Overview
Overview Asthma is a chronic airway inflammation disorder due to complex interactions between inflammatory cells, mediators and airway cells. In young children in whom lung function testing is not feasible, including most preschool children, asthma is defined by the presence of variable respiratory symptoms. Asthma is one of the most common causes of presentation to the Emergency department It implies reversible airway constriction (peak flows vary by >20%) +/- wheeze, dyspnoea or cough
| Definition Asthma: Condition of bronchial hyperactivity and smooth muscle hypertrophy leading to a chronic inflammatory condition of the airways associated with widespread bronchospasm that is reversible. Acute cough: Condition for less than 3 weeks, most commonly caused by acute upper respiratory infection but also may be caused by congestive heart failure, pneumonia, and pulmonary embolism. Chronic cough: Condition for longer than 3 to 8 weeks (case definitions vary). Smoker - chronic obstructive pulmonary disease. Nonsmoker with a normal chest radiograph and not taking an ACE inhibitor, it may be due to postnasal drip, gastroesophageal reflux disease (GERD), or asthma. |
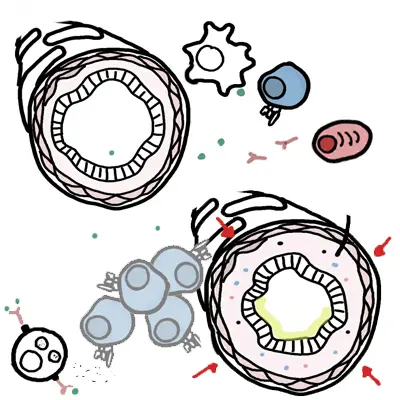
Airway obstruction occurs due to a combination of:
- Inflammatory cell infiltration
- Mucus hypersecretion with mucus plug formation
- Smooth muscle contraction
This page will mainly focus on paediatric asthma
Epidemiology
- Paediatric asthma is the most common chronic respiratory disease in the developed world, with the highest prevalence found in English-speaking countries such as the US, the UK, and Australia.
- Good control of asthma and prevention of exacerbations is important.
- There is a variable gender effect, with a higher prevalence in prepubertal males and postpubertal females
- Between 30-80% of children become asymptomatic around the time of puberty.
Patterns of Asthma
Infrequent intermittent asthma (70-75% of cases)
- Episodes of asthma lasting days to a week
- Episodes are generally 6 or more weeks apart
- Asthma triggered my URTI
- No need for preventer
Frequent intermittent asthma (20-25% of cases)
- Episodes occur at intervals less than 6 weeks
- Minimal symptoms between episodes
- Children may benefit from regular preventative therapy usually with ICS or Leukotriene antagonist
Persistent asthma (5-10% of cases)
- Symptoms on most days including:
- Disruption of sleep due to wheeze and cough
- Early morning dyspnoea
- Exercise dyspnoea or activity intolerance
- Require preventive therapy
- Referral to a paediatrician
Anatomy of the Respiratory Tract
Risk Factors
- Allergic sensitisation
- Atopy
- Family History
- Passive or Active tobacoo smoker
- Viral infections
- Higher serum eosinophils
Signs and Symptoms
| Asthma Triad CDE: Cough, Dyspnea, Expiratory wheeze |
Parental anxiety should not be discounted: it is often of significance even if the child appears relatively well.
Certain thing can trigger a wheezing episode in asthma
- Pollen
- Dust
- Featheres
- Fur
