Primary Hypothyroidism


Hypothyroidism: Variety of abnormalities that cause insufficient secretion of thyroid hormones. The most common cause is autoimmune thyroid disease
Primary Hypothyroidism: Clinical state resulting from underproduction of T4 and T3. Low free T4 with an elevated TSH is diagnostic of primary hypothyroidism. Autoimmune thyroiditis (Hashimoto’s disease) is the most common cause of primary hypothyroidism.
Secondary (Central) Hypothyroidism: The result of anterior pituitary or hypothalamic dysfunction.
Myxedema: Severe hypothyroidism in which there is accumulation of hydrophilic mucopolysaccharides in the ground substance of the dermis and other tissues leading to thickening of the facial features and doughy induration of the skin.
Subclinical hypothyroidism: Elevated TSH levels in the presence of normal concentrations of free thyroid hormones.
Hypothyroidism is a clinical state resulting from underproduction of the thyroid hormones T4 and T3. Most cases (95%) are due to primary hypothyroidism, a failure of the thyroid gland to produce thyroid hormones. Autoimmune thyroiditis (Hashimoto’s disease) is the most common cause of primary hypothyroidism. It affects women much more than men. In the developing world, iodine deficiency is a major cause of hypothyroidism. Drugs that can cause hypothyroidism include lithium and amiodarone. Six percent of post-partum women develop lymphocytic thyroiditis, which causes transient primary hypothyroidism.
Primary hypothyroidism is decreased production of thyroid hormones because of thyroid gland disease (most common is hashimoto’s thyroiditis). Secondary hypothyroidism is a problem in the Pituitary gland or hypothalamus resulting in ↓TSH leading to ↓Thyroid hormone production.
The thyroid gland is butterfly shaped endocrine organ that sits and wraps around the trachea. Anteriorly the thyroid glands are joined by the Isthmus. Developmentally, the thyroid isthmus can give rise to a structure contiguous called the pyramidal lobe, which extends upward.
Posteriorly the thyroid gland does not connect, however 4 parathyroid glands are attached onto the thyroid gland posteriorly.
The gland is in visceral compartment of the neck, along with the trachea, oesophagus and pharynx. The compartment is enclosed in the pre- tracheal fascia, which anchors the thyroid gland to the trachea, so that the thyroid moves up on swallowing.. The thyroid gland stands at the vertebral level C5-T1.
Embryologically, the thyroid gland begins its development at the base of the tongue before descending down to the trachea. This is the reason why thyroid ductal cysts can occur higher up on the neck, anywhere along the path of descent.
Arterial blood supply:
Venous drainage:
Physiology The thyroid gland produces 3 hormones:
Nongoitrous
Goiterous
General Hypothyroidism
Hashimoto’s Thyroiditis is associated with other autoimmune diseases including myasthenia gravis.
Clinical Examination
Hypothyroidism has slow deep tendon reflex.
Myxoedema (Medical Emergency) more info down the bottom
Investigations
Secondary hypothyroidism you will have ↓TSH as well as a ↓T3,T4. Might see decrease in other pituitary hormones.
If TSH is normal it is always euthyroid.
The goal of treatment is reduction of symptoms and prevention of long-term complications.Treatment is given upon establishing the diagnosis and is lifelong. Factors that affect drug dose must be considered.
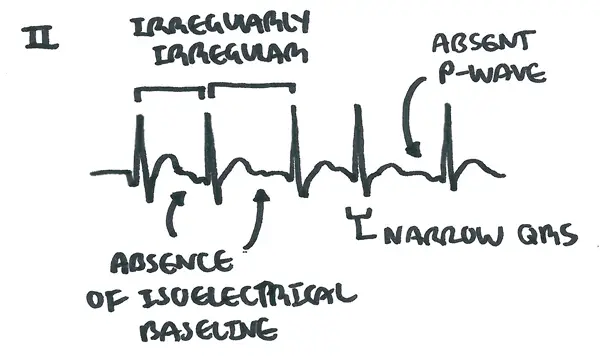
Levothyroxine (L-thyroxine) is a synthetically made thyroid hormone, mimicking T4. Side effects include increased risk of osteoporosis and atrial fibrillation. High doses can mimic hyperthyroidism state.

Complications
Prognosis is generally excellent with full recovery upon adequate replacement of thyroid hormones.
Myoxedema coma is a serious emergency, due to severe untreated hypothyroidism, and typically presents with impaired consciousness, hypoventilation and hypothermia. Hospitalizations is essential for initial treatment.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion