This section will mainly focus on Autosomal Dominant Polycystic Kidney Disease (ADPKD)
| Watch Video Autosomal Dominant Polycystic Kidney Disease |
Overview
Overview The polycystic kidney diseases are among the most common life-threatening inherited diseases worldwide and frequently cause kidney failure. Autosomal dominant polycystic kidney disease (ADPKD) is seen predominantly in adults, whereas autosomal recessive polycystic kidney disease (ARPKD) is mainly a disease of childhood. For ADPKD, screening asymptomatic at-risk adults with a family history by ultrasound is considered beneficial enabling earlier treatment of complications and to outweigh the risks.
Anatomy and Physiology
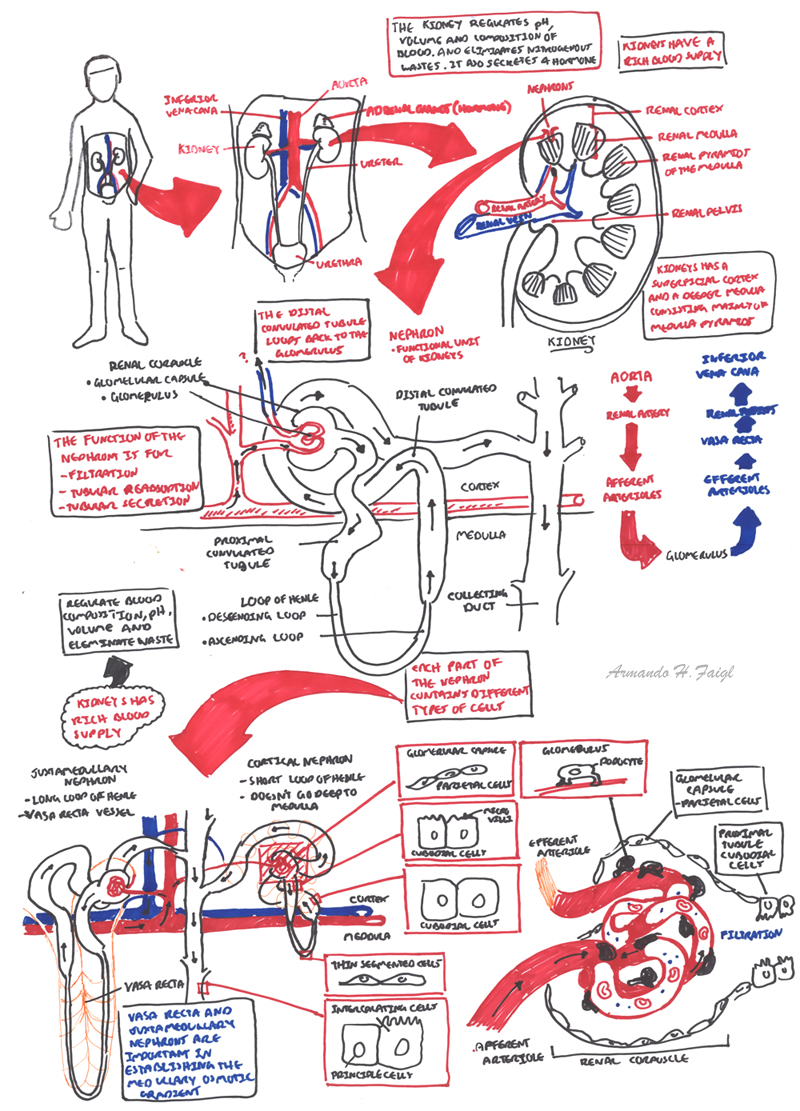
Anatomy The kidneys are retroperitoneal bean shaped organs thats sits between vertebral levels T11-L3. The left kidney sits higher then the right kidney and so the left ureter is longer then the right ureter.
