Overview
Overview Sleep apnea syndrome is an extremely common medical disorder associated with important morbidity. Sleep Apnea and can be classified as:
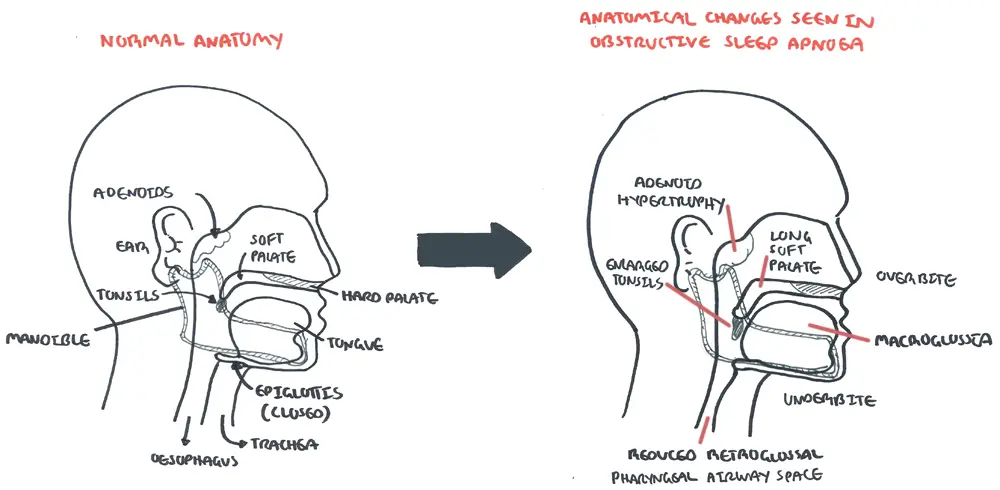
- Obstructive Sleep Apnea - is the most common, characterized by repetitive, intermittent collapse of the upper (pharyngeal) airway during sleep, which causes apnoeic episodes terminated by partial arousal
- Central Sleep Apnea - characterised by repetitive absent or diminished respiratory efforts that occur intermittently or in a cyclical pattern predominantly during sleep.
- Mixed Sleep Apnea - events initially appear central in origin, with respiratory effort occurring during the latter portion of the same episode.
| Definition Apnea:an episode of breathing cessation lasting at least 10 seconds in duration Hypopnoea: ≥10 second 50% reduction in breathing |
This page will mainly focus on Obstructive Sleep Apnoea
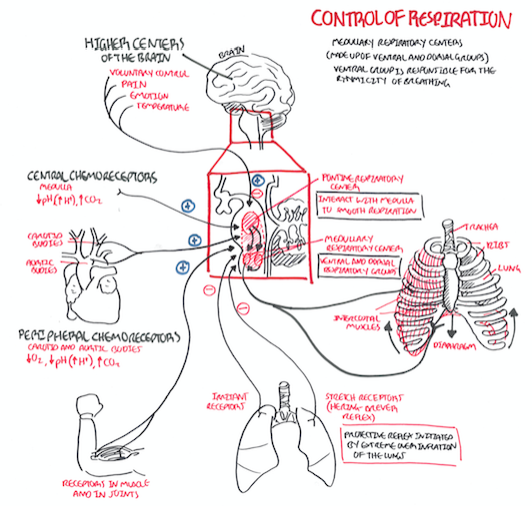
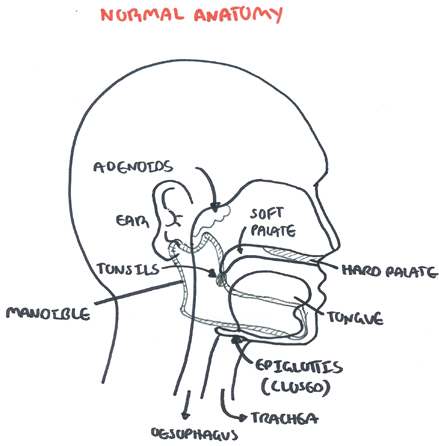
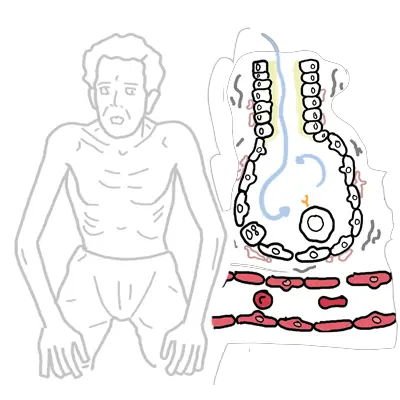
Respiratory Anatomy and Physiology
Risk Factors
- Male – doubles the risk, probably due to a testosterone effect on the upper airway
- Obesity - pharyngeal fat deposits tend to narrow the pharynx
- Craniofacial & upper airway abnormalities:
- Large neck circumference
- Maxillomandibular abnormalities
- Increased volume of soft tissues (including tonsils, adenoids & tongue)
Other risk factors
- Acromegaly & hypothyroidism
- Familial link
- Alcohol & sedatives – relaxing the upper airway dilating muscles
- Post-menopause (women)
- Polycystic ovary syndrome – combination of high levels of androgenic hormones & obesity increases risk of OSA by 30 fold.
Signs and Symptoms
- Excessive daytime sleepiness/somnolence
- Snoring
- Poor sleep quality
- Morning headaches
- ↓ libido
- ↓cognitive performance
Examination
- Overweight or obese
- Large neck circumference (≥40cm)
- Hypertension (50% of cases)
Differential Diagnosis
- Inadequate time in bed
- Shift work
- Excessive caffeine intake
- Physical illness
- Periodic limb movement disorder
- Narcolepsy
- Drugs
- Depression
Investigation
- Polysomnography (gold standard for diagnostic)
- Home sleep apnea testing (this is unattended)
Diagnosis The diagnosis of Obstructive Sleep Apnoea is based upon the presence or absence of related symptoms & the frequency of respiratory events during sleep (apneoas, hypopnoeas & respiratory effort related arousals) as measured by polysomnography or home sleep apnoea testing.
Severity
Severity Currently, the apnea–hypopnea index (AHI, number of apneas and hypopneas per hour of sleep) is the standard metric used to describe the severity of sleep apnea
| Mild | Moderate | Severe |
| 5-15 apnoeic episodes | 15-30 apnoeic episodes | >30 apnoeic episodes |
| Relatively asymptomatic | Aware of daytime sleepiness & take steps to avoid falling asleep at inappropriate times | Daytime sleepiness that interferes with normal activities. |
Management
Obstructive Sleep Apnoea Management
- Patient education
- Weight loss
- Change sleep position
- Alcohol avoidance
- Avoid certain medications (Benzodiazepines)
Medical Interventions
- Positive airway pressure (BPAP or CPAP)
- Oral appliances
| Side note Adherence: Estimated that 20-40% of patients do not use their positive airway pressure device & many others do not used it all night, every night |
Surgical therapy
- Tonsillectomy
- Uvulopalatopharyngoplasty
Pharmacology Patients continuing to have excessive daytime sleepiness despite adequate OSA-specific therapy may benefit from adjunctive pharmacologic therapy to stimulate respiratory drive:
- Theophylline
- Acetazolamide
| Pharmacology Theophylline, an xanthine derivative chemically similar to caffeine and theobromine, is used to treat asthma and bronchospasm. Theophylline relaxes the smooth muscle of the bronchial airways and pulmonary blood vessels and reduces airway responsiveness to histamine, methacholine, adenosine, and allergen. Theophylline competitively inhibits type III and type IV phosphodiesterase (PDE), the enzyme responsible for breaking down cyclic AMP in smooth muscle cells, possibly resulting in bronchodilation. Theophylline also binds to the adenosine A2B receptor and blocks adenosine mediated bronchoconstriction. In inflammatory states, theophylline activates histone deacetylase to prevent transcription of inflammatory genes that require the acetylation of histones for transcription to begin. Side effects: Nausea/vomiting, stomach/abdominal pain, headache, trouble sleeping, diarrhea, irritability, restlessness, nervousness, shaking, or increased urination. |
