Overview
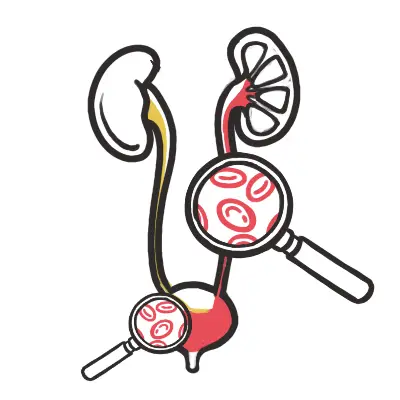
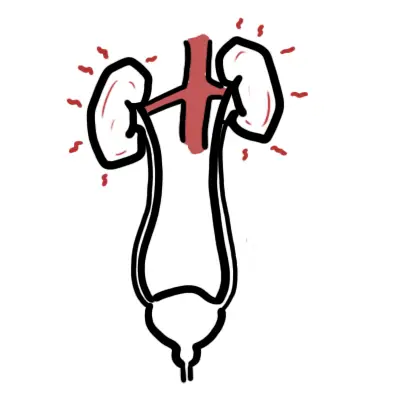
Haematuria is defined as evidence of blood in the urine under microscopy. It is a common symptom of both benign and malignant conditions.
- Haematuria can be microscopic or macroscopic (visible red/brown urine).
- Haematuria can be symptomatic or asymptomatic
- Haematuria can be glomerular or non-glomerular
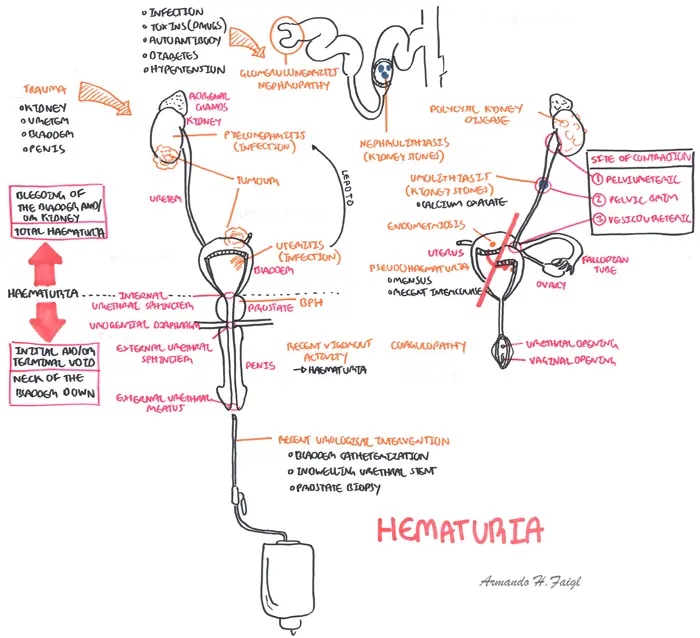
| Common causes | Features |
| UTI | Dysuria, fever, fatigue, nausea/vomiting |
| Nephrolithiasis (Renal stones) | Renal colic, flank pain radiating to back |
| Malignancy | Painless macroscopic haematuria |
| Post interventional | Recent catheterization or other procedures |
| Glomerulonephritis | Depends if nephrotic or nephritis syndrome |
| Vasculitis | Microscopic haematuria, often asymptomatic |
| Remember Transient haematuria: Exercise (‘joggers’ nephritis’), Menstruation, Sexual activity, UTI, Viral illnesses and Trauma. |
| Definition Haemturia: Blood in urine Microcopic (Invisible) haematuria: Macroscopic (Visible) haematuria: Dysuria: Pain while urinating |
Approach
Establish is it symptomatic or asymptomatic, microscopic or macroscopic and is it perhaps glomerular or non-glomerular (look at GFR, renal history)?
