Notes »
clinical
» Paediatrics
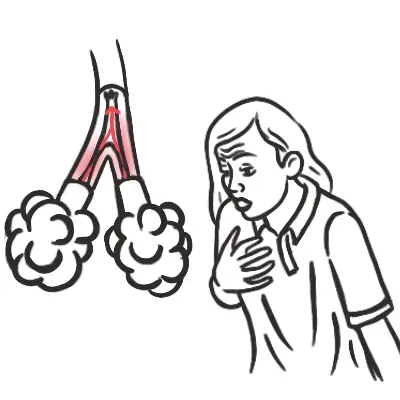
Wheeze
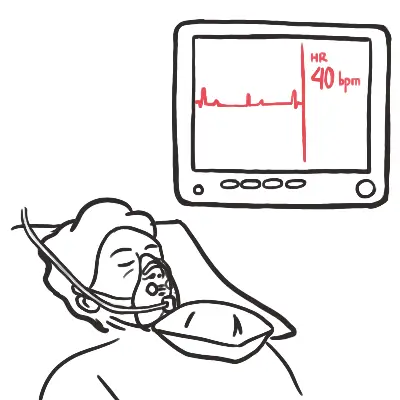
Overview Wheezing in infants and children is a common problem presented to primary care offices. Approximately 25 to 30 percent of infants will have at least one episode of wheezing. The presence of a wheeze implies narrowing of airways of any size throughout the proximal conducting airways. A wheeze requires sufficient airflow to generate the sound of a wheeze. Most infants and children with recurrent wheezing have asthma, but other causes should be considered in the differential diagnosis. Beware of the wheezing patient who suddenly becomes silent.
| Definition Wheeze: continous high-pitched whistling expiratory sound Stridor: caused by partial upper airway obstruction and is typically heard in inspiration, although it can also be heard on expiration if the obstruction is below the larynx (monophonic) Stertor: snoring sound Rhonchi: continuous low pitched, rattling lung sounds that often resemble snoring |
Mechanism of Wheeze
- Occurs during the prolonged expiratory phase by the rapid passage of air through airways that are narrowed to the point of closure.
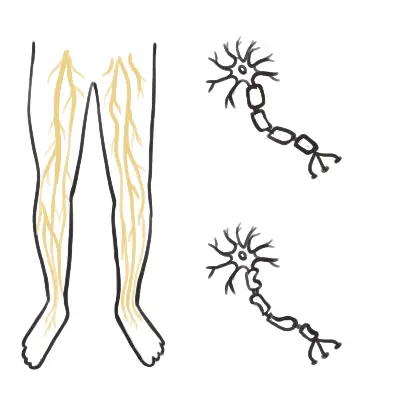
- Infants' and young children's bronchi are small, resulting in higher peripheral airway resistance → diseases that affect the small airways have a proportionately greater impact on total airway resistance in infants.
- Infants also have less elastic tissue recoil and fewer collateral airways, resulting in easier obstruction and atelectasis.
- The rib cage, trachea, and bronchi are also more compliant in infants and young children, and the diaphragm inserts horizontally instead of obliquely.
Approach
- History
- Onset
- Pattern
- Seasonality
- Cough
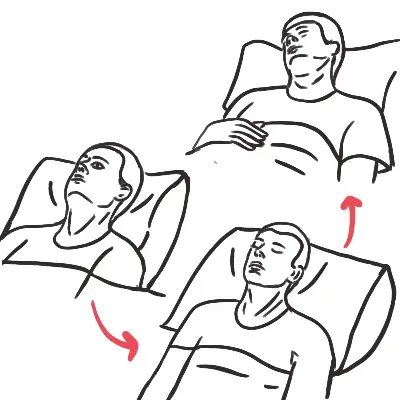
- Position changes
- Medical history
- Family History
- Examination
| Remember Beware of the wheezing patient who suddenly becomes silent. |
