Overview
Overview Haemorrhoid Plexi are normal anatomical structures. However if they enlarge they can cause discomfort and pain. There are internal and external haemorrhoids. Internal are usually asymptomatic whereas external are often painful. The most common complications of hemorrhoids are heavy bleeding, chronic unremitting prolapse of mucosal tissue, strangulation, ulceration, and thrombosis.
| Definition Haemorrhoid plexus: venous drainage of the anal canal being at the haemorrhoid plexi. There is an internal and external haemorroid plexus. Dilatation of a haemorrhoid plexus causes haemorrhoids. Haemorrhoids: collections of submucosal, fibrovascular, arteriovenous sinusoids that are part of the normal anorectum |
| Video: Haemorrhoids Overview |
Anorectal Anatomy
Overview The hindgut makes up the last 1/3 of the transverse colon, the descending colon, sigmoid colon, rectum and part of the anus. The anal canal commences at the level where the rectum passes through the pelvic diaphragm and ends at the anal verge.
Layers of the rectum mucosa (from inner to outer)
- Mucosa
- Submucosa
- Muscularis
- Outer longitudinal
- Inner Circular
- Serous
Anal Sphincters
- Internal sphincter
- Continuation of circular fibers of the colon. Thus, the internal sphincter is under autonomic control (Autonomic nervous system)
- Involuntary control
- Surrounds upper 3/4 of anal canal
- External sphincter
- Voluntary control
- Surrounds entire length of anal canal
- Consists of three parts – subcutaneous, superficial and deep
Intersphincteric Plane
- Between the external sphincter muscle laterally and the longitudinal muscle (inner sphincteric muscle) medially
- Contains anal glands
- The plance can be opened up surgically to provide access for operations on the sphincter muscles
Anal glands
- Apocrine glands
- Glands are occasionally infected and acts as a source of anal fistula
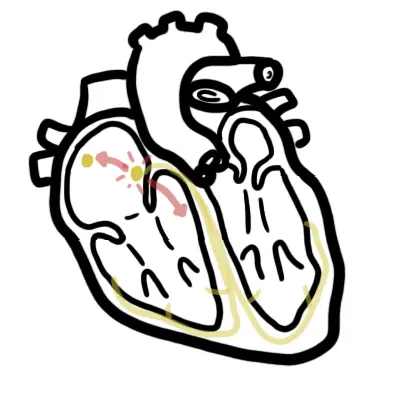
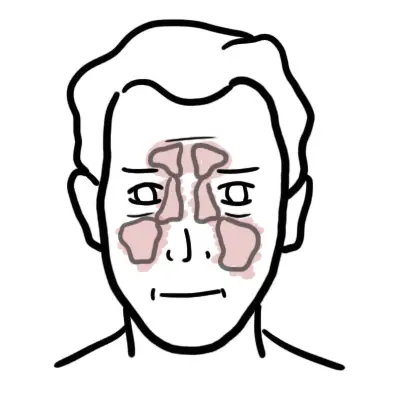
Pectinate line (dentate line)
- Muco-cutaneous junction of anal canal
- Divides anal canal into upper and lower lowers which differ in
- Blood supply
- Lymph drainage
- Nerve supply
- Corresponds with position of anal valves
- Situated at the middle of internal sphincter
| PECTINATE LINE (DENTATE LINE) | ||
| Distinction | Above Pectinate line | Below Pectinate line |
| Embryological origin | Endoderm | Ectoderm |
| Epithelium | Colomnar epithelium | Stratified squamous epithelium |
| Lymph drainage | Internal iliac lymph node | Superficial inguinal lymph nodes |
| Artery | Superior rectal artery | Middle and inferior rectal arteries |
| Veins | Superior rectal veins | Middle and inferior rectal veins |
| Innervation | Inferior hypogastric plexus | Inferior rectal nerve |
| Haemorrhoids | Internal haemorrhoids | External haemorrhoids |
| Hilton’s Line also called while line/anocutaneous line indicates lower end of the internal sphincter. Ischiorectal abscess when communicates with anal canal usually opens at or below Hilton’s line. |
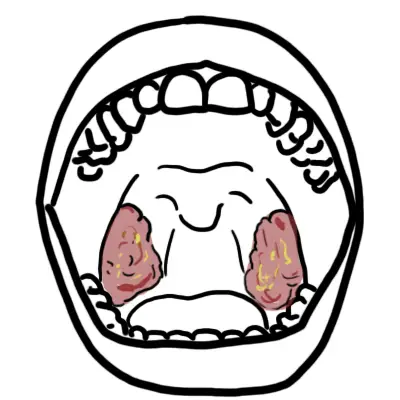
Types
| Internal Haemorrhoid Staging | |
| I | Protudes slightly |
| II | Protrudes during straining and returns back to normal afterwards |
| III | Protrudes out of the anal canal and is reducible |
| IV | Non reducible prolapse |
Internal Haemorrhoid occur above the pectinate line and can prolapse out of the anal canal. This is a late stage and requires surgery.