- History
- Urinary symptoms
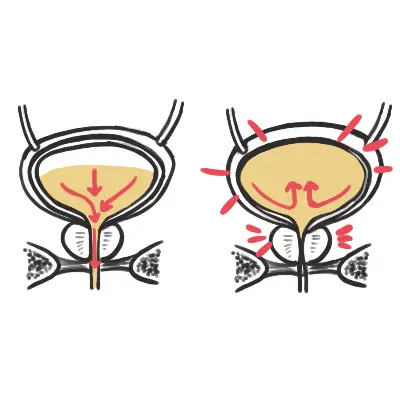
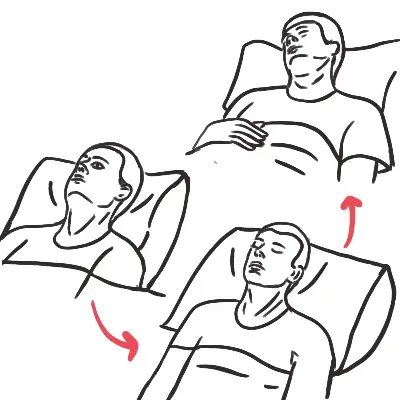
- What part of the stream?
- Throughout - upper urinary tract cause
- Start or finish - lower urinary tract cause
- Risk factors for malignancy
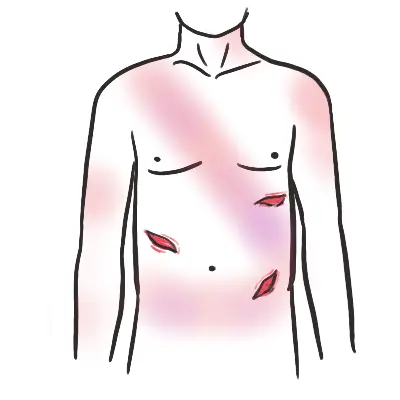
- Examination - Check every system
- Joint inflammation, rash → autoimmune
- Signs of anaemia
- ↑BP and Oedema → glomerular disease
- Flank pain/tenderness → stones, pyelonephritis
- Investigation
- Exclude transient causes
- Urine dipstick
- EUC
| Remember >40 year old presenting with haematuria is bladder malignancy (+/- risk factors) until proven otherwise. |
Investigation
Investigation aims to confirm your diagnosis and or rule out other differential diagnosis. Investigations should help confirm whether it is glomerular or non-glomerular.
- Clinical Examination - Check prostate on PR exam
- PSA?
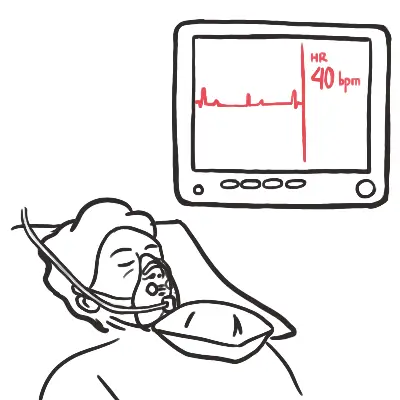
- Full blood count - Infection and Anaemia
- EUC - Kidney function
- eGFR - Glomerular or non-glomerular?
- Urine dipstick
- Urine MCS
- Urine Cytology
- Group and hold - for blood loss incase you need to resuscitate
- Ultrasound Kidney - to identify renal tumours or cysts
- Cystoscopy (gold standard) - Identify bladder tumour and other urinary tract malignancies
- CT scan abdomen - Renal tumour suspected
| Remember Initial investigations for haematuria should include intravenous pyelogram, urine cytology, full blood examination, renal function, and PSA in men. |
Differential Diagnosis
Microscopic invisible haematuria In Australia, microscopic haematuria is defined as >10 red blood cells in high field power on microscopic evaluation. This varies from >3–10 cells depending on British, European or American definitions. Microscopic haematuria should be confirmed by repeating the urine microscopy so that at least two of three tests are positive. Most common causes include UTI, BPH and renal stones. However, 70% of microscopic haematuria causes are unknown, and is thought to be attributed to transient benign physiological conditions, including vigorous physical exercise, sexual intercourse or menstrual contamination.
