short umbilical cord |
| Multiparity (esp grand multips) | |
Diagnosis
- Abdominal palpation
- Pelvic examination: head not felt in pelvis (buttocks and/or feet may be felt)
- Ultrasound scan will confirm diagnosis
Treatment
- Perform External Cephalic Version at 37 weeks → vaginal delivery
- Planned caesarean section for 39 weeks
- Vaginal breech delivery
| External Cephalic Version (ECV) procedure involves placing hands on mother’s abdomen (externally). The fetal bottom is then moved away from pelvis and fetus genty turned in several steps from breech, to a sideways position, and finally to a head-first position (cephalic) (~50% success rate and allows for vaginal delivery). |
| Remember Almost 90% foetuses presenting by the breech at term are delivered by caesarean section. |
Maternal Collapse at Delivery
| Medical Causes | Condition |
| 6 H's | Hypovolaemia, Hypoxia, Hypoglycaemia, Hydrogen ions (acidosis), Hyper/Hypokalaemia, Hypothermia |
| 6 T's | Tension pneumothorax, Tamponade, Thrombosis (MI), Thromboembolism (PE), Trauma, Toxins |
| Obstetrics Causes | Condition |
| During Pregnancy | Ectopic pregnancy Antepartum Haemorrhage, Pre-Eclampsia/Eclampsia, Septic Shock |
| During Labour/Delivery | Amniotic Fluid Embolism (→ cardiorespiratory collapse), Inversion/rupture of uterus, Prolapsed cord, Shoulder dystocia, Acute foetal distress, Cardiac arrest |
| Post-Partum | Post-partum haemorrhage; Infection |
Major causes of Maternal mortality
- Postpartum haemorrhage
- Heart disease
- Pregnancy induced hypertension
- Amniotic embolism
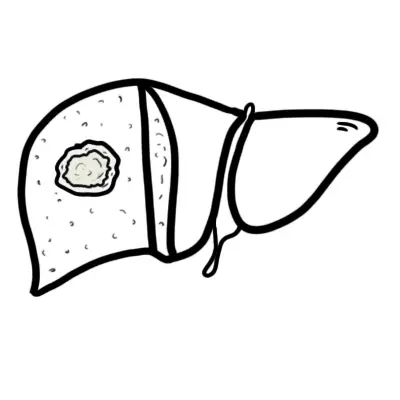
Uterine Rupture
Uterine rupture occurs in 2 per 10,000 of all pregnancies. It is a rare but significant event. It may occur before or after birth and can vary in size.
| Definition Uterine Rupture: disruption of the uterine muscle extending to and involving the uterine serosa or disruption of the uterine muscle with extension to the bladder or broad ligament. Uterine dehiscence: disruption of the uterine muscle with intact uterine serosa. |
Risk Factors
- High parity
- Multiple pregnancy
- Previous uterine trauma
- Previous uterine surgery
- Induction and/or augemntation of labour
- High or mid cavity forceps
- Obstructed labour (with or without Bandl's Ring)
- Direct trauma
- Extension of a cervical laceration
- Internal manipulation to correct unstable lie or malpresentation
Clinical Manifestation
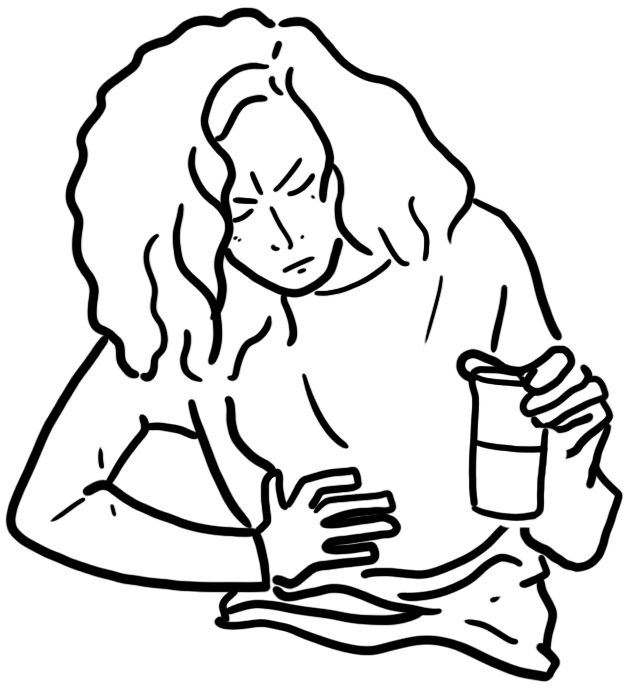
- Cessation of previously effective contractions
- Tonic/hypertonic contractions
- Pain unrelated to contractions
- Pain over the uterine scar
- Should tip pain (rupture)
- Antepartum haemorrhage
- Post partum haemorrhage
- Haematuria
- Fetus palpated in maternal abdomen
- Loss of station of the presenting part
- Abnormal fetal heart rate pattern
Treatment
- Call of help!