Central sleep apnoea: (ranked in order of treatment line)
Without Cheyne-Stokes breathing:
- CPAP or ASV
- Supplemental oxygen
- Acetazolamide or zolpidem (for idiopathic/ primary CSA)
With Cheyne-Stokes breathing:
- Optimise underlying medical condition
- CPAP
- Oxygen therapy
- Non-invasive positive pressure ventilation (NIPPV)
- Cardiac resynchronization therapy or acetazolamide or theophylline
| Cheyne-Stokes breathing is a disorder characterised by recurrent central apnoeas during sleep alternating with a crescendo-decrescendo pattern of tidal volume. It is often observed in patients with congestive heart failure and severe sleep apnoea |
| Pharmacology Acetazolamide is a reversible inhibitor of the carbonic anhydrase enzyme that results in reduction of hydrogen ion secretion at the renal tubule and an increased renal excretion of sodium, potassium, bicarbonate, and water. It can be used as a diuretic or to treat glaucoma as it prevents excessive build up of aqueous humor. It also inhibits carbonic anhydrase in the central nervous system to minimize abnormal and excessive discharge from CNS neurons. Acetazolamide can be administered to patients with a metabolic alkalosis to promote retention of hydrogen ions at the level of the renal tubule. Side effects: dizziness, lightheadedness, polyuria, blurred vision, dry mouth, drowsiness, loss of appetite, stomach upset, headache, fatigue, tinnitus. |
Complications and Prognosis
Complications
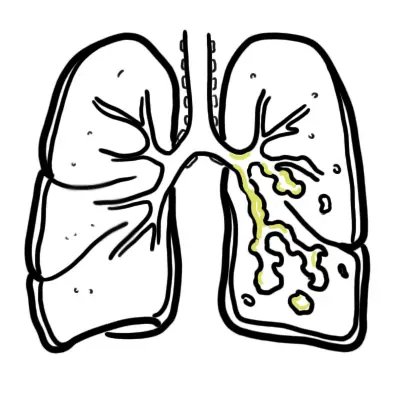
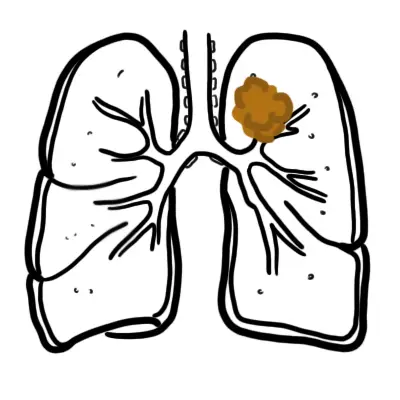
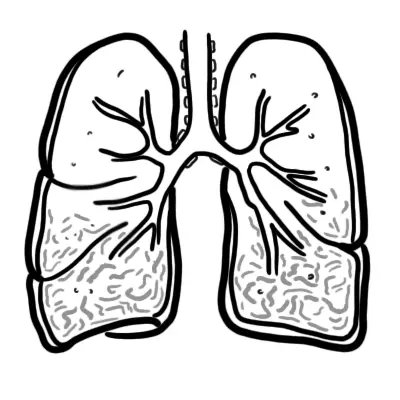
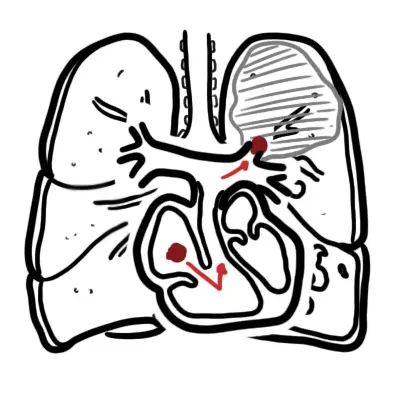
- Pulmonary hypertension
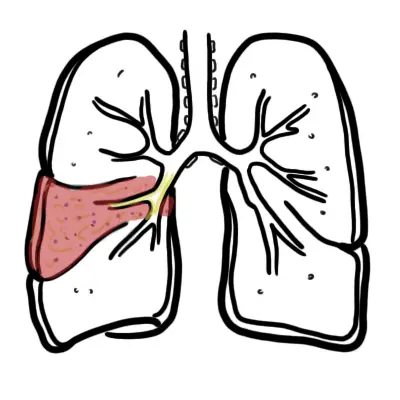
- Type II respiratory failure
- Hypertension
- ↑ Risk of cardiovascular diseases including heart failure
- Depression
- Cognitive dysfunction
- Impaired glucose metabolism
- Pregnancy hypertensive complications
| Type II respiratory failure is where you have ↑CO2 and ↓O2. Initial treatment is thus BiPAP) |
Prognosis Patients efficiently treated may report improvements in alertness and some improvement in quality of life, mood, and cognitive function. Mortality and morbidity from cardiovascular disease is also reduced. Risk of motor vehicle accidents seems to be lower in treated versus untreated patients.