Assess risk of urological malignancy
| DIFFERENTIAL DIAGNOSIS OF MICROSCOPIC (INVISIBLE) HAEMATURIA | ||
| Condition | History | Examination |
| UTI | Dysuria, fever, fatigue, nausea/vomiting | Fever, suprapubic tenderness |
| Benign prostatic Hyperplasia | Nocturia, polyuria, hesitancy, uregency, double voiding | Enlarged prostate on digital rectal examination, palpable bladder due to urinary retention |
| Nephrolithiasis (Renal stones) | Sudden onset renal colic, flank pain radiating to back, nausea, vomiting | Renal angle tenderness |
| Polycystic Kidney Disease | Family History | Bilateral Kidney enlargement |
| Glomerulonephritis | High Blood pressure, weight gain, oedema, | |
| Menstruation | Cyclical haematuria associated with menstruation | - |
| Prostatitis | Pelvic pain, dysuria | Digital rectal exam - tender prostate |
| Urethral strictures | ||
| Post interventional | Recent catheterization or other procedures | Presence of catheter or urethral stent |
| Trauma (post sex, exercise) | Recent sexual activity, strenuous exercise | - |
| Vasculitis | Microscopic haematuria, often asymptomatic | |
| Rhabdomyolysis | Recent fall/trauma | Myoglobin present not haemoglobin. But myoglobin is still picked up on dipstick |
| Remember 70% of microscopic haematuria causes are unknown. |
| GLOMERULAR DISEASE | |
| Likely | Unlikely |
| Haematuria throughout voiding | Haematuria initial or terminal voiding |
| Proteinuria | Fever, night sweats and sudden weight loss |
| Oedema, oliguria, dark urine | |
| High BP | Blood clots |
| Joint ache, rash | |
| Dysmorphic RBCs and RBC casts | |
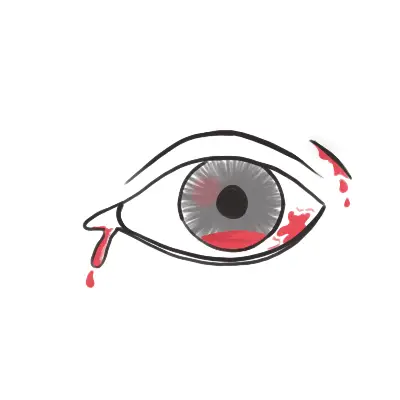
Macroscopic (Visible) Haematuria is more concerning and warrants thorough investigation, as the prevalence of urinary tract carcinomas among patients with macroscopic haematuria are quite high (~5-20%). However, 50% of microscopic haematuria causes are unknown, and is thought to be attributed to transient benign physiological conditions, including vigorous physical exercise, sexual intercourse or menstrual contamination.
Assess risk of urological malignancy
| DIFFERENTIAL DIAGNOSIS OF MACROSCOPIC (VISIBLE) HAEMATURIA | ||
| Condition | History | Examination |
| UTI | Dysuria, fever, fatigue, nausea/vomiting | Fever, suprapubic tenderness |
| Nephrolithiasis (Renal stones) | Sudden onset renal colic, flank pain radiating to back, nausea, vomiting | Renal angle tenderness |
| Benign Prostatic Hyperplasia | Nocturia, polyuria, hesitancy, urgency, double voiding | Enlarged prostate on digital rectal examination, palpable bladder due to urinary retention |
| Bladder Cancer | Painless macroscopic haematuria | - |
| Prostate cancer | Advanced age, weight loss, night sweats, decreased appetite. Urinary symptoms | Abnormal digital rectal examination, prostate nodule or diffuse hardness of the gland |
| Alport's Syndrome (Connective tissue disease) | Hearing impairment, family history of haematuria, hearing loss, or renal disease | Hypertension, oedema, sensorineuronal hearing loss, anterior lenticonus, corneal erosions |
| Post interventional | Recent catheterization or other procedures | Presence of catheter or urethral stent |
Referral
Urologist Referral is recommended in patients presenting with macroscopic haematuria, persistent microscopic haematuria, abnormal urine cytology, irritative lower urinary tract symptoms or recurrent urinary tract infections.
- >40yo
- Risk factors for malignancy
- Macroscopic haematuria
- Upper urinary tract imaging abnormality
- Ultrasound
- CT
- Intravenous urography
- Lower urinary tract assessment abnormality
- Urine Cytology
Nephrologist Referral
- Systemic signs and symptoms
- Glomerular disease suspected?
- Low eGFR
- Abnormal EUC