- Resuscitate
- Cease oxytoxin if in progress
- Monitor ongoing blood loss
- Monitor foetus
- Prepare for immediate transfer to theatre to expedite birth
- Surgical repair or hysterectomy
| Remember After the emergency Document, Debrief and Disclosure. |
Complications
- Maternal haemorrhage (concealed or revealed)
- Damage to other pelvic structures
- Hysterectomy
- Fetal compromise and possible demise
- Maternal death
Uterine Inversion
Uterine inversion occurs when the uterine fundus inverts within the endometrial cavity. 1 in every 2,500 births.
| Side note Uterine inversion can follow both vaginal and caesarean births and frequently occurs with the placenta still attached. |
Stages of uterine inversion
- 1st degree - the fundus inverts/dimples and reaches the internal os
- 2nd degree - the body of the uterus is inverted and protrudes through the cervix
- 3rd degree - the uterus completely inverted and appears outside the vulva
Risk Factors
- Adherent placenta
- Uterine abnormalities
- Precipitate labour and birth
- Multiparity
- Prolonged labour
- Short umbilical cord
- Performing controlled cord traction prior to placental seperation
- Manual removal of placenta
Clinical Manifestation
- Lower abdominal and/or bakc pain
- Excessive blood loss
- Fundus feels dimpled or not its proper position on abdominal palpation or vaginal examination
- Uterine protrusion through the cervix visible on speculum or palpated on vaginal examination
- Uterine protrusion at the introitus
- Shock disproportion to observed blood loss
Treatment
- Call for help
- Resuscitate
- Manual replacement
- Consider uterine relaxation with beta-mimetic agents (tetrabutaline, nitroglycerin)
- Hydrostatic replacement
- Remove placenta in operating theatre
- After placenta removal, commence aggressive PPH
- Commence antibiotics
| Remember do not attempt to remove the placenta (to prevent further haemorrhage). |
Complications
- Maternal shock and collapse
- Post partum haemorrhage
- Pain
- Hysterectomy
- Endometritis
- Damage to intestines and/or other pelvic anatomy
Umbilical Cord Prolapse
Umbilical cord prolapse is a true obstetric emergency requiring immediate delivery. It is when the umbilical cord descends through the cervix alongside or past the presenting fetal part in the presence of ruptured membranes. If the cord is compressed, the foetus will die within 5-10 mins.
| Definition Cord Prolapse: The umbilical cord lies in front of or beside the presenting part in the presence of ruptured membranes. Cord Presentation: The presence of the umbilical cord between the presenting part and the cervix. |
Aetiology Mechanism of Foetal Death is from compression of the umbilical vessels by the presenting part and/or umbilical arterial vasospasm due to exposure of cord → acutely compromised foetal circulation→ foetal death or neurological sequelae unless immediate delivery.
