Overview
Overview Congenital heart disease (CHD) is the most common congenital disorder in newborns.
Classification
- Acyanotic and Cyanotic
- Pulmonary blood flow
- Increased
- Decreased
- Normal
| Cyanotic (T's) | Acynotic (D's) |
| Tetralogy of Fallot | ASD |
| Transposition of the great vessles | VSD |
| Tricuspid atresia | AVSD |
| Truncus arteriosus | Patent Ductus Arteriosus |
| Other: Pulmonary stenosis, Aortic stenosis, Coarctation of the aorta |
Epidemiology
- One-third to three-quarters of children have an innocent murmur noted at some time between age 1 and 14 years, the most frequent of which is an innocent Still's murmur
Clinical Manifestation In infants, feeding difficulties may be the first sign of congestive heart failure
Cardiovascular
- Poor feeding
- Cyanosis/pallor
- Clubbing
- Murmur
- Palpitation
- Dizziness
- Hepatomegaly
Constitutional
- Excessive, unexplained irritability
- Excessive sweating
- Poor weight gain
- Decreased activity or sleeping (easily fatigued)
- Delayed developmental milestones motor
- Poor exercise intolerance
Respiratory
- Chronic cough - pulmonary vascular congestion
- Dyspnoea on exertion
- Wheezing - pulmonary congestion
Differential Diagnosis - innocent murmur's
| Remember The most common innocent murmur is a Still murmur |
- Aortic Systolic murmur
- Still murmur
- Venous hum
Investigations
- ECG
- Arrythmias
- Chest X-ray
- Echocardiogram
- 16-20weeks gestation
- After delivery
- Cardiac catheterization
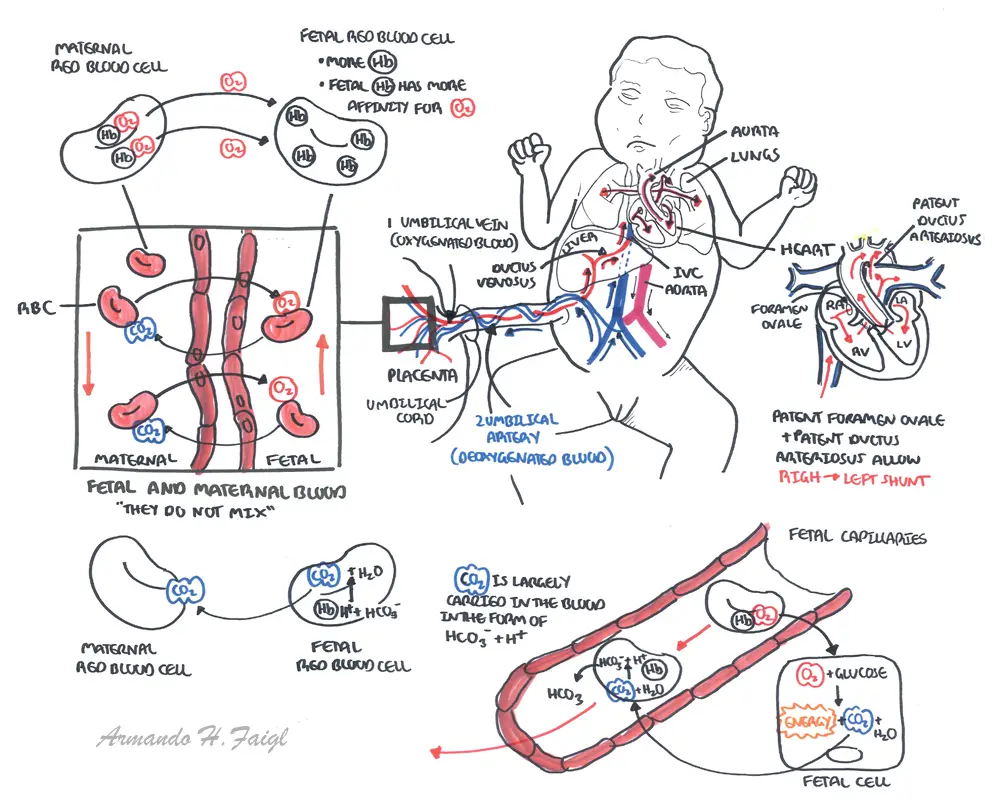
Foetal cardiac anatomy and physiology
Embryology
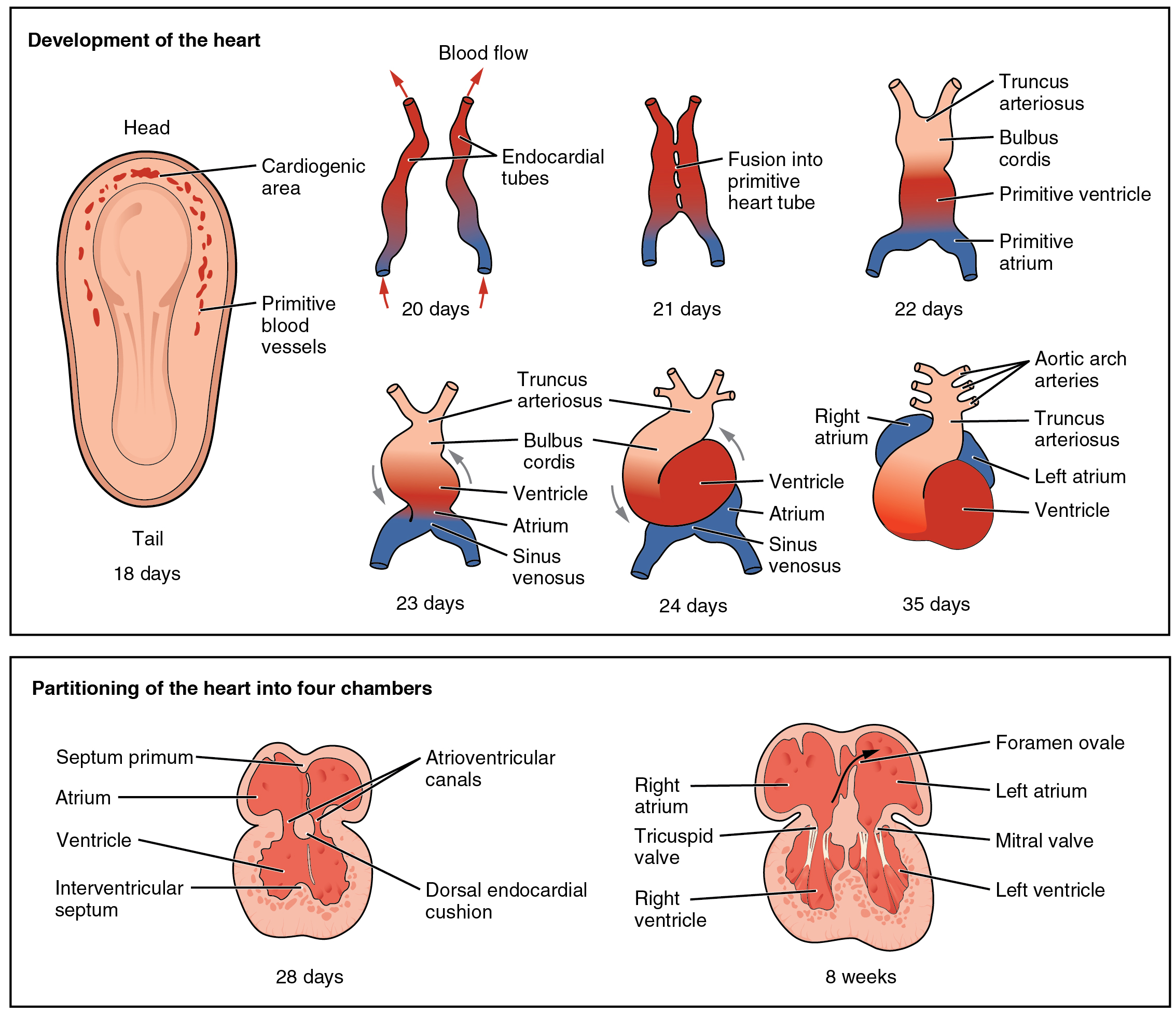
Foetal Circulation
Atrial Septal Defect
Overview
- Left to Right shunt
- Right atrium and right ventricle enlargement
- Patients can present with atrial fibrillation