| DISTINGUISHING AETIOLOGY OF WHEEZING IN CHILDREN | |
| Questions | Indications |
| How old was the patient when the wheezing started? | Distinguishes congenital from noncongenital causes |
| Did the wheezing start suddenly? | Foreign body aspiration |
| Is there a pattern to the wheezing? | Episodic: asthma Persistent: congenital or genetic cause |
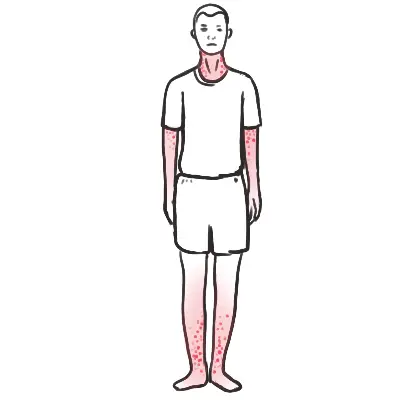
| Is the wheezing associated with a cough? | GORD/GERD, sleep apnoea, asthma, allergies |
| Is the wheezing associated with feeding? | GORD/GERD |
| Is the wheezing associated with multiple respiratory illnesses? | Cystic fibrosis, immunodeficiency |
| Is the wheezing associated with a specific season? | Allergies: fall and spring Croup: fall to winter RSV: fall to spring |
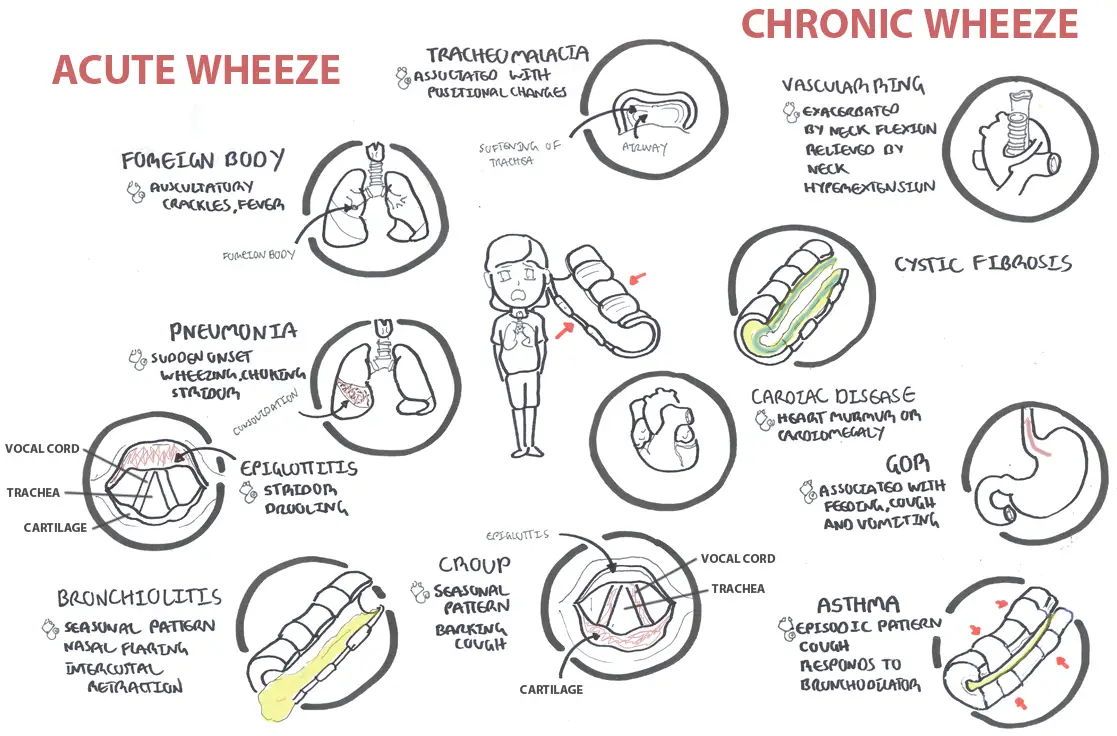
Differentials of wheeze in children
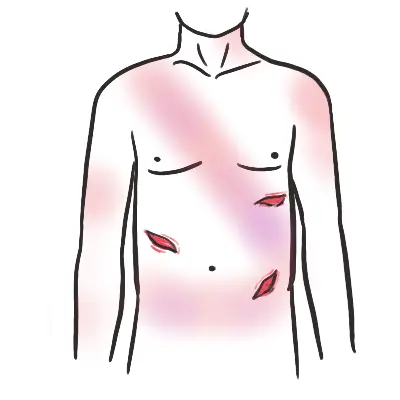
Investigations
- FBC
- Chest X-ray - if unexplained wheezing that is unresponsive to bronchodilators or with recurrent wheezing
- Bronchoscopy - Immediate bronchoscopy should be performed if foreign body aspiration is suspected
- Allergy testing
- Sweat chloride test - cystic fibrosis
- Serum immunoglobulin levels - Immunodeficient?
- Barium swallow - may detect vascular rings and esophageal compression.
- Computed tomography - can identify lung nodules and bronchiectasis, but these are uncommon causes of wheezing in children.
| Remember X-ray Features that suggest inhaled foriegn body include: Inspiratory (nothing), Expiratory can reveal gas trapping. If foreign body has been lodged for a long time à atelectasis (rather than gas trapping, due to the reabsorption of the gas). Hyper-inflated lung on opposite non obstructed lung. Tadioopaue ibject may be seen on chest C-ray |
| Side Note Foreign bodies are revealed in up to 70% of patients |
| DIFFERENCE BETWEEN TRANSIENT INFANT WHEEZE AND ASTHMA | |
| Transient Infant Wheeze | Asthma |
|
|