Difference between Cord presentation and Cord prolapse In both conditions, a loop of the cord is below the presenting part. Difference is condition of membranes:
- If membranes intact - cord presentation
- If membranes ruptured - cord prolapse
Incidence Cord Prolapse
- 0.1-0.6% overall incidence
- Higher in breech ~1%
- Perinatal mortality rates up to 20-30%
Clinical Identification of Cord Prolapse
- Visual inspection or palpation during vaginal exam - Umbilical cord is visualised or felt below or beside the presenting part
- Abnormal CTG changes:Bradycardia and Severe decelerations (atypical, variable, prolonged)
| RISK FACTORS FOR CORD PROLAPSE | |
| Pregnancy risk factors | Procedure-related |
| Placenta praevia | Obstetric manipulation increases risk →50% cases cord prolapse preceded by obstetric procedure |
| High / ill-fitting presenting part | Artificial Rupture of Membranes (ARM) especially if high-presenting part |
| High parity | Rotational instrumental delivery |
| Multiple pregnancy | Application of uterine pressure transducer |
| Prematurity | Vaginal manipulation of foetus with ruptured membranes |
| Polyhydramnois | |
| Malpresentations | |
| Long umbilical cord | |
| Remember Over 50% of cases of cord prolpase are preceded by an obstetric procedure. |
Complications
- Foetal Hypoxia
- Foetal Death
- Neonatal Hypoxic Ischaemic Encephalopathy
- Neonatal Death
- Maternal - increased operative birth and associated complications
Treatment
- Recognise and call for help!
- Initiate immediate assessment of clinical circumstances (gestation, presentation, cervical dilatation, foetal wellbeing. Immediate delivery is necessary when the foetus is viable)
- Relieve pressure on cord to prevent compression:
- Trained person to place hand in vagina to push presenting part out of the pelvis to maintain blood flow → continue until delivery
- Roll the women into either: Knee chest, exaggerated Sim's or Trendelenberg position
- Urinary bladder may be filled with fluid via catheter to elevate presenting part - If there will be a long DELAY in delivery
Side note Excessive handling of the cord may cause it to spasm
- Administer oxygen to the woman via a mask
- Discontinue oxytocics if present
- Tocolytics to abolish uterine contractions
- DELIVERY MUST BE EXPEDITED TO REDUCE MORBIDITY AND MORTALITY TO THE FOETUS
| Remember Paediatrician or neonatologist needs to be present. Remember paired cord blood samples of pH and base excess! |
| Remember After the emergency Document, Debrief and Disclosure. |
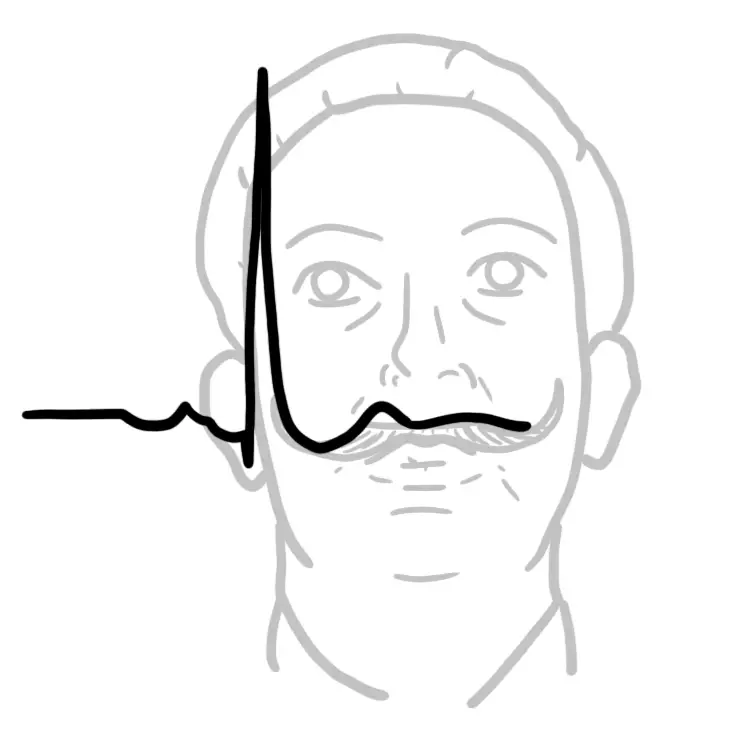
Shoulder Dystocia
Shoulder dystocia is defined as a vaginal cephalic delivery that requires additional obstetric manoeuvres to deliver the foetus after the head has delivered and gentle traction has failed. Shoulder dystocia cannot be predicted nor prevented in the majority of cases. Brachial plexus injury (BPI) is one of the most important fetal complications of shoulder dystocia. Maternal morbidity is increased, particularly the incidence of postpartum haemorrhage as well as third and fourth-degree perineal tears.