- Pulmonary hypertension (late stage)
- 4 different types
- Ostium Primum
- Ostium secundum (most common - 75%)
- Unroofed coronary sinus defect
- Sinus venosus defect
- Patent foramen ovale (~20-25% of population)
- Not a true ASD
- Embolic phenomenon (venous origin bypasses lung)
Clinical Presentation
- Child and adult are usually asymptomatic
- Mid-systolic murmur (pulmonary valve)
- Congestive heart failure in large defects
- Adults:
- Mid-systolic murmur (pulmonary valve)
- Palpitations (AF)
- Paradoxical embolus
- Cerebral abscess
Investigations
- Echocardiogram
- location and type of ASD
Pathophysiology
- Pressure normally greater in left side of heart
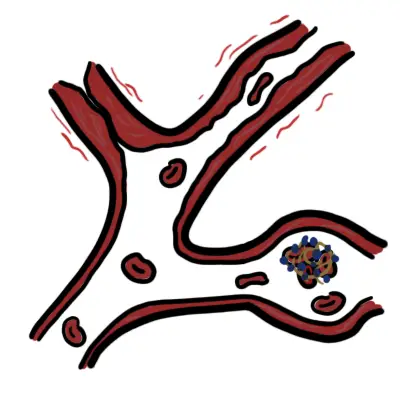
- ASD causes left to right shunt → right atrial hypertrophy → ↑blood flow to right ventricle (right ventricular hypertophy) → ↑pulmonary blood flow
Eisenmenger Syndrome (Cyanosis)
- ↑Pulmonary blood flow from sheer stress/circumferential stretch → Endothelial dysfunction and vascular remodelling → ↑pulmonary vascular resistance (pulmonary hypertension) → ↑pressure on the right side of heart → right to left shunt
| Pulmonary hypertension is present when mean pulmonary artery pressure exceeds 25mm Hg at rest or 30 mm Hg with exercise. ECG findings include: RVH or strain, RAD, p-pulmonale, tall R waves in V1. |
Ventral Septal Defect
Overview Most common congenital heart defect. It occurs in almost 50 percent of all patients with congenital heart disease.
Risk factors
- Family history
- Trisomy 21
- Maternal
- Alcohol
Important features of VSD
- Size of defect - small or large
- Pulmonary vascular resistance
- Location type
| Remember 75% of small defects undergo spontaneous closure within the first two years of life. Moderate VSD may close overtime. Large rarely close and require surgery |
