Overview
Overview The diagnosis of COPD is usually limited to individuals who have chronic airflow obstruction associated with tobacco smoke or some other noxious inhalant, and it is usually not difficult to distinguish it from other causes of chronic airflow obstruction. The most commonly associated clinical disorders associated with COPD are emphysema and chronic bronchitis.
| Definitions Chronic Obstructive Lung Disease: A serious, progressive and disabling condition that limits airflow in the lungs. It includes emphysema and chronic bronchitis. Strongly associated with smoking Interstitial Lung Disease: Includes a diverse group of respiratory conditions characterised by inflammation and fibrosis of the interstitium. Worsening hypoxia and respiratory failure may develop with disease progression. The disease is considered a restrictive lung disease Restrictive Lung Disease: Unable to fully fill the lungs with air. Their lungs are restricted from fully expanding. |

Summary of Chronic Obstruction Pulmonary Disease (COPD) COPD is a progressive lung disease characterised by dyspnoea, wheezing, chest tightness and cough. COPD is an umbrella term for a number of lung disease, two common types being emphysema and chronic bronchitis. Smoking, air pollution and certain occupations are risk factors. COPD is an obstructive disorder and so the use of bronchodilator can alleviate symptoms and improve lung function.
Risk Factors
- Smoking
- Air-pollution
- α1-antitrypsin deficiency
Signs and Symptoms
COPD results from an increase in the rate of decline in lung function over time.
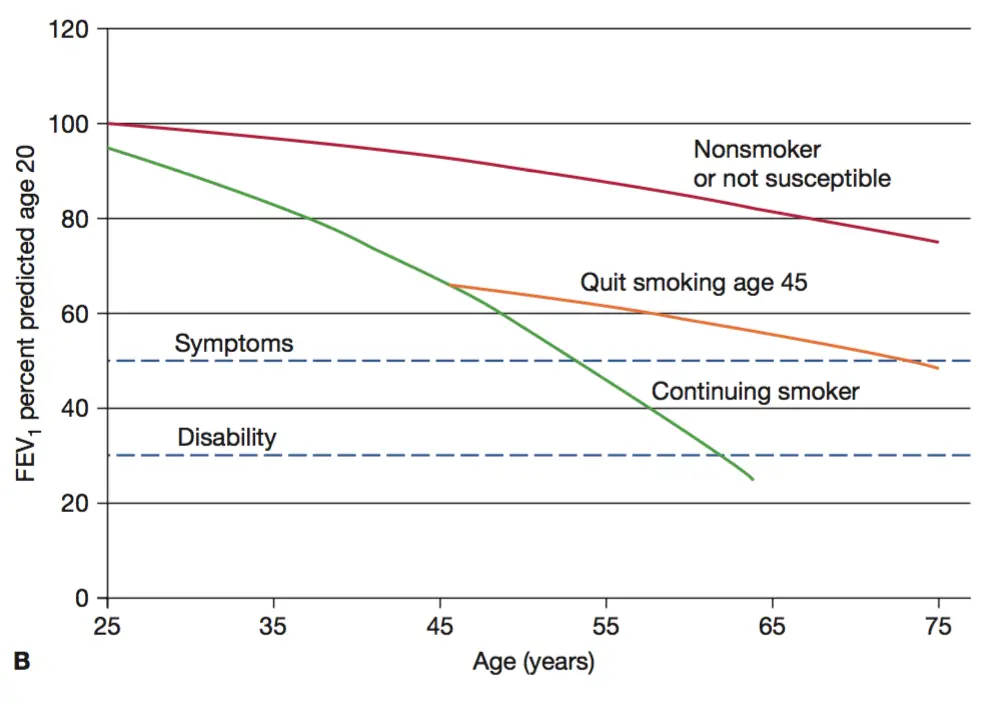
Natural history of the decline in FEV1 overtime. Comparing a hypothetical non-smoker, smoker and ex-smoker. Quitting smoking can slow progression to COPD by 50%.
| Cardinal Triad of COPD: (exertional) Dyspnoea, Chronic cough and sputum production |
Clinical Presentation
- Chronic dyspnea
- Chronic cough
- Sputum production
- Wheezing
- Chest tightness
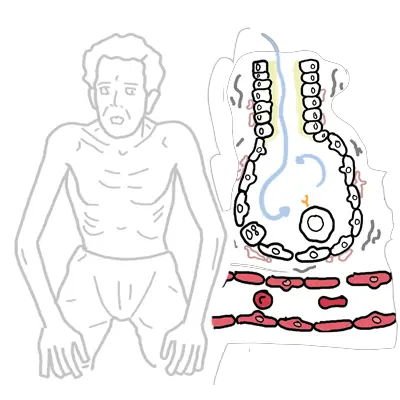
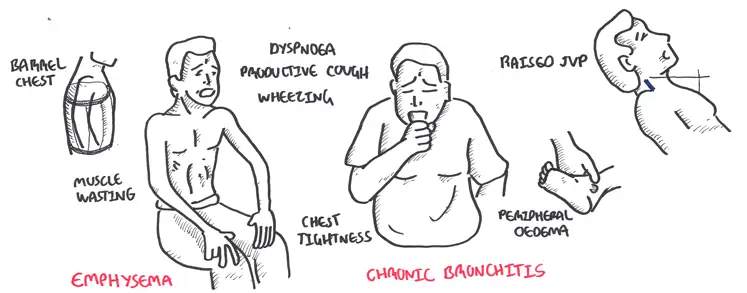
Clinical Examination - Pure emphysema (pink puffers)
- Muscle wasting
- Pursed lips
- Barrel chest
Clinical Examination - Pure chronic bronchitis (blue bloaters)
- Cyanosis (hypoventilate)
- Overweight/obese due to inactivity
- Right-sided heart failure (ie. increased JCP, peripheral oedema)
Differential Diagnosis
| COMMON CAUSES OF CHRONIC COUGH |
| COPD |
| Asthma |
| GORD |
| Post nasal drip |
| COMMON CAUSES OF CHRONIC DYSPNOEA | |
| Respiratory Disease | Cardiovascular Disease |
| COPD | Myocardial Dysfunction (Heart Failure) |
| Asthma | Obesity/de-conditioning |
| Interstitial lung disease | |
Investigations
- Lung Function Test - Spirometry
- Chest X-Ray
- Full blood count
- ABG
- Serum α-antitrypsin
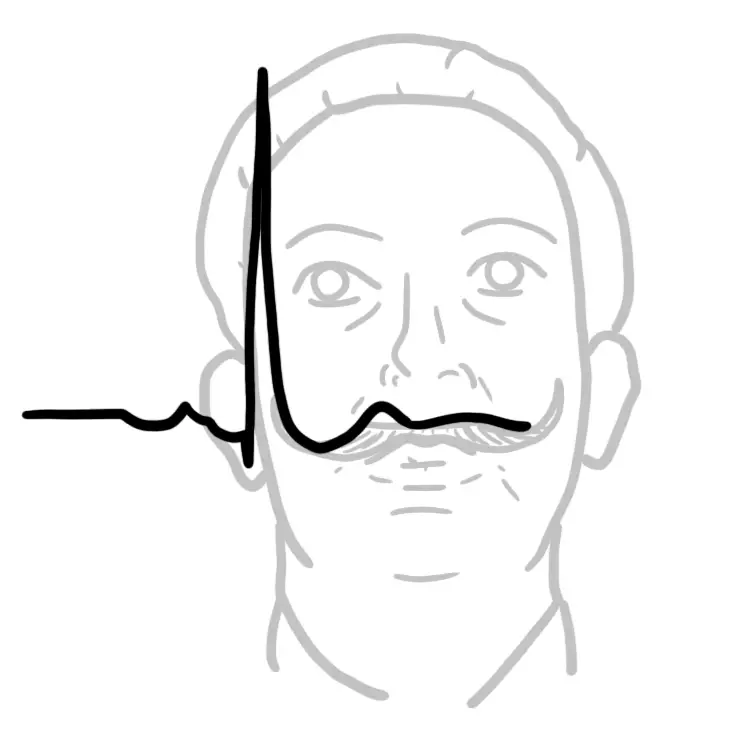
- ECG
- Echocardiogram
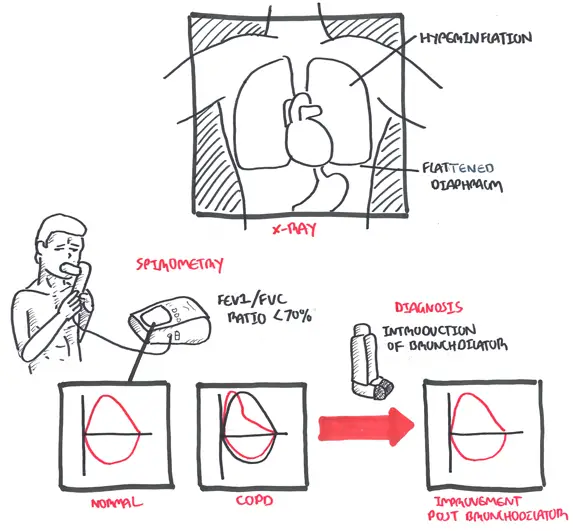
Investigations Chest X-ray (CXR) is essential in ruling out differentials and help confirm COPD. A CXR may reveal hyperinflation and a flattened diaphragm. Spirometry is for diagnosing and monitoring disease. COPD is diagnosed when FEV1/FVC ratio is below 70% and improves with introduction of a bronchodilator.
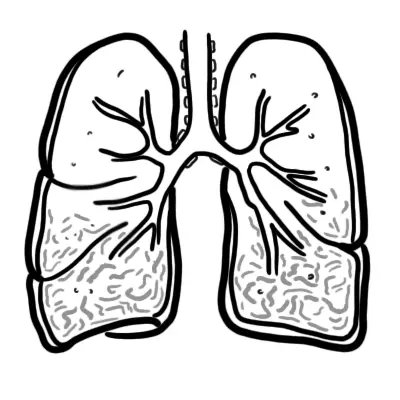
| Emphysema | Chronic Bronchitis |
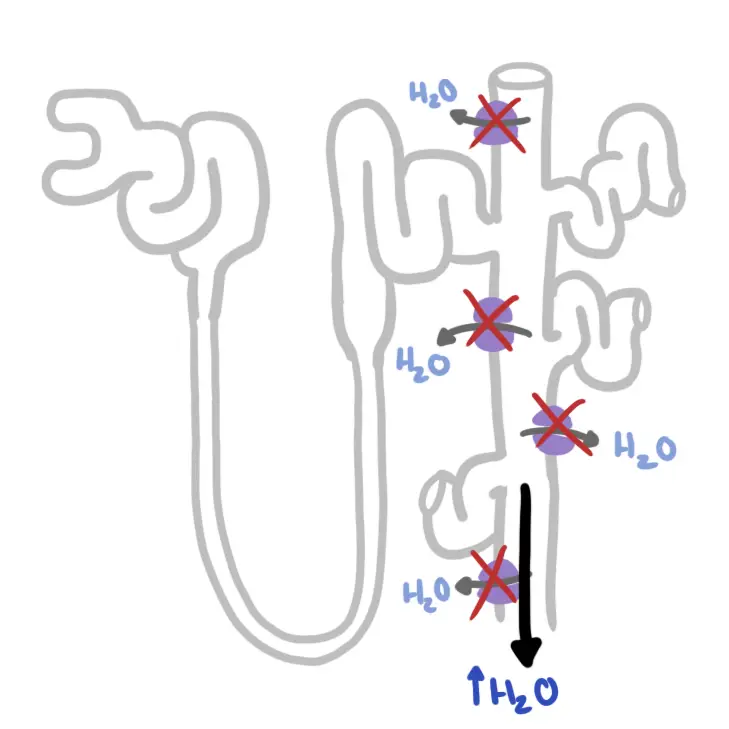
| Defined Pathologically Dilation and destruction of air spaces distal to the terminal bronchiole without obvious fibrosis. Decreased elastic recoil of alveoli causing decreased expiratory driving pressure, airway collapse and air trapping. |
Defined Clinically Productive cough on most days for at least 3 consecutive months in 2 successive years. Obstruction is due to narrowing of the airway lumen by mucosal thickening and excess mucus |
Severity
| COPD Severity is based on FEV1 (COPD is diagnosed by FEV1/FVC) |
| Mild FEV1 <.7 |
| Moderate FEV1 0.5-0.3 |
| Severe FEV1 <0.3 |
| MRC Dyspnea score | |
| 1 | Not troubled by breathlessness except on streous exercise |
| 2 | Dyspnea when hurrying or walking up a slight hill |
| 3 | Walks slower than contemprorores on level ground due to dyspnea, or has to stop for breath when talking at own pace |
| 4 | Stops for breath after walking 100m or less on ground level |
| 5 | Too breathlesss to leave house, or when getting dressed |
Pathology
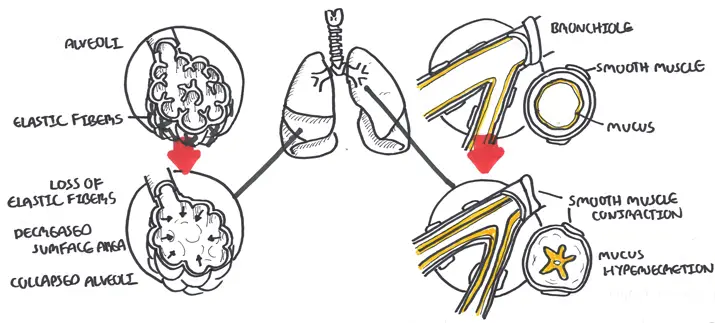
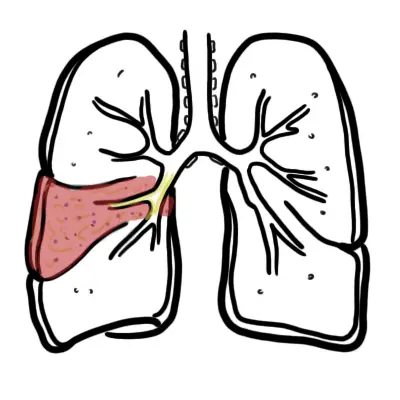
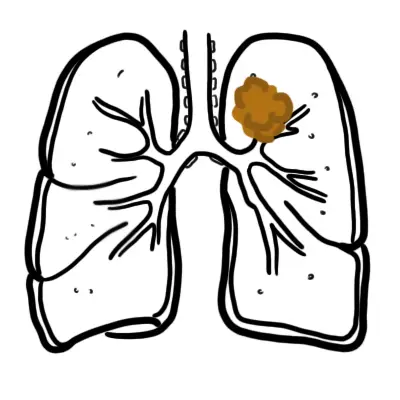
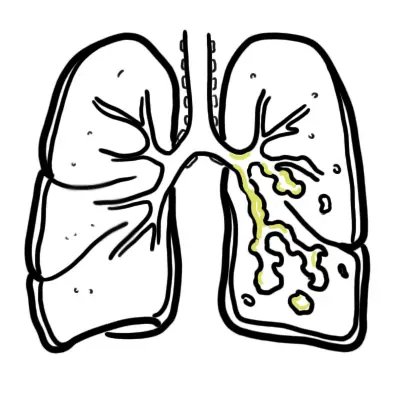
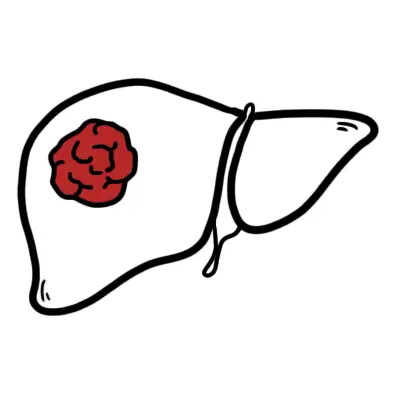
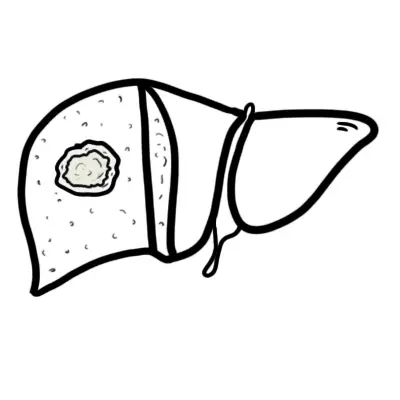
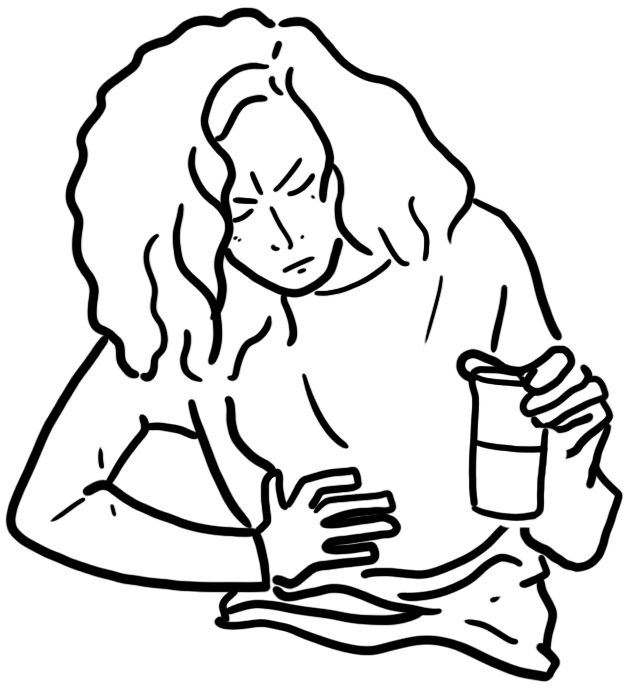
Left Image Pure emphysema effects the alveoli causing destruction of elastic fibers, decreasing surface area resulting in air trapping. Right Image Pure chronic bronchitis affects the respiratory tract leading to goblet cell proliferation, mucus hypersecretion and smooth muscle hypertrophy. However, typically people present with a mixture of emphysema and chronic bronchitis.
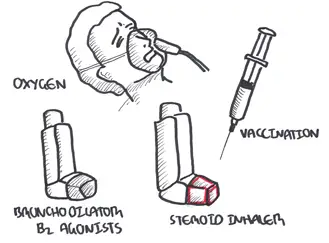
Management
- Patient education and vaccination
- Smoking cessation
- Pulmonary rehabilitation
- Short acting bronchodilators
- Beta 2 agonists
- Muscarinic 3 antagonists
- Long acting bronchodilators
- Inhaled corticosteroids
- Oxygen therapy
| Remember Smoking cessation and supplemental oxygen to treat chronic hypoxemia are the only medical therapies shown to decrease mortality among persons with chronic obstructive pulmonary disease. |
| Remember to step down therapy to lowest doses which control symptoms |
What are the 5 “A’s” of smoking cessation counseling?
|
Emergency (acute exacerbations) sustained (>24-48 h) worsening of dyspnea, cough, or sputum production leading to an increased use of medications
- Bronchodilators
- Short acting beta 2 agonists (w/ spacer)
