Overview
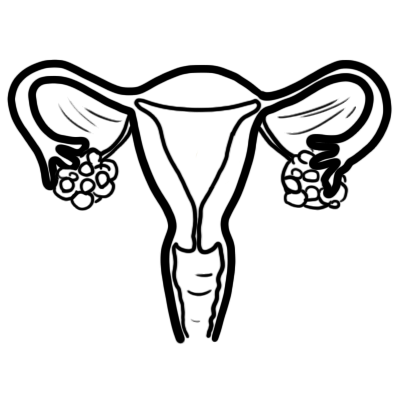
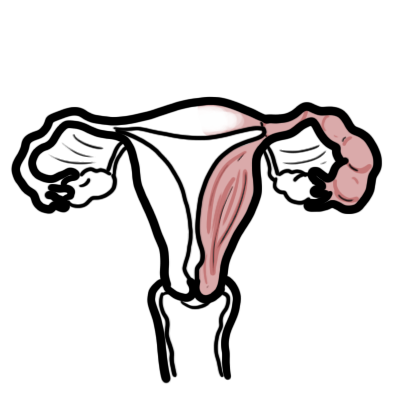
Overview Polycystic ovary syndrome is a common, lifelong condition that appears to be increasing in prevalence with increasing obesity, and is more common in Indigenous and southeast Asian women. PCOS is the presence of multiple follicular cysts in the ovaries (>12 cysts). PCOS results in hormonal imbalance resulting in the associated signs and symptoms (ie. infertility, androgenism)
| Definition Cyst: A cyst is a sac or pocket in your body filled with fluid, semi-solid material or air Ovarian cyst: Sac filled with liquid or semi-liquid material arising in an ovary. There are many differential diagnosis of ovarian cysts and majority are benign Polycystic Ovarian Syndrom |
Anatomy and Physiology Ovary
The Ovary
- Paired, situated on either side of the uterus
- Situated close to lateral pelvic wall
- Located in the ovarian fossa of Waldeyer
- The only intra-abdominal structure not covered by peritoneum
- Consists of the cortex and medulla
Ligaments associated with the Ovary
- Ovarian ligament - attaches to the ovary inferiorly and connects it to the uterus
- Suspensory Ligament of the Ovary - connect ovary to the lateral abdominal wall.
Blood supply
- Ovarian artery
- Right Ovarian vein: through pamipiniform plexus → Ovarian Vein → Inferior Vena Cava
- Left Ovarian Vein: through pamipiniform plexus → Ovarian Vein → Left Renal Vein → Inferior Vena Cava
Lymphatics
- Para aortic lymph nodes
Innervation
- Sympathetic supply from T10 along ovarian artery
Risk Factors
Family history of PCOS
- 50% of first-degree relatives

Risk Factors
Premature adrenarche – development of PCOS in 50% of cases
- Early adrenarche – ‘awakening’ of adrenal gland, sex hormones causing changes such as development of pubic hair, oily skin, oily hair, body odour (development of apocrine sweat glands)
| Side note Early adrenarche differs to puberty. Puberty is when body becomes capable of sexual reproduction, development of testes and ovaries → secondary sex characteristics |
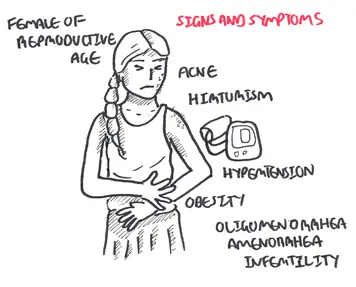
Signs and Symptoms
Clinical Presentation is often of a young women who experiences irregular periods +/- weight gain/hirsutism
Hyperandrogenism
- Acne
- Hirsutism - hair
Menstrual disturbance
- Oligomenorrhoea
- Secondary amenorrhoea
- Cystic ovaries
- Infertility
Obesity
- Hyperglycaemia
- Elevated oestrogens
Insulin resistance
- Dyslipidaemia
- Hypertension
| Cardinal Triad of PCOS: hyperandrogenism, presence of cysts in ovaries (>12) and anovulation |
Differential Diagnosis
- Congenital adrenal hyperplasia
- Hypothyroidism
- Hyperprolactinaemia
- Cushing's syndrome
| Congenital adrenal hyperplasia refers to enlarged adrenal glands. It is due to inherited enzyme deficiency. Congenital adrenal hyperplasia is the most common adrenal disorder of infancy and childhood.Congenital adrenal hyperplasia results excessive androgens (male hormones). There is also a severe salt-losing form of the condition. |
Differential Diagnosis for Ovarian Cysts
- Polycystic Ovarian Syndrome
- Endometriomatous Cysts
- Function cysts - most common
- Follicular cysts
- Theca luthein cysts