Clinical Presentation
- Small defect - holosystolic murmur
- Moderate large defect over time
- Failure to thrive
- Tachypnoea, dyspnoea
- Feeding difficulties
- Recurrent pulmonary infections
- Endocarditis risk
- Pansystolic murmur (Tricuspid area) - no radiation
- Thrill around Tricuspid area
- Loud P2
- Cardiomegaly
| Causes of Pansystolic mumurs |
| Mitral regurgitation |
| Ventricular septal defect |
| Tricuspid regurgitation |
Pathophysiology of VSD
- Pressure normally greater in left side of heart
- VSD causes left-to-right shunt → ↑pressure in right ventricle → right ventricular hypertophy → ↑pulmonary blood flow
Eisenmenger Syndrome (Cyanosis)
- ↑Pulmonary blood flow from sheer stress/circumferential stretch → Endothelial dysfunction and vascular remodelling → ↑pulmonary vascular resistance (pulmonary hypertension) → ↑pressure on the right side of heart → right to left shunt
Investigations and diagnosis
- Echocardiogram (diagnostic)
- Chest x-ray - changes of left-to-right shunt
Management
- Surveillance (small VSD)
- Cardiologist - echocardiograms/murmur
- Immunizations
- Monitoring of growth parameters
- Monitoring symptoms of heart failure
- Nutritional support - ↑calorie intake
- Medical management - heart failure
- Diuretics
- +/- ionotropes
- Surgical - for symptomatic moderate/large VSD
- Direct patch closure of VSD
Complications
- Endocarditis
- Aortic regurgitation
- Aortic stenosis
- Congestive heart failure
Patent Ductus Arteriosus
Overview Normally ductus arteriosus closes and become ligamentum arteriosus. Patent ductus arteriosss is where the ductus arteriosus persists post partum for more than 3months. Patent ductus arteriosus creates a Left to right shunt. This occurs in 1 in 2000 live births.