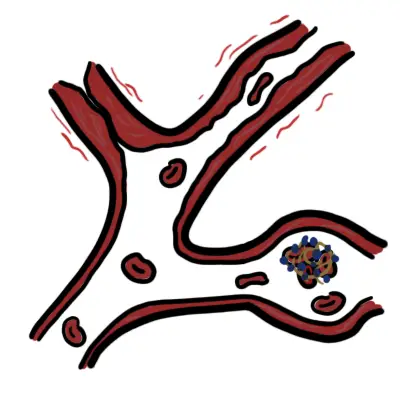
External haemorrhoid occur below the pectinate line and can form thrombus. A thrombosed external haemorrhoid is very painful but self resolves after 2 weeks. They can leave behind skin tags.
Risk Factors

Signs and Symptoms
Patients who present with any symptoms related to the anorectum need to be carefully evaluated to determine the cause. The most common manifestation of hemorrhoids is painless rectal bleeding associated with bowel movement, described by patients as blood drips into toilet bowl.
Internal Haemorrhoids
- Usually not painful even if prolapsed or thrombosed because they occur above the dentate line
- Painless rectal bleeding
- Aching after a bowel movement
- Fullness or discomfort feeling
External Haemorrhoids
- Occur below the dentate line and so causes pain
- Pain on defecation
- Rectal bleeding
- Thrombosed vein (VERY PAINFUL!)
| Think Although external thrombosed haemorrhoids causes severe pain, the presence of severe pain raises the possibility of other conditions, including anal fissure, perirectal or perivaginal infection, abscess, and other inflammatory processes. |
| Remember Commonest age of onset is young adulthood. |
| Remember Typically haemorrhoids occur in the same location as the main anal blood vessels pedicles (described as 3, 7 and 11 o’clock positions as seen in the supine position. |
Differential Diagnosis
More information on clinical presentation of per rectal bleeding.
Investigations
Flexible sigmoidoscopy or colonoscopy may be appropriate if there is concern about the cause of symptoms. During a these procedures, haemorrhoid band ligation and haemorrhoidectomy can be performed.
Diagnosis
Diagnosis is usually by rigid sigmoidoscopy and proctoscopy.
Management
General treatment
- Avoidance of constipation and straining
- Ingest a sufficient amount of insoluble fiber
- Sufficient water to avoid constipation and straining
Medical treatment
- Bulking or softener laxatives
- Sitz bath can be used to clean the butock area.
- Steroid cream – temporary relief of some symptoms
- Pramoxine (anti-itching) – temporary relief of some symptoms
Surgical treatment
- Rubber band ligation – Stage I, II, III
- Photocoagulation – Stage I, II
- Sclerotherapy – Stage I, II
- Haemorrhoidectomy – Stage IV
- Thrombectomy of External Hemorrhoid
| Remember Avoid constipation/straining. Do not give laxatives. Exercise, diet and drink plenty water are good recommendations. |
Complications and Prognosis
Complications
- Anaemia
- Pain
- Heavy bleeding
- Chronic unremitting prolapse of mucosal tissue
- Strangulation
- Ulceration
- Thrombosis
Prognosis External haemorrhoids usually self limiting and patients live with existing lump. Banding is a good treatment option with good outcome.
















Discussion