The kidneys is divided into three sections:
- Renal cortex - renal arches and renal columns
- Renal Medulla - pyramids, papillae, major calyx, minor calyx
- Renal Sinus - Pelvis, renal vessels and lymphatics
Arterial Supply
- Aorta → Renal artery (L2) → Segmental artery → Interlobular artery → Cortical radiate artery → Afferent Arteriole → GLOMERULUS
Venous Drainage
- GLOMERULUS → Efferent arteriole (has branches forming the Vasa recta) → Arcuate vein → Interlobar vein → Renal Vein → Inferior vena cava
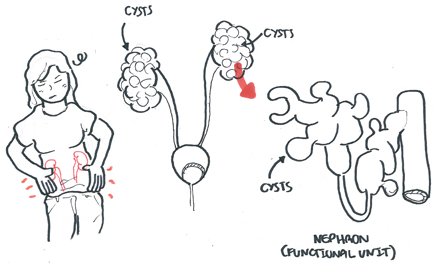
Nephrons
- Functional units of Kidneys
- Nephron's are structurally divided into two types:
- Cortical
- Juxtamedullary
- Nephron is a long tube that is divided into the following sections:
- Bowman's capsule - where the GLOMERULUS sits and filters blood into the nephron
- Proximal convulated tubule
- Loop of Henle
- Distal convulated tubule
- Collecting duct
The collecting ducts then drain into the Minor calyx → Major calyx → Renal pelvis → Ureter → Urinary bladder.
| Watch Video Nephrology Overview |
Physiology of the Kidney
Function:
- Urine formation
- Excretion of waste products
- Regulation of electrolytes
- Regulation of acid-base balance
- Control of water balance
- Control of blood pressure
- Renal clearance
- Regulation of RBD production (through hormone erythropoetin)
- Synthesis of vitamin D to active form
- Secretion of prostagladins
Risk Factors
ADPKD is a inherited kidney disease. It is Autosomal dominant and so the risk of developing ADPKD is 50%. However, some 10-15% of patients diagnosed with ADPKD will report no family history.
| Risk Factors for Progression of ADPKD |
| Genotype |
| Age of end stage renal failure |
| Male |
| Hypertension |
| Urinary tract manifestation before age 35 years |
Signs and Symptoms
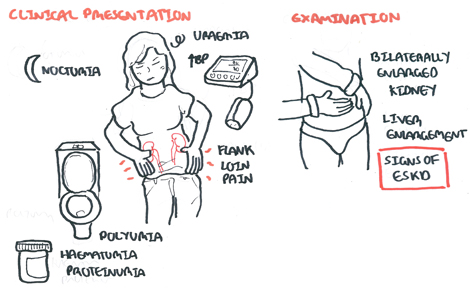
Clinical Presentation
- Flank or loin pain from enlarged or infected cysts
- Nocturia
- Polyuria
- Hypertension
- Proteinuria
- Haematuria
- Uraemic symptoms
| Remember Hypertension is the earliest manifestation of ADPKD and is preferentially managed with ACE inhibitors or ARBs |
Examination
- Bilaterally enlarged kidneys with irregular surfaces
- Enlarged liver with an irregular, lobulated edge
- Signs of end-stage kidney disease
- Hypertension
| Signs of End-stage Kidney Disease |
| Scar in the iliac fossa nad a mass consistent with renal transplant |
| Arteriovenous fistula (haemodialysis) |
| Peritoneal fistula |
| Scar of the neck consistent with parathyroidectomy (renal bone disease) |
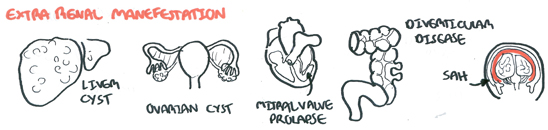
Extra-renal Manifestation
- Liver cysts
- Intra-cranial aneurysm -> Sub Arachnoid Haemorrhage
- Mitral Valve prolapse
- Ovarian cyst
- Diverticular Disease
Differential Diagnosis
Bilateral Renal Enlargement
- Bilateral hydronephrosis
- Amyloidosis
- Ruberous sclerosis
- Von Hippel-Lindau disease
| Von Hippel-Lindau disease is a hereditary condition associated with hemangioblastomas, which are blood vessel tumors of the brain, spinal cord. The disease has an increased risk of developing clear cell renal cell carcinoma and renal cysts. |
