Overview
Pericarditis is the most common form of pericardial disease and a relatively common cause of chest pain. The etiology of pericarditis may be infectious (eg, viral and bacterial) or noninfectious (eg, systemic inflammatory diseases, cancer, and post-cardiac injury syndromes). Tuberculosis is a major cause of pericarditis in developing countries but accounts for less than 5% of cases in developed countries, where idiopathic, presumed viral causes are responsible for 80% to 90% of cases. The diagnosis is based on clinical criteria including chest pain, a pericardial rub, electrocardiographic changes, and pericardial effusion.
| Video: Pericarditis Overview |
| Definition Acute pericarditis: An inflammation of the pericardial sac surrounding the heart. Pericardial friction rub: Harsh, high-pitched, scratchy sound, with variable intensity, usually best heard at the left sternal border by auscultation, due to pericarditis. Pericardial Effusion: Fluid that fills the pericardial space, which may be due to infection, haemorrhage, or malignancy. A rapidly accumulating effusion may lead to cardiac compromise. Cardiac Tamponade: Increased pressure within the pericardial space caused by an accumulating effusion, which compresses the heart and impedes diastolic filling. |
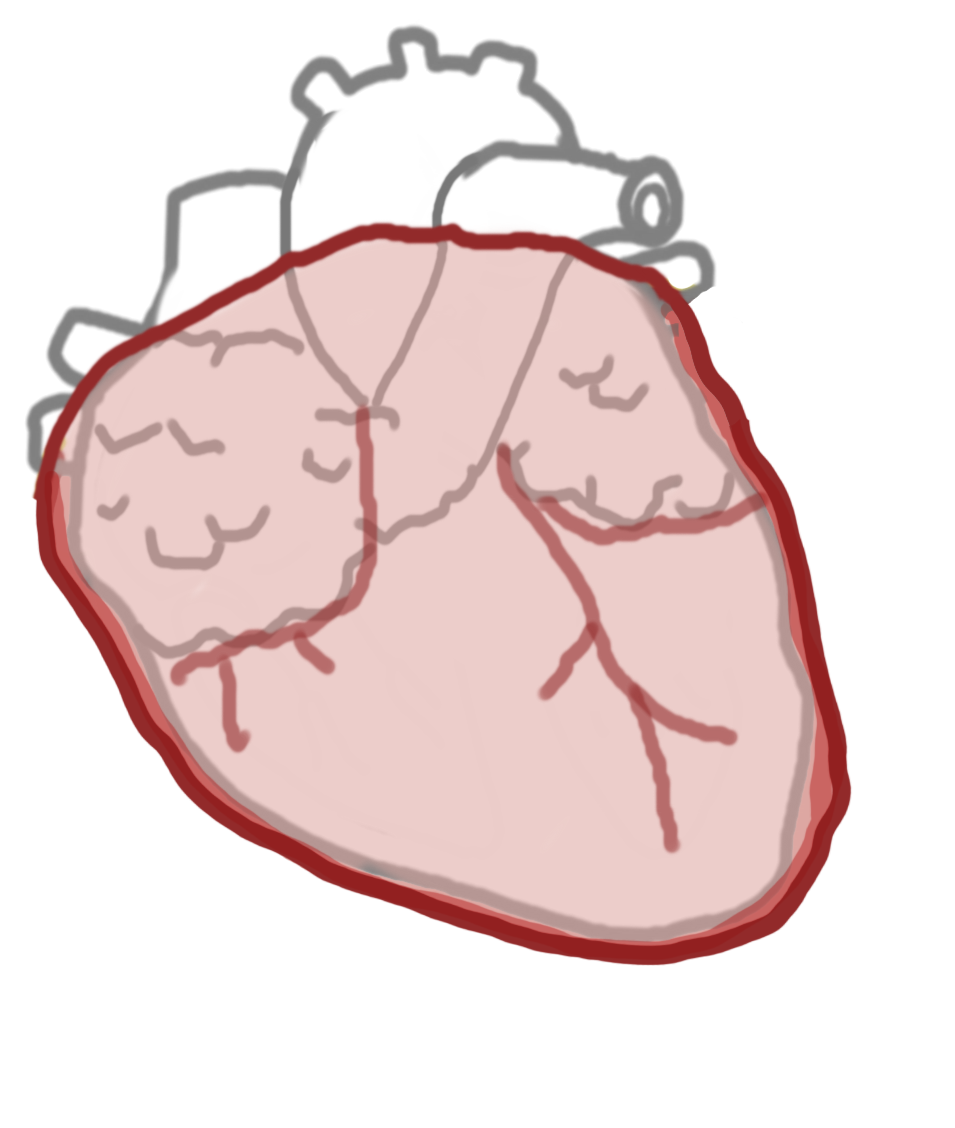
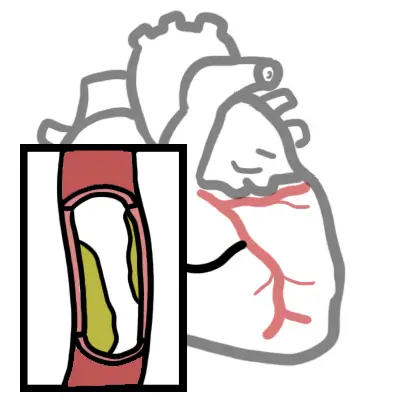
Anatomy of the Pericardium
The pericardium is a membranous layer that covers the heart and helps protect it, fixes the heart in the mediastinum and lubricates the heart.