- Short acting muscarinic antagonists (nebulizer)
- Oral corticosteroids (3-5 days) or IV hydrocortisone
- Eventually transition to inhaled corticosteroids
- Antibiotic if purulent sputum
- Oxygen therapy if needed
Complications and Prognosis
Complications
- Polycythemia 2° to hypoxemia
- Chronic hypoxemia
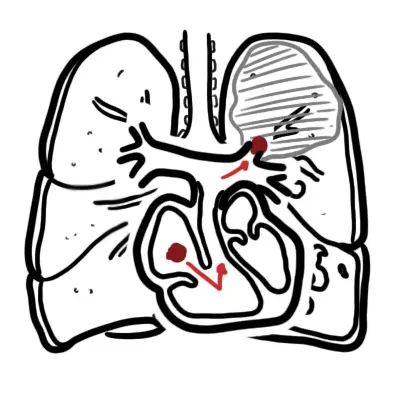
- Pulmonary hypertension
- Cor pulmonale
- Pneumothorax due to rupture of emphysematous bullae
- COPD exacerbation
Prognosis
- Level of dyspnea is the single best predictor
- 5 yr survival
- FEV1 <1 L = 50%
- FEV1 <0.75 L = 33%
α1-antitrypsin deficiency
Overview α1-antitrypsin deficiency
| Conditions suggesting a1- Antitrypsin Deficiency |
| Early onset |
| Non-smoker |
| Emphysema predominantly in lung bases (paracinar) |
| Necrotising panniculiitis |
| Family history |
| Bronchiectasis without other etiology |
Restrictive vs. Obstructive
| Remember The hallmark of restrictive lung disease is decreased lung capacities, particularly the TLC but also the vital capacity. |
| Remember In both obstructive and restrictive lung disease, the FEV1 is decreased, the FEV1 /FVC is decreased in obstructive processes and normal in restrictive processes. |
References
- UpToDate
- Best Practice
- Toronto Essential Notes
- Case files