Investigation and Diagnosis
- FBC
- EUC
- LFT
- Urinalysis
- MSC
Most often, the diagnosis of ADPKD is made from a positive family history and imaging studies showing large kidneys with multiple bilateral cysts and possibly liver cysts
Diagnosis Imaging criteria of ADPKD in at-risk individuals
| Age | Cyst Count | Imaging |
| 15-39 | >3 (total) | Ultrasound |
| 40-59 | 2 (both kidneys) | Ultrasound |
| >60 | 4 (both kidneys) | Ultrasound |
| 16-40 | >10 (both kidneys) | MRI |
Pathophysiology
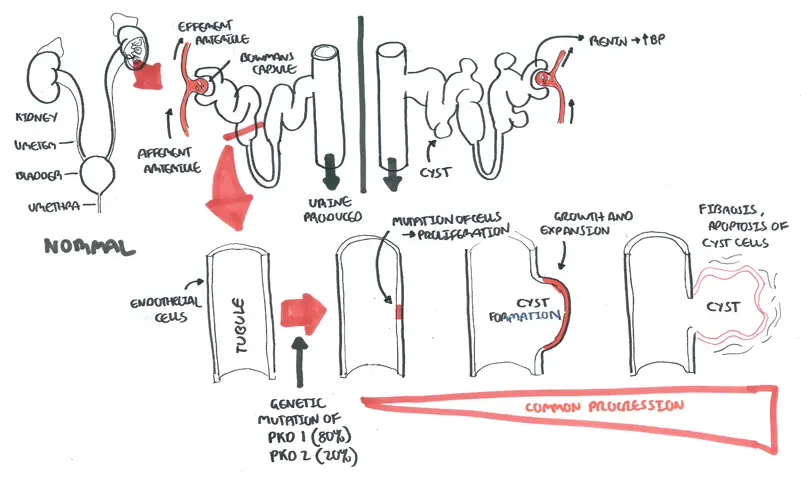
ADPKD is a genetic condition. In 80% of cases there is a PKD1 mutation and PKD2 mutation in 20% of cases. This results in a mutation of cells which grow and proliferate forming cysts. These cysts eventually die and fibrose resulting in scarring and fibrosis of the kidney.
Management
No treatment has been proved to prevent cyst growth or the decline in kidney function.
- General
- Increase water intake, decrease Na+ intake and avoid caffeine
- Monitor EUC
- ACE inhibitors/ARBs - for hypertension (aim <130 systolic)
- Antibiotics - infections
- Dialysis - for end stage kidney disease
- Laproscopic cyst removal
- Tolvaptan
| Pharmacology Tolvaptan is a selective vasopressin (ADH) receptor 2 antagonist. It inhibits the reuptake of water from the distal nephron's and is shown to result in a 50% reduction in the annual rate of kidney growth. |
| Remember avoiding NSAIDs is advised for people with polycystic kidney disease as this drug is a nephrotoxin |
Complications and Prognosis
Complications
- Urinary Tract Infection
- Hypertension
- Chronic Kidney Disease
- Cyst Haemorrhage
- Cyst infection
- Nephrolithiasis
- Subarachnoid haemorrhage
Prognosis
Psychological impact of ADPKD - 60% experience anxiety and depression
Autosomal Recessive Polycystic Kidney Disease
Overview ARPKD is primarily a disease of infants and children. The incidence is 1:20,000 births. The kidneys are enlarged, with small cysts, <5 mm, limited to the collecting tubules.
Clinical Features
- ~50% of affected neonates die of pulmonary hypoplasia, the result of oligohydramnios from severe intrauterine kidney disease.
- ~80% of those who survive the neonatal period are still alive after 10 years
- One-third will have developed end stage renal disease.
- Enlarged kidneys may be detected soon after birth as bilateral abdominal masses
- Impaired urinary concentrating ability and metabolic acidosis ensue as tubular function deteriorates.
- Hypertension often occurs in the first few years of life.
- Kidney function deteriorates progressively from childhood into early adult life.
- Longer-term survivors frequently develop complications of portal hypertension from periportal fibrosis.
Diagnosis Ultrasonography reveals large, echogenic kidneys. The diagnosis can be made in utero after 24 weeks of gestation in severe cases, but cysts generally become visible only after birth.