| Definition Shoulder Dystocia: Inability of the fetal shoulders to deliver spontaneously, usually due to the impaction of the anterior shoulder behind the maternal symphysis pubis. McRobert's Manoeuvre: The maternal thighs are sharply flexed against the maternal abdomen to straighten the sacrum relative to the lumbar spine and rotate the symphysis pubis anteriorly toward the maternal head. Suprapubic pressure: The operator’s hand is used to push on the suprapubic region in a downward or lateral direction in an effort to push the fetal shoulder into an oblique plane and from behind the symphysis pubis. Erb Palsy: A brachial plexus injury involving the C5-C6 nerve roots, which may result from the downward traction of the anterior shoulder; the baby usually has weakness of the deltoid and infraspinatus muscles as well as the flexor muscles of the forearm. The arm often hangs limply by the side and is internally rotated. |
| Risk Factors for Shoulder Dystocia |
| Maternal |
| Abnormal pelvic anatomy |
| Gestational diabetes |
| Post-dates pregnancy |
| Previous shoulder dystocia |
| Short stature |
| Fetal |
| Suspected Macrosomia |
| Labour related |
| Assisted vaginal delivery (forceps or vacuum) |
| Protracted active phase of first-stage labor |
| Protracted second-stage labor |
Management (HELPERR)
- Call for Help
- Evaluate for Episiotomy
- Legs: McRoberts Maneuver
- External Pressure - suprapubic
- Enter: rotational maneuvers
- Remove the posterior arm
- Roll the patient to her hands and kness
| Remember The biggest risk factor for shoulder dystocia is fetal macrosomia, particularly in a woman who has gestational diabetes. |
Maternal Complications of Shoulder Dystocia
- Postpartum hemorrhage
- Rectovaginal fistula
- Symphyseal separation or diathesis, with or without transient femoral neuropathy
- Third- or fourth-degree episiotomy or tear
- Uterine rupture
Fetal Complications of Shoulder Dystocia
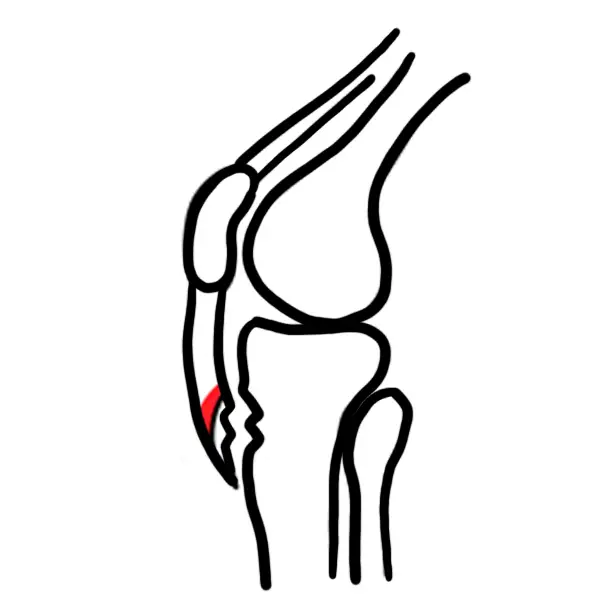
- Brachial plexus palsy
- Clavicle fracture
- Fetal death
- Fetal hypoxia, with or without permanent neurologic damage
- Fracture of the humerus
| Remember The most common injury to the neonate in a shoulder dystocia is brachial plexus injury, such as Erb palsy. |
Amniotic Fluid Embolism
Amniotic fluid embolism is a rare and potentially catastrophic, but poorly understood condition that is unique to pregnancy. It may range from a relatively minor subclinical episode through to one which is rapidly fatal.
| Definition Amniotic Fluid: Amniotic Fluid Embolism: Venous Thrombo Embolism: |
Risk Factors - not really well understood could be an interplay of:
- Advanced maternal age
- Placenta praevia
- Placental abruption
- Operative delivery
- Induction of labour
Clinical Presentation often occur in the intrapartum and immediate postpartum period
- Hypotension
- Fetal distress
- Pulmonary oedema or ARDS
- Cardiopulmonayr arrest
- Cyanosis
- Coagulopathy
- Dyspnoea
- Seizure
- Uterine atony
- Bronchospasm
| Amniotic Fluid Embolism Triad: Hypotension, Fetal distress and pulmonary oedema/ARDS. |
Diagnosis The diagnosis of AFE is a clinical one, based on the presence of cardiovascular and respiratory compromise and coagulopathy after the exclusion of other causes.
Treatment Supportive and advanced life support.
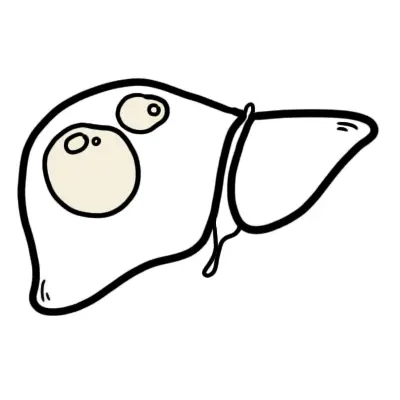
Invasive Implantation of placenta
Invasive implantation increases following caesarean section and is incrementally linked to the number of caesarean sections the woman has had.
| Definition Placenta accreta: Abnormal adherence of the placenta to the uterine wall due to an abnormality of the decidua basalis layer of the uterus. The placental villi are attached to the myometrium. Placenta increta: The abnormally implanted placenta penetrates into the myometrium. Placenta percreta: The abnormally implanted placenta penetrates entirely through the myometrium to the serosa. Often invasion into the bladder is noted. |
| Risk Factors |
| Placenta previa |
| Implantation over the lower uterine segment |
| Prior cesarean scar or other uterine scar |
| Uterine curettage |
| Fetal Down syndrome |
The usual management of placenta accreta (abnormal adherence of the placenta to the uterus) is hysterectomy.
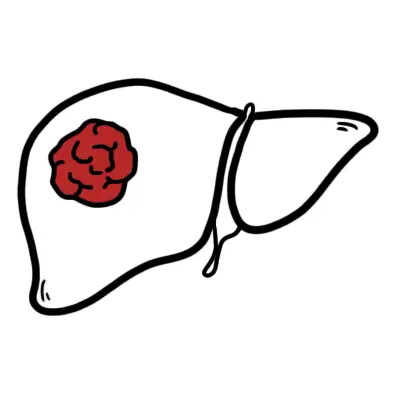
Postpartum Haemorrhage
Overview
Postpartum Haemorrhage is potentialy life-threatening and is one of the leading causes of maternal death. The incidence of PPH may be underestimated by up to 50%, due to the clinical difficulty in accurately estimating blood loss
- Minor PPH: blood loss of 500-1000mls
- Major PPH: blood loss of >1000mls
| Definition Postpartum Haemorrhage: a blood loss exceeding 500ml after delivery of the infant or any amout of blood loss postpartum that causes haemodynamic compromise in the women. Primary Postpartum Haemorrhage: occurs <24hours of delivery Secondary Postpartum Haemorrhage: occurs >24hours - 6weeks Antepartum Haemorrhage: Any bleeding from the genital tract after the 20 th week of pregnancy and before the onset of labour. |
| RISK FACTORS | ||
| Maternal | Current Pregnancy | Labour |
| Previous PPH | Antepartum Haemorrhage | Long labour (>12hrs) |
| ↑Age | Multiple pregnancy | Syntocinon in labour |
| High parity | Macroscomia | Operative delivery |
| Coagulation disorders | Caesarean section | |
| Anaemia | ||
Causes of post partum haemorrhage:
- Tone - Uterine atony (90%)
- Trauma - Lacerations of the genital tract (6%) - Trauma-related bleeding can be due to lacerations, surgical incisions, or uterine rupture.