- Excercise,
- Viruses
- Chemical
- Smoke
- Traffic
Differential Diagnosis
- Foreign Body
- Pertussis
- Croup
- Pneumonia/TB (Do X-Ray!)
- Aspiration
- Cystic Fibrosis
- Transient infant wheezing
- Sinusitis
- Cardiac failure due to congenital heart disease
- Structural airway abnormality - laryngomalacia, vascular ring
Investigations
- FBC
- Chest X-ray
- Arterial/Venous blood gas (for severe asthma)
- Spirometry
Side note Spirometry
|
Diagnosis
- Clinical History
- Clinical features cough, dyspnoea and wheeze
- Clinical Response to bronchodilator
Aetiology and Pathophysiology
Aetiology
- Genetic predisposition
- Triggers
- Infections à viral (up to 80% of hospital admissions for asthma are following a viral illness)
- Exercise (especially in dry, cold air)
- Allergens (dust mites, pollen, food, animal dander)
- Environment smoking
- Chemicals (salicylates)
Pathophysiology
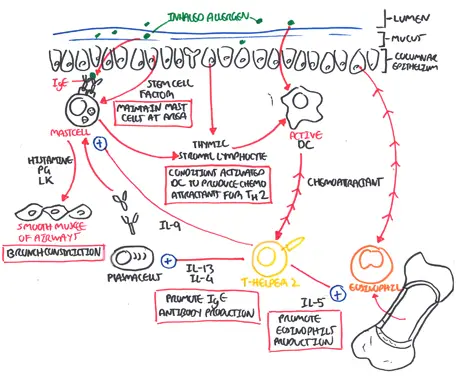
| Watch Asthma Pathophysiology |
Management
Asthma action plan
The essential elements of asthma self-management education are:
- Written information about asthma and individualised patient details
- Self-monitoring of symptoms and/or lung function (spirometry, peak flow)
- A written asthma action plan
- Regular review by doctor, asthma educator, or nurse on medications and current asthma control, reinforcement of trigger avoidance behaviours and lifestyle changes if warranted, feedback to the patient about how well they are controlling their asthma, and how control can be improved
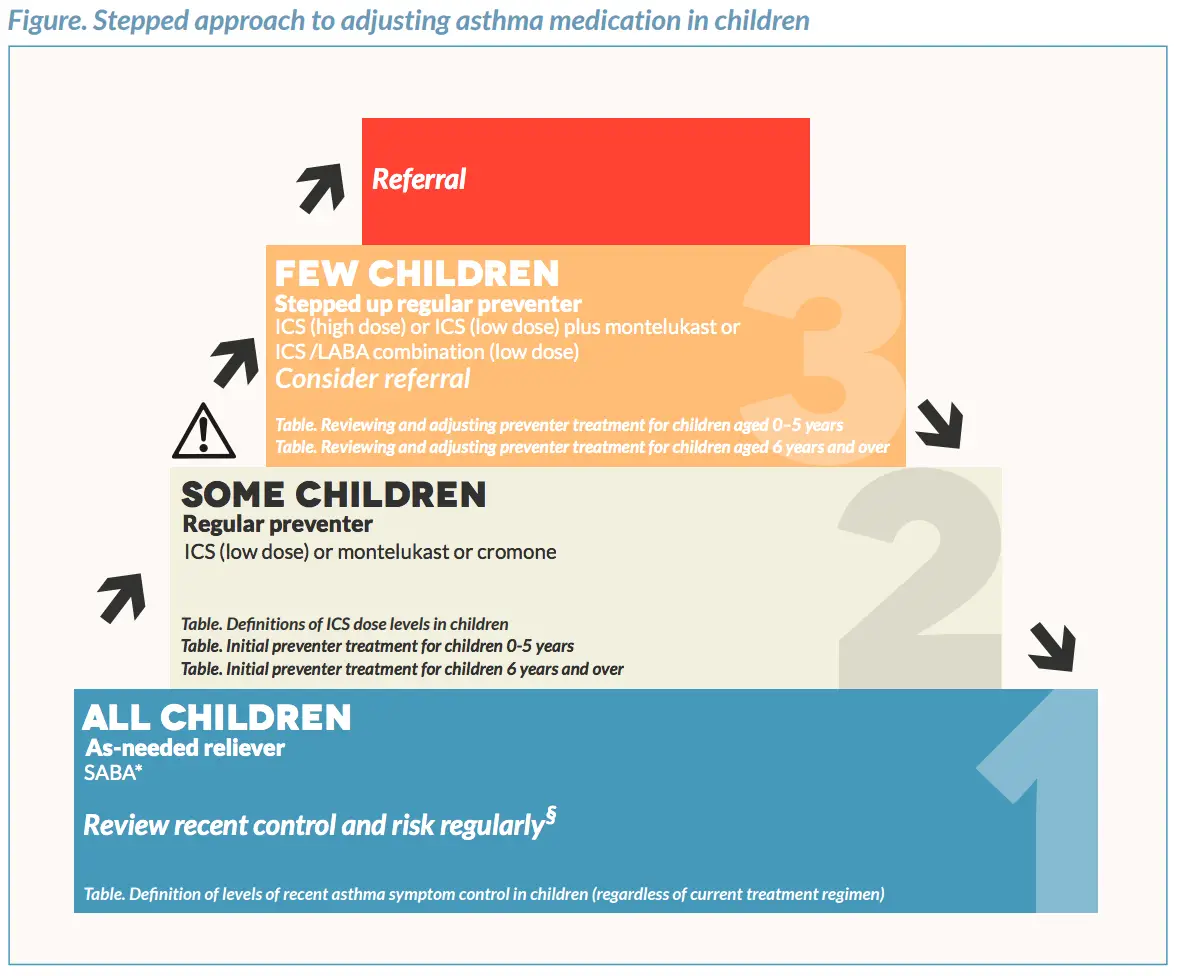
Image from Australian Asthma Handbook
| MEDICATIONS FOR CHILDHOOD ASTHMA | |||
| Medication | Mechanism of Action | Contraindication | Side-effects |
| Short Acting b2-agonist | Sympathomimetic relaxes bronchial smooth muscles by stimulating B2 receptors | Tremors, palpitations, headache. Hyperglycaemia, tachycardia, muscle cramps, lactic acidosis, hypokalaemia | |
| Long Acting b2-agonist | Sympathomimetic relaxes bronchial smooth muscles by stimulating B2 receptors | Tremors, palpitations, headache. Hyperglycaemia, tachycardia, muscle cramps, lactic acidosis, hypokalaemia | |
| Ipratropium bromide | Anticholinergic M3 receptor antagonist – promote bronchodilatation by inhibiting parasympathetic bronchomotor tone | Dry mouth, throat irritation, blurred vision, dizziness, urinary retention, constipation | |
| Theophilines (aminophylline) |
Not understood – thought to have adrenergic effects as well as anti-inflammatory effects | Nausea, vomiting, diarrhoea, GOR, anxiety, tremor, palpitations, seizures, arrhythmias, tachycardia | |
| Corticosteroids | Reduce airway inflammation and bronchial hyper-reactivity | Candidiasis, bruising, facial skin irritation due to nebules, systemic effects (adrenal suppression, bone density loss, glaucoma, skin thinning and bruising, impaired growth) | |
| Magnesium | |||
| Adrenaline | |||
Asthma Emergency
Assessment of and management of Asthma in Emergency
- Acute Mild/moderate asthma
- Acute asthma
- Life-threathening asthma