Anatomy
The ductus arteriosus closes in approximately 90 percent of full-term neonates by 48 hours of age. Prolonged patency of the ductus arteriosus occurs in premature infants and those born at altitude
Risk Factors
- Maternal rubella
- High altitude (oxygen tension)
- Prematurity
- Female gender
Clinical presentation
- Continous murmur around pulmonary valve
Management
- Spontaneous closure (unlikely after 3 months)
- Pharmacological ductal closure in premature babes: indomethacin/ibuprofen
- Antibiotic prophylaxis for endocarditis risk
- Device/surgical closure
Coarctation of the Aorta
Overview A stricture is present in the aorta which leads to restricted blood flow to the lower part of circulation. BP in head and UL’s is high, whilst that in the LL’s is low. Heart failure may develop Surgical repair is needed in most cases.
Clinical presentation
- Weak femoral and lower limb pulses
- Radial femoral delay
- Bounding pulses in arms and carotids
- Difference in left and right arm blood pressure (suggests subclavian coarctation
- Hypertension
- Pink upper body and cyanotic lower body (paediatrics mainly)
| Remember Coarctation should be suspected in an asymptomatic child with hypertension |
Investigations
- Chest X-ray
- ECG
- Echocardiogram (gold standard)
Management
- Neonates - PGE1
- Surgery for significant coarctation
- Adults - treat heart failure and hypertension, followed by surgery
Complications
- Cerebrovascular disease
- Systemic hypertension
- Endocarditis
- Aortic aneurysms
Stenotic congenital heart defect
Overview Aortic valve is thickened and narrowed leading to
development of abnormally high pressure in LV. LV becomes
hypertrophied. Correction with baloon valvuloplasty or surgery.
Pulmonary stenosis Pulmonary valve is thickened and narrowed leading to development of abnormally high pressure in RV. RV becomes hypertrophied If severe, treated with balloon catheter to dilate narrowing.
Tetralogy of Fallot
Overview The most common cyanotic congenital cardiac defect. In 1888, Etienne-Louis Arthur Fallot described four cyanotic patients with four similar anatomic features
4 anatomical features
- Right ventricular hypertrophy
- Pulmonary stenosis
- Ventral septal defect
- Aorta overriding the ventricular septum
| Side Note there are a number of associated anatomical features associated with TOF including right aortic arch, left anterior descending from the right coronary artery, patent ductus arteriosus. |
Pathophysiology
- Largely dependant on right ventricular outflow obstruction
- VSD → Aortic arch overriding the defect (aorta now pointing more to the right then left allowing blood from right ventricle to enter) → Left to right shunt (acynotic)
- Left to right shunt→ Right ventricular hypertrophy → ↑pulmonary pressure causing pulmonary valve stenosis → ↑Right ventricular hypertrophy → Right to left shunt (cynotic)
- "Tet spells" - Periods of increased oxygen demand/ultilisatio. Near occlusion of the right ventricular outflow tract with profound cyanosis.
| Side note Children with cyanotic congential heart disease often squat. This kinks the femoral artery increasing peripheral resistance. This in turn increases left-sided ventricular resistance which lessens the burden of right-eft shunt. |
Clinical presentation - depends on degree of right ventricular outflow obstruction
- May be asymptomatic until hypercyanotic (tet) spells.
- Hypercapneia
- Agitation
Clinical Examination
- Cyanosis
- Harsh ejection systolic murmur (Pulmonary valve) stenosis)
- Systolic thrill (Pulmonary valve)
- Holosystolic murmur (Tricuspid area from ventricle septal defect)
- Clubbing of nail beds
Diagnosis
- Echocardiogram with dopller
- ECG
- Right ventricular hypertrophy
| Remember ECG findings of right ventricular hypertrophy include: p-pulmonale (Right atrium), tall R waves in V1, upright T wave in V1 and marked right axis deviation |
- Chest X-ray - Boot shaped heart, unturned apex and a concave main pulmonary artery segment
- Cardiac catheterisation to further delineate structural abnormalities.
Management - surgical
- VSD closure with patch
- Enlargement of pulmonary artery
- Palliative procedure for symptom relief
- Shunts - subclavian artery to the ipsilateral pulmonary artery
Tricuspid atresia
Transposition of the great arteries
Eisenmenger Syndrome
Overview Eisenmenger syndrome is the triad of congenital systemic-to-pulmonary cardiovascular communication, pulmonary arterial disease causing severe pulmonary hypertension, and cyanosis
Diagnosis
- Presence of congenital heart disease
- Exclusion of other causes of pulmonary hypertension
Clinical findings
- Congenital heart defect
- Central cyanosis
- Digital clubbing