- Tissue - Retained placenta and abnormal placenta (3-4%)
- Thrombin - Coagulation disorders, thromcytopaenia associated with pre-eclampsia, amniotic fluid embolism, severe infection
| Remember 4Ts for the causes of PPH: Tone, tissue, trauma, thrombin. |
Maternal morbidity and mortaility from PPH is caused by:
- Hypovolaemia → ↓cardiac return → ↓Cardiac output→ ↓BP → ↓Renal/hepatic organ failure, Acute respiratory syndrome, Sheehan's Syndrome and DIC
Prevention
- Antenatal detection and correction of anaemia (morbidoty ↑ for anaemic women)
- Active management of 3 rd stage of labour for all women- MOST effective as it ↓ risk PPH by 50%
- Adminstering an Oxytocic with the anterior should
- Early cord clamping and cutting
- Delivery of placenta by controlled cord traction whilst guarding the uterus
- Post-delivery - check & repair genital trauma early, confirm placenta & membranes complete, observe any blood loss for clotting, regular observations
| Remember Significant haemorrhage can occur rapidly as maternal blood circulates through uterus at 500-800mL/min and 2/3 cases of PPH cannot be predicted. |
Treatment
- Call for help
- Lie women flat, uterine massage, keep women warm
- Resuscitate (O2 , IV access, fluids, catheter, monitor vitals)
- Assess Aetiology - 4Ts - Treat depending on Aetiology
- Abdominal assessment of uterus
- fundal massage to expel any products and promote contraction
- explore lower genital tract for trauma
- check placenta and membrane for completeness (tissue)
- review history and observe clots (thrombin)
Atony PPH Management Adminstration of medicine: promotes contraction of the uterine corpus - decreases the likelihood of uterine atony
- Massage the fundus and expel clots and products
- Oxytocin agents
- Ergometrine
- Prostagladins
- Mechanical stimulation of uterine contraction (massage of uterus through the abdomen and bimanual compression
- Surgical methods (If all methods above fail)
- Ligation of the uterine arteries
- Ligation of the hypogastric arteries
- Selective arterial embolisation
- Hysterectomy
| Remember the third stage of labor should be actively managed to reduce the risk of postpartum hemorrhage. |
| Side note Consider uterine rupture as trauma. There can be signs of shock with not visible blood loss. There is abdominal tenderness, shoulder tip pain. |
Preterm Labour and PPROM
| Definition Preterm Labour: Defined as delivery between 24 and 37 weeks Rupture of membranes (ROM): Leakage of amniotic fluid from the cervix Preterm Prelabour rupture of membrane (PPROM): Defined as rupture of membranes between 24 and 37 weeks in the absence of uterine activity (labour) Prelabour rupture of membrane (PROM): Defined as rupture of membranes in the absence of uterine activity (labour) after 37 weeks. NOT PRETERM |
Overview The diagnosis of preterm labour is generally based upon clinical criteria of regular, painful uterine contractions accompanied by cervical dilation and/or effacement between 24-27 weeks.
Investigations of preterm labour
- Transvaginal ultrasound
- Fetal fibronectin - positive are more likely to deliver. Fetal fibronectin is not usually present in cervicovaginal secretion before 22weeks
Aetiology of Preterm labour
- Multiple pregnancy
- Antepartum Haemorrhage
- Intrauterine growth restriction
- Cervical incompetence
- Chorioamnionitis
- Abnormal baby
- Congenital uterine anomaly
- Polyydramnios
- Infections - Bacterial vaginosis
- Iatrogenic
- Idiopathic
Prevention of preterm labour
- Infection is a cause of preterm labour - could antibiotics against bacterial vaginosis have a role?
- Progesterone
- Cervical cerclage
- Reduction of pregnancy numbers (as multi-pregnancy is associated with increased risk of preterm labour)
- Cessation of smoking/illicit drug use
Management of preterm labour
- Aim to prolong gestation but also to improve perinatal outcome
- Steroid therapy (IM dexamethasone to mother) - To induce pulmonary surfactant in the lungs of the immature fetus and prevent respiratory syndrome
- Tocolytics - β Sympathomimetic, nitrates, calcium channel blockers (Nifedipine), Oxytocin anatagonist
| Pharmacology Tocolytics. Contraindications: Antepartum haemorrhage, severe pulmonary Embolism, Maternal condition if pregnancy prolonged, heart disease and thyrotoxicosis (Salbutamol). |
Complication of Premature baby (as a result of preterm delivery)
- Respiratory Distress Syndrome
- Intraventricular Haemorrhage
- Necrotizing enterocolitis
- Neonatal jaundice
- Failure to thrive
- Cerebral Palsy
Preterm prelabour rupture of membranes
- Occurs in 33% of preterm deliveries
- 33% of PPROM associated with infection - do investigations!
| Chorioamnionitis |
Investigations
- FBC
- CRP
- Vaginal swab
- Urine analysis
- Ultrasound
Prelabour rupture of membranes