A healthy 25-year-old woman presents with worsening dysmenorrhea, pain of recent onset in the left lower quadrant, and dyspareunia. She has regular menstrual cycles, and her last menstrual period was 3 weeks before presentation. She has been trying to fall pregnant over the past 10 months without success and she is becoming more concerned.
Overview
Overview Endometriosis is defined as the presence of endometrial glands and stroma outside the endometrial cavity and uterine musculature. Like the endometrial tissue from which it is derived, endometrial implants and cysts respond to the hormonal fluctuation of the menstrual cycle. Endometriosis is a common condition associated with infertility and should be suspected in any infertile woman. Endometriosis affects 6-10% of women of reproductive age and is a major contributor to pelvic pain.
| Definition Endometriosis: The presence of endometrial glands and stroma outside the endometrial cavity and uterine musculature Endometritis: Inflammation of the endometrium usually by an infection Infertility: Inability to conceive after 1 year of unprotected intercourse. Primary Infertility: A woman has never been able to get pregnant. Secondary Infertility: A woman has been pregnant in the past, but has 1 year of inability to conceive. Dysmenorrhoea: Painful menstruation Dyspareunia: Difficult or painful sexual intercourse. |
Risk Factors
- Mullerian anomiles
- Diethylstilbestrol exposure in utero
- Early Menarche
- Late menopause
- Obesity
- Short menstrual cycles
- Low birth weight
- Exposure to endocrine disrupting chemicals
- Genetics
- Red meat and trans fat
| Side note Protective factors include fruit, green vegetables, n-3 long chain fatty acids, prolonged lactation and multiple pregnancies. |
Signs and Symptoms
Clinical Presentation Women with extensive endometriosis may have minimal symptoms. Whereas, women with minimal endometriosis may have severe pain.
- Severe dysmenorrhea
- Chronic Pelvic pain
- Deep dyspareunia
- Ovulation pain
- Chronic fatigue
- Pain on defecation
- Infertility
| Four Ds of endometriosis: dysmenorrhea, dyspareunia and dyschezia and dysuria. |
| Think Endometriosis should be considered a possible aetiology in patients who present with dysmenorrhea that does not respond to oral contraceptive or NSAIDs. |
| Side note In approaching infertility, there are five basic factors to examine: (1) ovulatory, (2) uterine, (3) tubal, (4) male factor, and (5) peritoneal factor (endometriosis). |
Clinical Examination
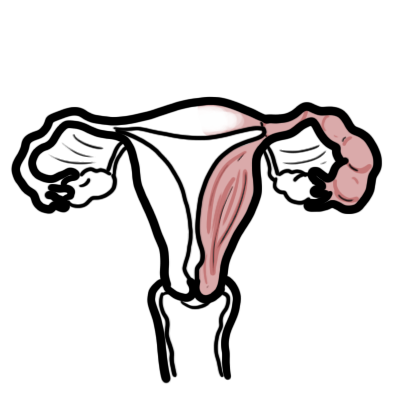
- Pelvic tenderness
- Fixed (immobile) retrograde uterus
- Tender/Thickened uterosacral ligaments which may be nodular
- Enlarged ovaries
Differential Diagnosis
Gyaenacological
- Adenomyosis
- Leiomyomata (Fibroids)
- Interstitial cystitis
- Pelvic Inflammatory Disease
- Ovarian cyst
- Uterine Myoma
Non-Gyaenacological
Investigations
- Transvaginal ultrasound (preferred)
- MRI
Diagnosis Laparoscopy is the “gold standard” in diagnosing endometriosis, and lesions may have a variety of appearances. The mean interval between the onset of pain and definitive surgical diagnosis is 10.4 years.
| Side note When surgical treatment is being considered, attempt laparoscopic excision or ablation at the time of diagnostic laparoscopy when possible. |
| Indications for Laproscopy |
| NSAID - resistant lower abdominal pain/dysmenorrhoea |
| Pain resulting in days off work/school or hospitalization |
| Pain and infertility investigation |
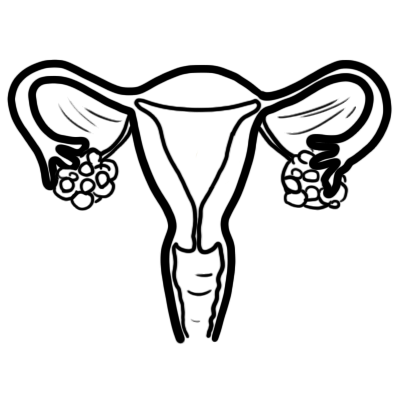
| Remember Endometriosis is most commonly found on the ovaries and is typically bilateral. |
Pathology
Gross and microscopic pathology Endometriosis lesions in the pelvis can be categorized into three types:
- Superficial peritoneal lesions - typically located on pelvic organ or pelvic peritoneum. Classical lesions are powder burn or gun shot lesions
- Ovarian lesions (endometrioma) - an ovarian cyst, or endometrioma, is formed when ectopic endometrial tissue within the ovary bleeds and results in a hematoma surrounded by duplicated ovarian parenchyma
- Deeply infiltrating endometriosis - a solid endometriosis mass situated more than 5 mm deep to the peritoneum
Pathophysiology
Theories
- Retrograde menstruation
- Vascular and lymphatic dissemination of endometrial cells
- Coelomic metaplasia of multipotential cells in the peritoneal cavity
- Impaired Immunity
Management
Management reasonable goals for management of endometriosis include reduction in pelvic pain, minimizing surgical intervention and preserving fertility
Hormonal treatment - mimic pregnancy or menopause
- Combined oral contraceptives
- Progestagens
- Intrauterine Devices (Mirena)
- Gonadotropin-releasing hormone agonists
- Aromatase inhibitors
| Side note all drugs are equally effective in relieving pain and are associated with up to 50% recurrence after approximately 12-24 months after stopping. |
Pain Treatment - Hormonal treatment helps alleviate pain
- NSAIDs may help
Surgical Treatment - eliminate all visible peritoneal lesions, endometriomas, deep endometriosis and associated adhesions, and to restore normal anatomy. May involve:
- Laparoscopic ablation
- Open Surgery with local resection
- Hysterectomy +/- oophorectomy
| Remember In the five years after surgery or medical treatment, 20-50% of women will experience recurrence of symptoms. |
Complications and Prognosis
Complications
- Ovarian failure post-surgical intervention
- Adhesions formation
- Endometriosis increases risk of developing autoimmune diseases
- Mental Health Illness
- Infertility
| Remember No medical treatment can improve fertility in endometriosis patients. |
Prognosis Endometriosis-associated pain can be managed by medical and surgical means, with a varying degree of recurrence and progression. Delays in diagnosis are common and result in untreated pain. Fertility issues depends on multiple factors.