The pericardium has two layers:
- Serous layer
- Fibrous layer
The pericardium has two layers:
- The serous pericardium has a parietal and visceral layer and forms a closed sac
- The parietal layer lines the inner surface of the fibrous pericardium and is reflected onto the heart as the visceral layer, or epicardium
- Between the parietal and visceral pericardium is the pericardial space which contains serous fluid, important in
- The fibrous pericardium is the outermost layer, and it is firmly bound to the central tendon of the diaphragm.
Risk Factors
| Remember Patients with systemic autoimmune disease can have multiorgan involvement, such as pericarditis, nephritis, pleuritis, arthritis, and skin disorders. |
Signs and Symptoms
- Fever and malaise
- Sharp retrosternal or left-sided chest pain.
- The pain is often eased by leaning forward and is worse in the supine position
- "pericardial rub" -friction rub on auscultation, often transient -
- Tachycardia
| Remember Acute Pericarditis triad: chest pain, friction rub and ECG changes |
Pericarditis causing pericardial effusion can show
- Signs of right sided heart failure - ↑JVP, peripheral oedema
- Paradoxical pulse (systolic blood pressure decreases by more than 10 mm Hg during inspiration)
Differential Diagnosis
Remember to differentiate pericarditis from other life-threatening causes of chest pain, including acute coronary syndrome, myocarditis or pulmonary thromboembolism
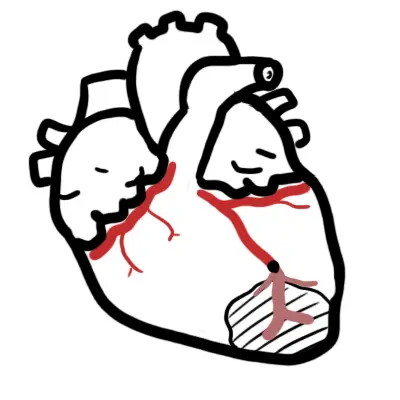
- Myocardial Infarction (Acute Coronary Syndrome)
- Pulmonary Embolism
- Pneumonia
- Pneumothorax
- Costochondritis
Investigations
| Remember Prompt echocardiography may be required to determine the presence and amount of pericardial fluid. |
- FBC
- EUC
- LFT
- X-ray
- Echocardiogram
- Troponin and other cardiac markers
| PERICARDITIS VS MYOCARDIAL INFARCTION | ||
| ECG | Acute pericarditis | Acute MI |
| ST-segment elevation | Diffuse in limb leads V2-V6 | Depending on area of infarction (inferior, anterior or lateral) |
| PR-segment depression | Present | Absent |
| QRS complex changes | Absent | Loss of R-wave and development of Q-wave |
Management
- NSAIDs + PPIs help relieve symptoms
- Colchicine and steroids are also used for as adjuncts and for more serious cases
- For resistant recurrent pericarditis, seek specialist advice.
In symptomatic pericardial effusion and cardiac tamponade cardiocentesis is performed.
Complications and Prognosis
| Remember Constrictive pericarditis and pericardial effusion can mimic heart failure but both of these can themselves be differentiated |
| Constrictive Pericarditis | Cardiac Tamponade | Heart failure | |
| Kusmaul's sign | Present | Absent | Absent |
| Pulsus paradoxus | Uncommon | Present | Absent |
| Jugular Venous Pressure (JVP) | Increased | Increased | Increased |
| Percardial Knock (third heart sound, due to rapid ventricular filling's being abruptly halted by the restricting pericardium) | Present | Absent | Absent |
| Hypotension | Variable | Severe | Variable |
| Remember Kusmaul's sign looks at JVP relationship with breathing. This is different to Kusmaul breathing which is air hunger, rapid deep breathing a sign of metabolic acidosis |
| Remember Constrictive pericarditis may show calcifications of the pericardium on chest x-ray or thickened pericardium on echocardiography. Definitive therapy is resection of the pericardium |
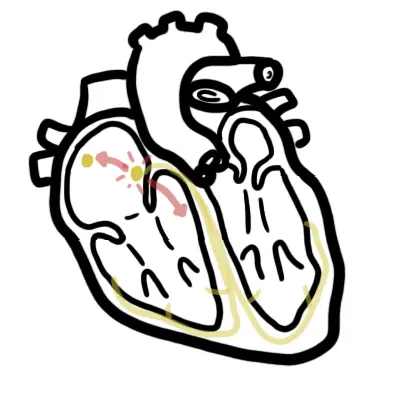
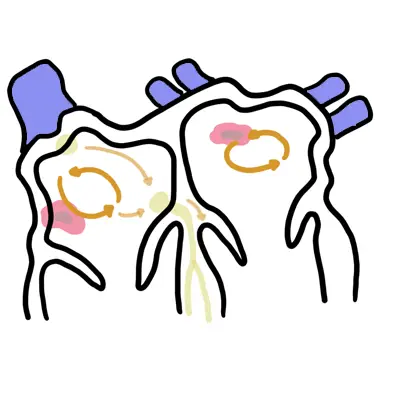
Cardiac Tamponade
| Classical Quatret of Tamponade: hypotension, increased JVP, tachycardia, pulsus paradoxus |
Pathophysiology high intra-pericardial pressure → decreased venous return → decreased diastolic ventricular filling → decreased CO → hypotension and venous congestion Investigation
- ECG
- Echocardiogram
- Cardiac catheterization
Managment
- Pericardiocentesis – ultrasound guided
- Pericardiotomy
- Avoid diuretics and vasodilators (these decrease venous return to already under filled RV-> decrease LV preload -> decrease CO)
- IV fluid may increase CO
- Treat underlying cause