- Corpus luteum cysts
| Endometriomatous cysts of the ovary are cysts filled with blood arising from the ectopic endometrium. They usually enlarge pre and during menses and slightly shrink thereafter. The ovary is the commonest site of pelvic endometriosis |
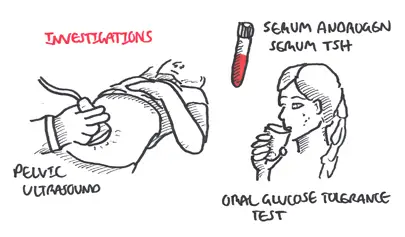
Investigations
- Serum quantitiative βhCG – exclude pregnancy, ectopic and trophoblastic disease
- Full Blood Count
- Blood Glucose Level
- Thyroid function tests (looking for hypothyroidism)
- Hormones: FSH/LH/Progesterone
- LH:FSH ratio 2.5:1
- Minor elevation of androgens
- Mild hyperprolactinaemia
- Ultrasound - vaginal or abdominal
Diagnosis
- Oligo/anovulation
- Hyperandrogenism
- Clinical (hirsutism or less commonly male pattern alopecia) or
- Biochemical (raised free androgen index or free testosterone)
- Polycystic ovaries on ultrasound (>12)
Other aetiologies must be excluded such as congenital adrenal hyperplasia, androgen secreting tumours, cushing syndrome, thyroid dysfunction and hyperprolactinaemia
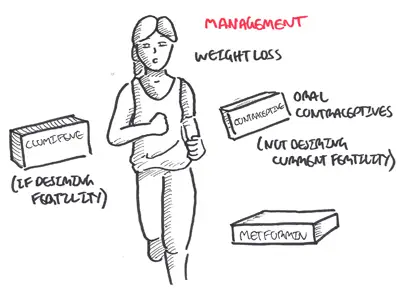
Management
Obesity - Weight loss
Amenorrhoea
- Use low dose combined oral contraceptive preparation
- Progestogen for 12 days every 1-3 months to induce withdrawal bleed
Hyperandrogenism and hirsutism
- Anti-androgens e.g. Dianette
- Cosmetic techniques
- Spironolactone – has anti-androgenic properties
Infertility
- Weight reduction through exercise and diet
- Clomifene citrate - induces ovulation
- Anovulatory infertility resistant to anti-oestrogens can try parenteral gonadotropin therapy or laparoscopic ovarian diathermy
- Metformin
| Pharmacology Clomifene is used mainly in female infertility due to anovulation to induce ovulation. Clomifene has both estrogenic and anti-estrogenic properties, but its precise mechanism of action has not been determined. Clomifene should only prescribed with ultrasound monitoring available to minimise the 10% risk of multiple pregnancy |
Ovarian diathermy
- Reduced risk of multiple pregnancy
- Similar pregnancy rate to gonadotropin therapy at 12 months
Insulin sensitising agents - Metformin
Complications and Prognosis
- Infertility
- Pregnancy complication (ie. spontaneous pregnancy loss)
- Type 2 Diabetes
- Non-alcoholic fatty liver disease
- Cardiovascular disease
- Obstructive sleep apnoea
- Psychological issues
- Metabolic syndrome
- Dyslipidemia
Infertility
Overview Infertility is defined as inability to become pregnant after 12 months of regular, unprotected intercourse. It is important to remember that infertility can arise from female factors, male factors or a combination of both. Approximately 85% of couples spontaneously conceive within 12 months. Those who are unable, warrant evaluation. Older women with risk factors for infertility may warrant evaluation at 6 months.
Risk Factors of Infertility
- Smoking
- Alcohol
- Obesity
- Older age
Aetiology of Infertility
- Combined factors from both partners (40%)
- Male factors (>30%)
- Ovulatory disorders (<30%)
- Fallopian tube disease (<20%)
- Endometriosis
- Coital problems
- Cervical factors
- Unexplained (~30%)
More information on Infertility
| Watch video Female infertility |